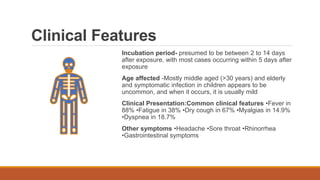
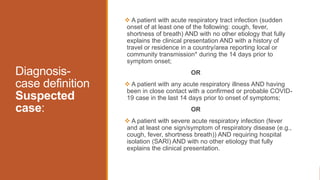
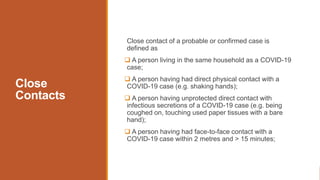
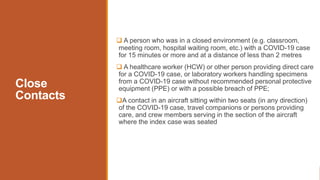
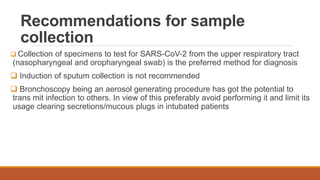
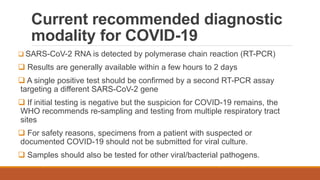
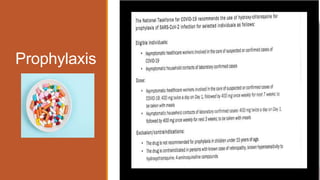
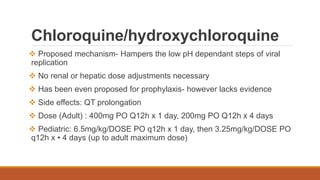
This document provides information on COVID-19, including that it is caused by a coronavirus that commonly infects humans and animals. The virus spreads mainly through respiratory droplets from coughing or sneezing. Most cases are mild, but some develop severe pneumonia requiring hospitalization. Diagnosis is via PCR testing of respiratory samples. While there is no vaccine, potential treatments include chloroquine and supportive care. Public health measures aim to test, isolate cases and trace contacts to control spread.