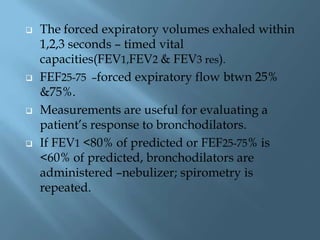
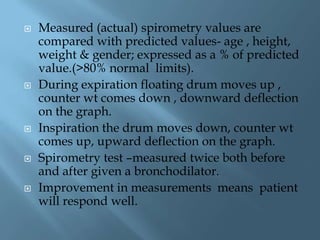
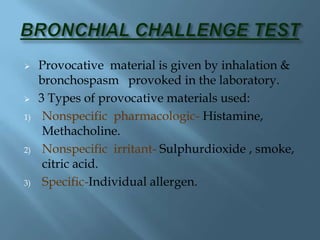
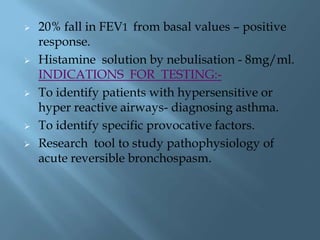
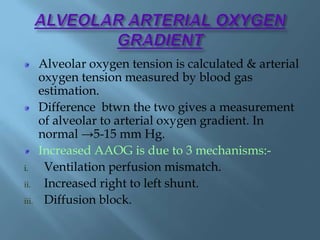
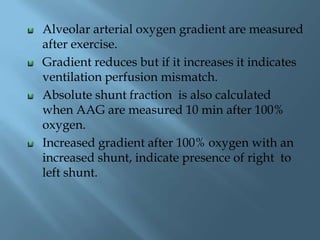
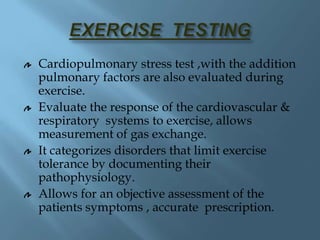
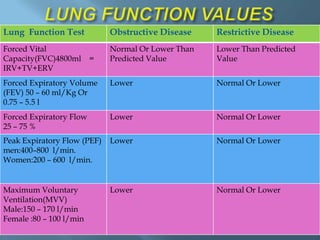
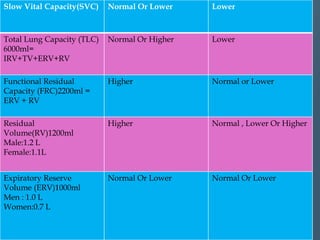
This document discusses various pulmonary function tests used to evaluate lung function. It describes tests such as spirometry, which measures volumes of air inhaled and exhaled over time producing a spirogram. Static lung volumes like total lung capacity and functional residual capacity are also discussed. Other tests mentioned include bronchial provocation tests to identify hypersensitive airways, measurement of carbon monoxide diffusing capacity, and exercise testing to evaluate cardiopulmonary response to exertion. The document provides details on procedures and clinical applications of these pulmonary function tests.