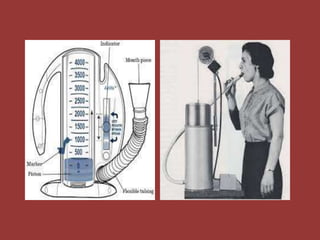
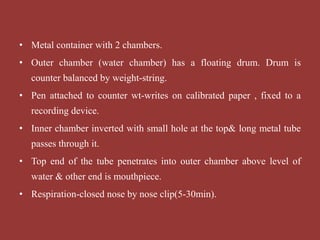
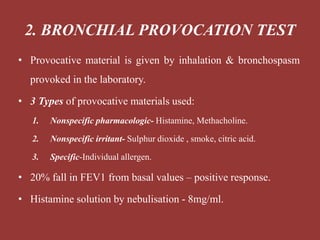
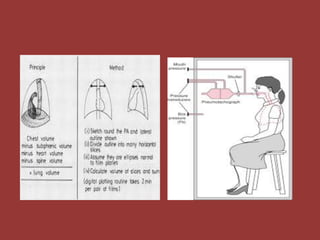
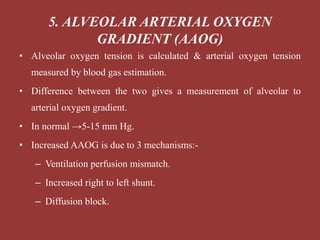
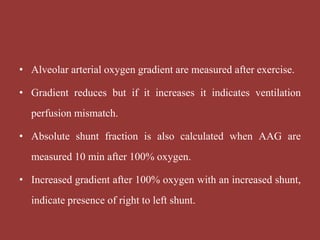
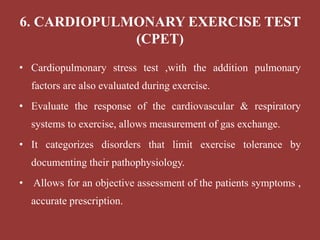
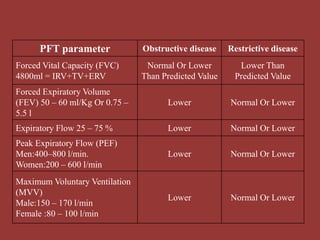
This document discusses pulmonary function tests (PFTs), which assess lung function by measuring various parameters including tidal volume, vital capacity, and gas exchange. PFTs can detect and quantify respiratory disease, evaluate disease progression and response to therapy. The document describes several PFT techniques including spirometry, which measures volumes of air inhaled and exhaled; static lung volumes; diffusing capacity tests; and exercise testing. It provides indications for each test and discusses abnormal findings in obstructive and restrictive lung diseases.