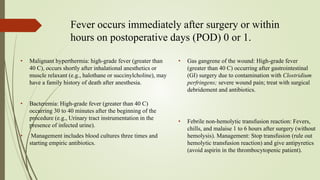
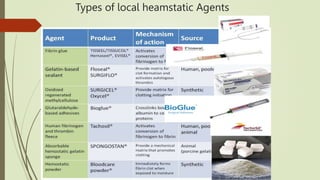
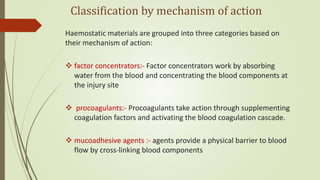
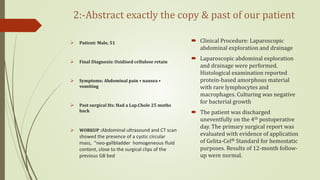
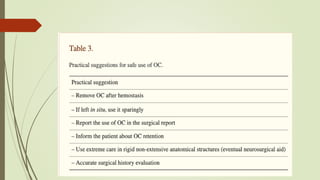
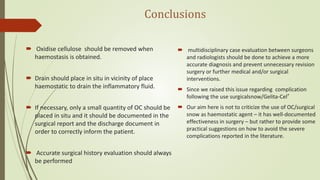
This document discusses a case of postoperative fever of unknown origin in a young patient following laparoscopic cholecystectomy. Standard workups did not reveal a cause. The case is presented at a morbidity meeting to discuss potential causes. The sequential surgical management of the patient involving ERCP and cholecystectomy is reviewed. Common and uncommon causes of postoperative fever are discussed. The pathophysiology and definitions of fever are reviewed. Different types of local hemostatic agents used in surgery and their mechanisms of action are described. Finally, the literature is reviewed to find a similar case where retained oxidized cellulose used as a hemostatic agent during a prior surgery was found to be the cause of fever in this patient.