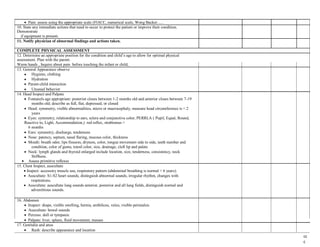
This document provides guidelines for students to follow when conducting a pediatric physical assessment. It outlines 21 steps for the assessment, including preparing equipment, introducing oneself to the patient, performing a rapid initial assessment, taking vital signs, conducting a full physical exam of different body systems, and documenting findings. The assessment is to be performed on an infant or child patient under the supervision of an instructor, with the goal of informing the physician of any abnormal findings and planning appropriate care.