Description:
In this comprehensive and insightful presentation, we explore the critical role of hospital formularies in ensuring optimal patient care and cost-effective medication management. A hospital formulary is a carefully curated list of medications approved for use within a hospital, serving as a guiding resource for prescribing, dispensing, and administering drugs. It plays an indispensable role in enhancing patient safety, reducing medication errors, and ensuring that treatments adhere to the highest standards of clinical practice.
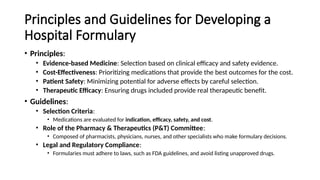
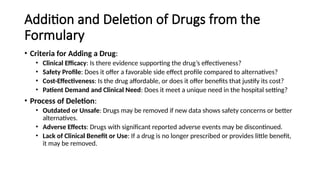
This presentation delves deep into the formulation, management, and impact of hospital formularies, highlighting their significance in optimizing therapeutic outcomes while minimizing unnecessary healthcare expenses. With a focus on evidence-based practices and the collaboration of multidisciplinary healthcare teams, it provides valuable insights into the processes that shape formulary decisions, including drug efficacy, cost-effectiveness, and patient-centered care.
The Hospital Formulary also serves as an essential tool for pharmacists, clinicians, and healthcare administrators, offering a structured approach to drug selection, inventory control, and therapeutic guidelines. By understanding the complexities of formulary management, healthcare professionals can streamline medication use, minimize therapeutic duplication, and ensure that patients receive the most appropriate and affordable medications for their conditions.
Throughout this presentation, you'll gain a clear understanding of how formulary committees make informed decisions, and how these decisions influence both patient outcomes and hospital operations. Whether you're a healthcare professional looking to improve your knowledge or someone interested in understanding the critical role of medication management in hospitals, this presentation provides a wealth of information and practical strategies.
Key Takeaways:
The strategic importance of a well-maintained hospital formulary.
How formulary decisions impact patient safety and clinical outcomes.
The relationship between formularies, cost containment, and medication efficacy.
Practical tips for improving formulary processes and ensuring patient-centered care.
With the increasing complexities of modern medicine, understanding the Hospital Formulary system is crucial to improving healthcare delivery, patient satisfaction, and long-term clinical success. This presentation offers a roadmap for enhancing the formulary system to meet the evolving needs of healthcare institutions, ensuring that patients receive the best possible care at an affordable cost.
Tags: Hospital Formulary, Medication Management, Evidence-Based Medicine, Healthcare Cost Containment, Pharmaceutical Care, Clinical Pharmacy, Drug Selection, Formulary Committee, Patient Safety, Therapeutic Guidelines, Drug Cost-Effectiveness, Healthcare Administration, Pharmacy Practice, Medication Errors, Hospital Administration, Healthcare