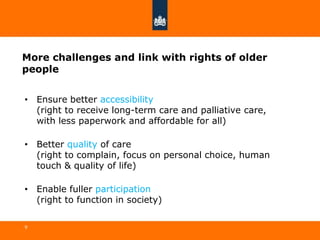
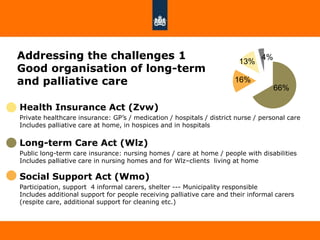
The document discusses recent developments in long-term care and palliative care in the Netherlands. It addresses the challenges of an aging population by outlining the country's organized system of long-term care, which integrates palliative care and offers good social protection against long-term care costs. Additional policy programs have also been implemented to better meet the needs of older people and improve various aspects of care, such as the National Program for Palliative Care and initiatives focused on nursing homes and combating loneliness.