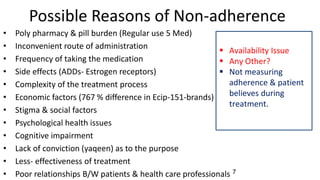
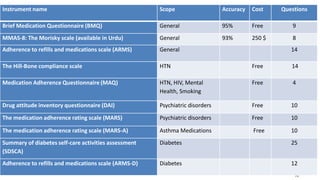
The document discusses medication non-compliance and various ways to measure it. It notes that 50-75% of chronically ill patients do not take their medication as prescribed. Several validated questionnaires are available to measure adherence, including the Morisky Medication Adherence Scale (MMAS-8) and the General Medication Adherence Scale (GMAS). Measuring adherence through questionnaires, pill counts, pharmacy records, and biomarkers can help healthcare providers understand reasons for non-compliance and address them to improve treatment outcomes.