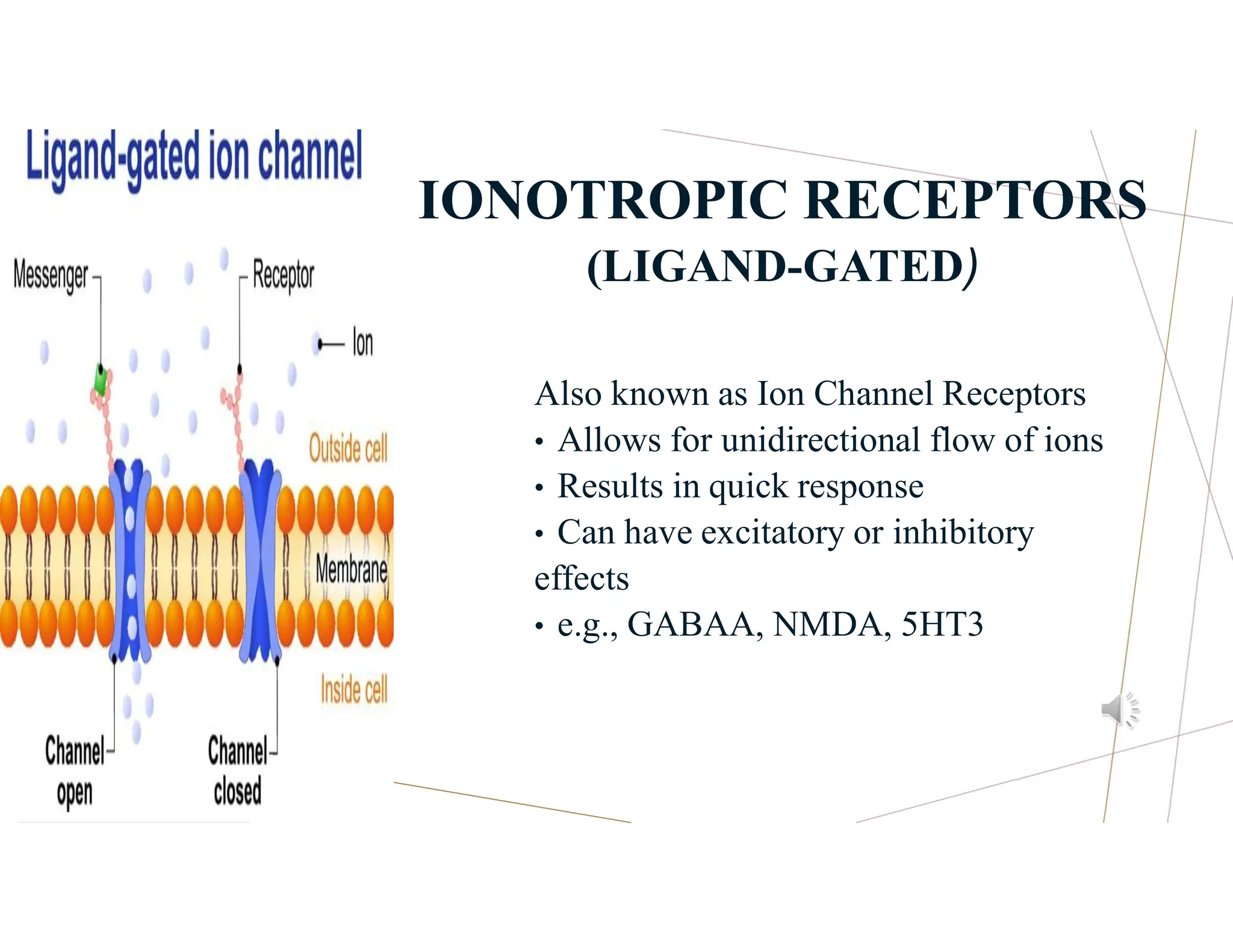
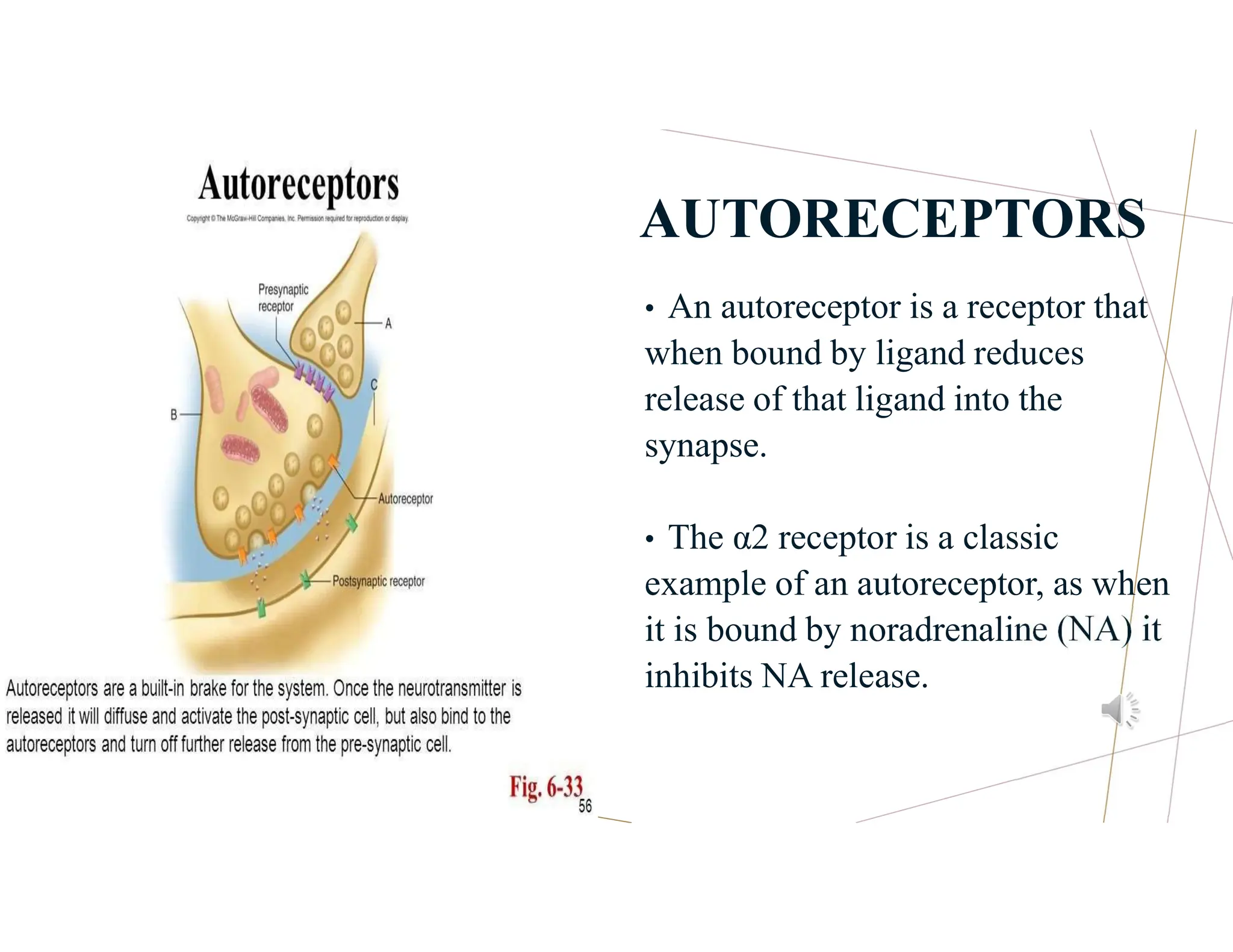
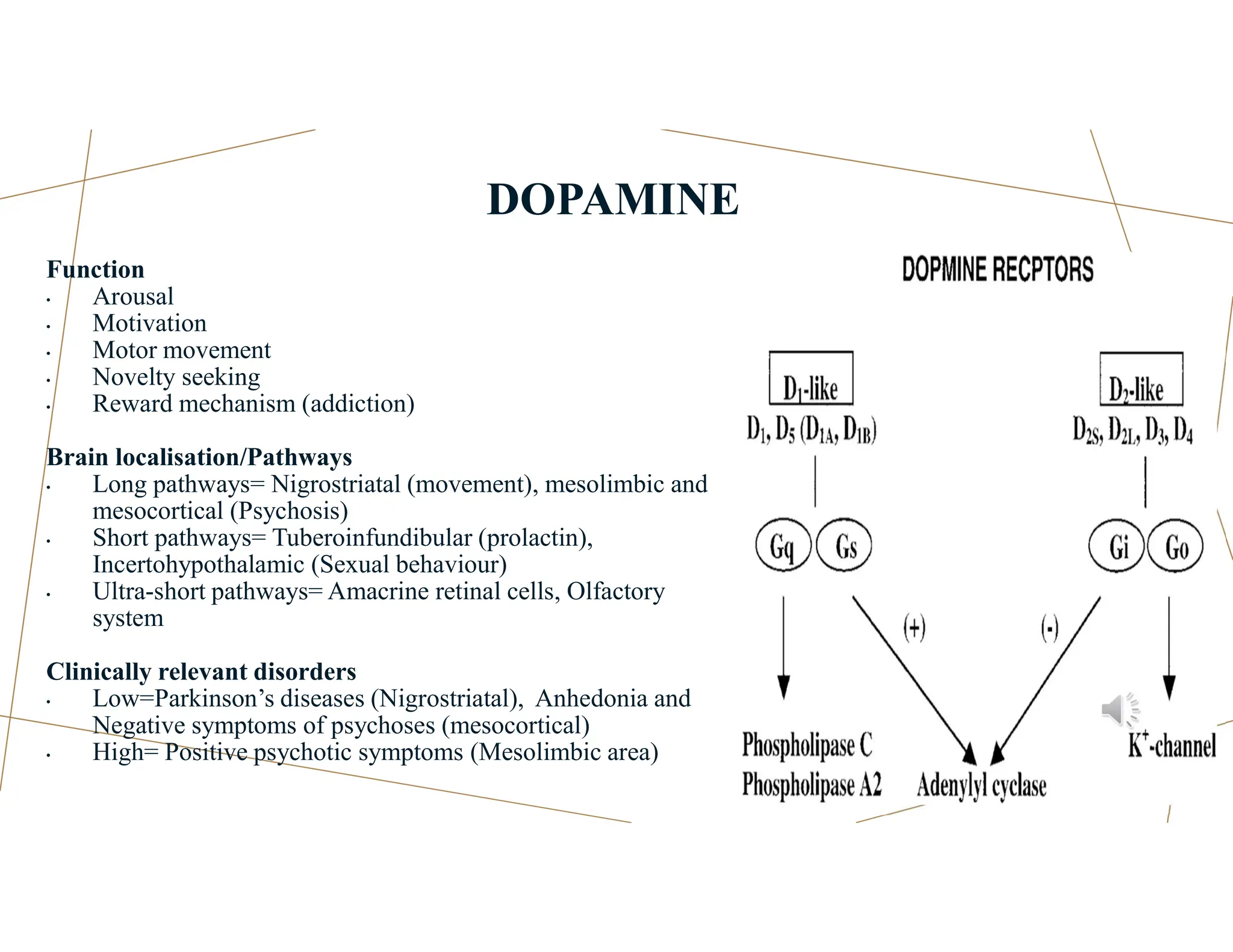
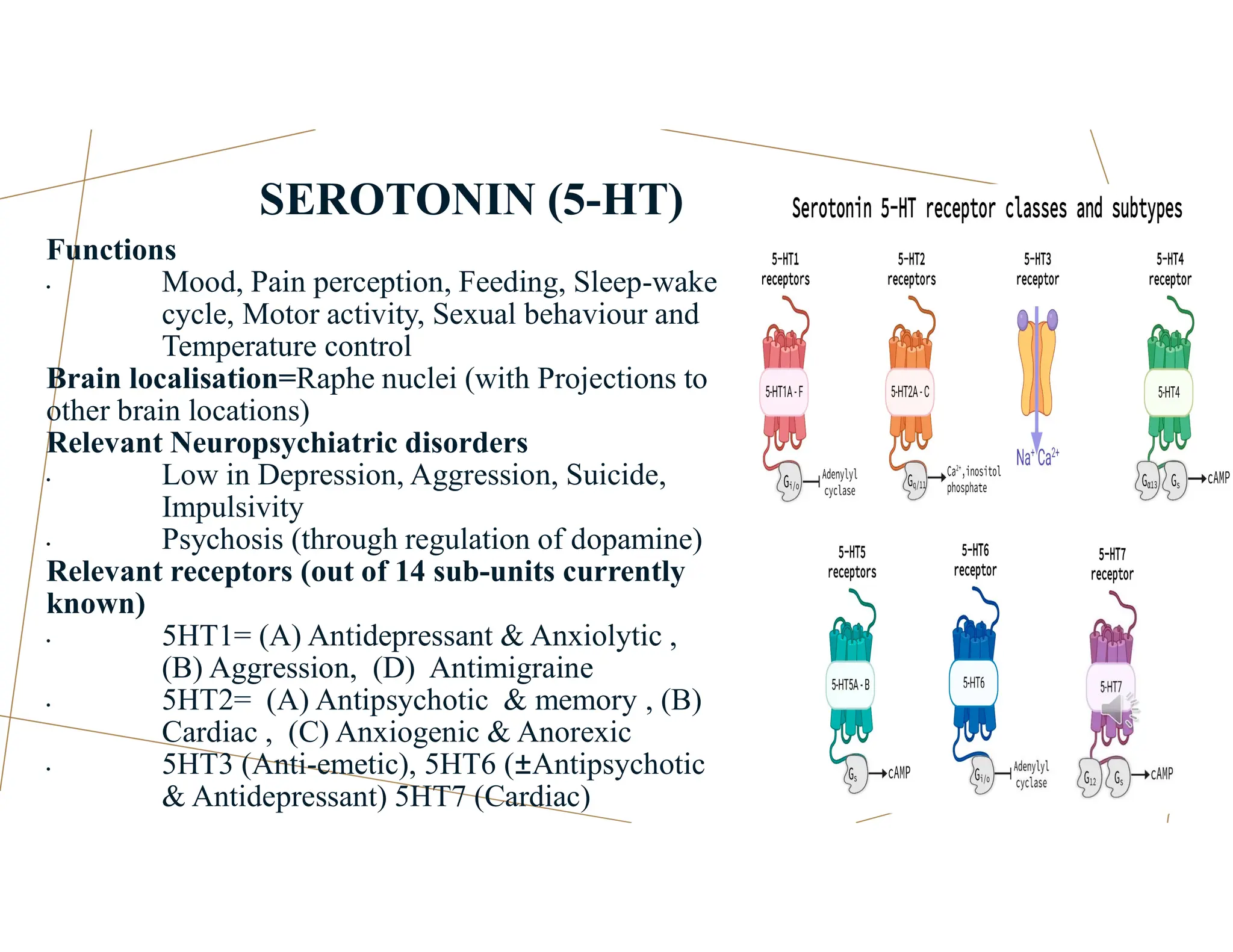
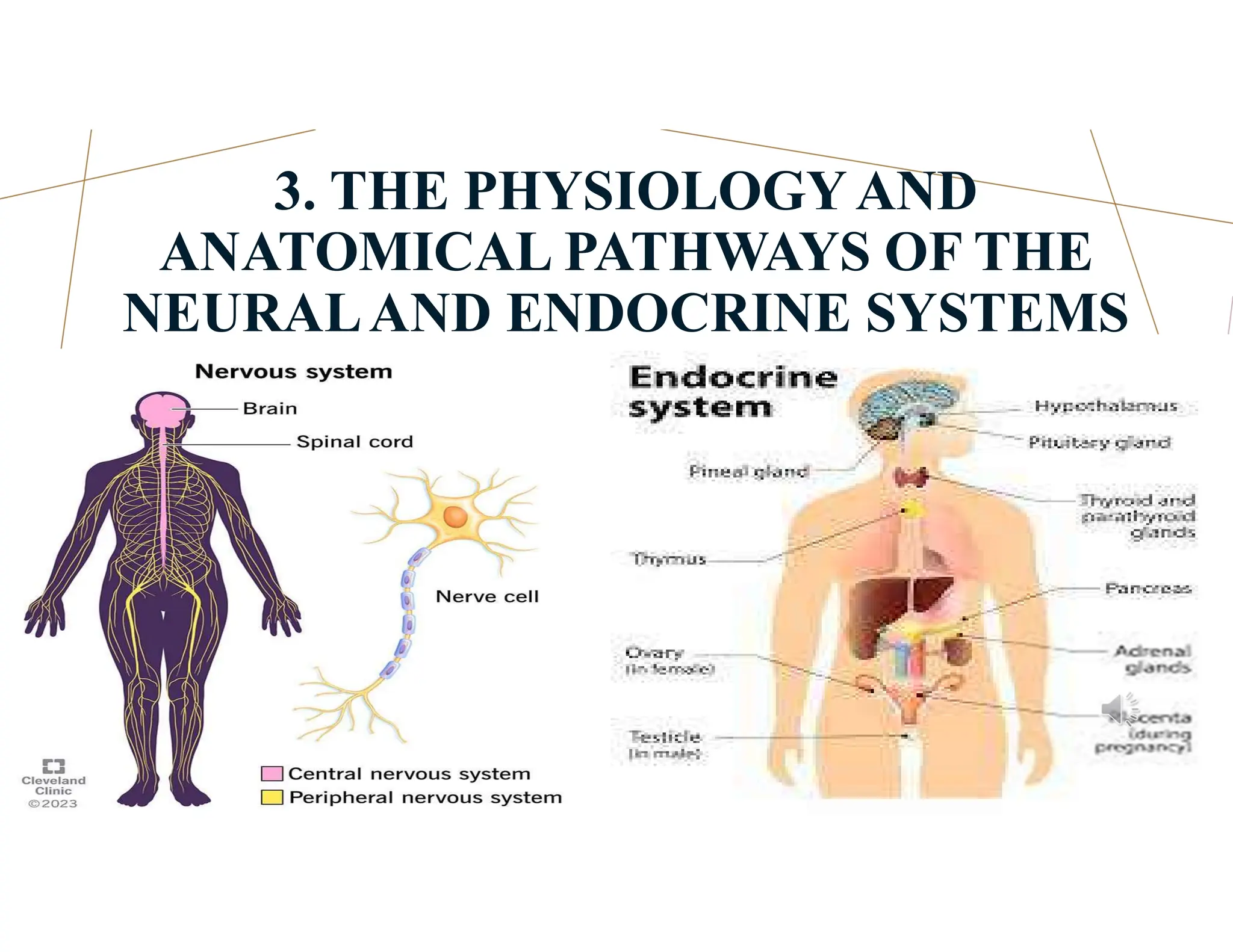
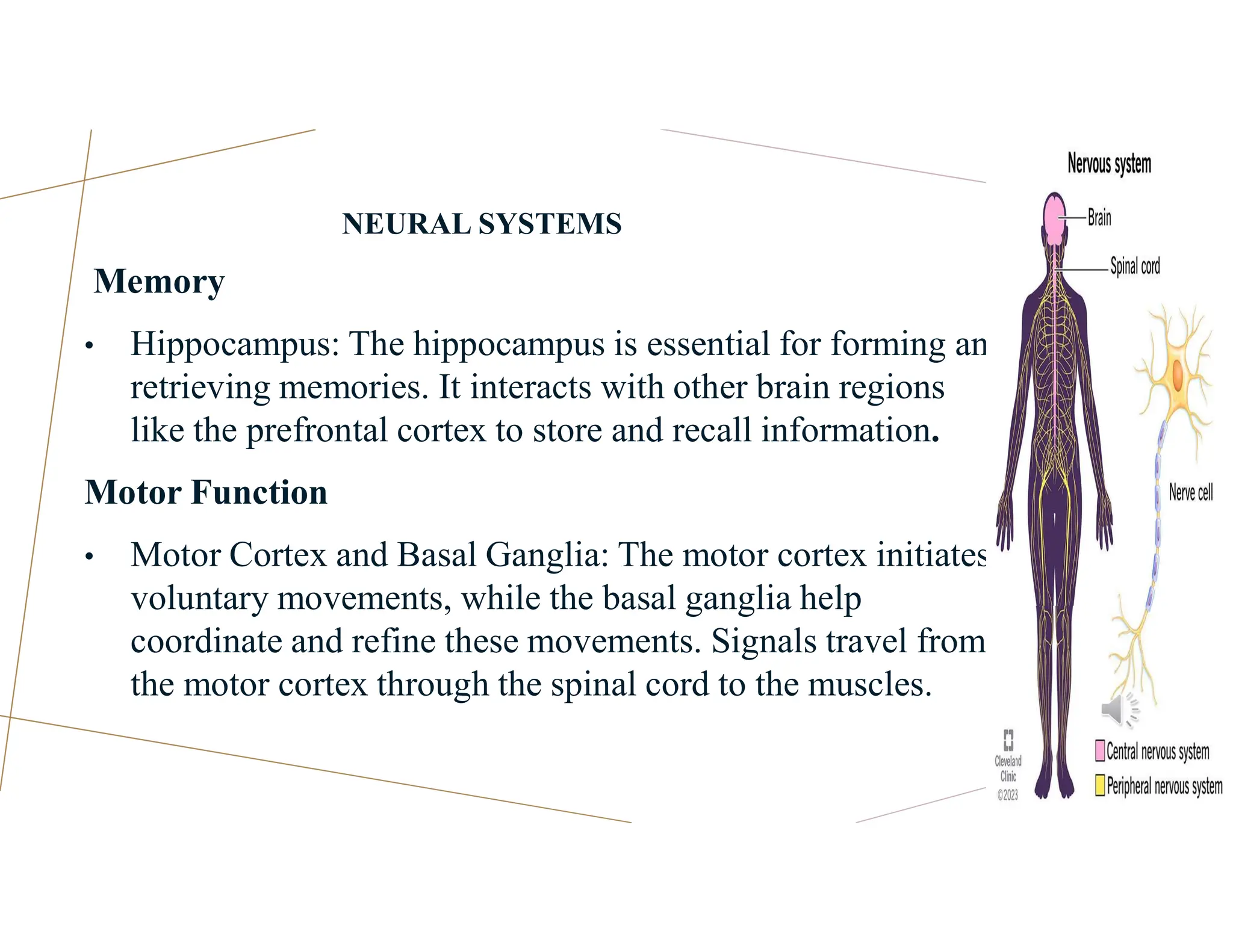
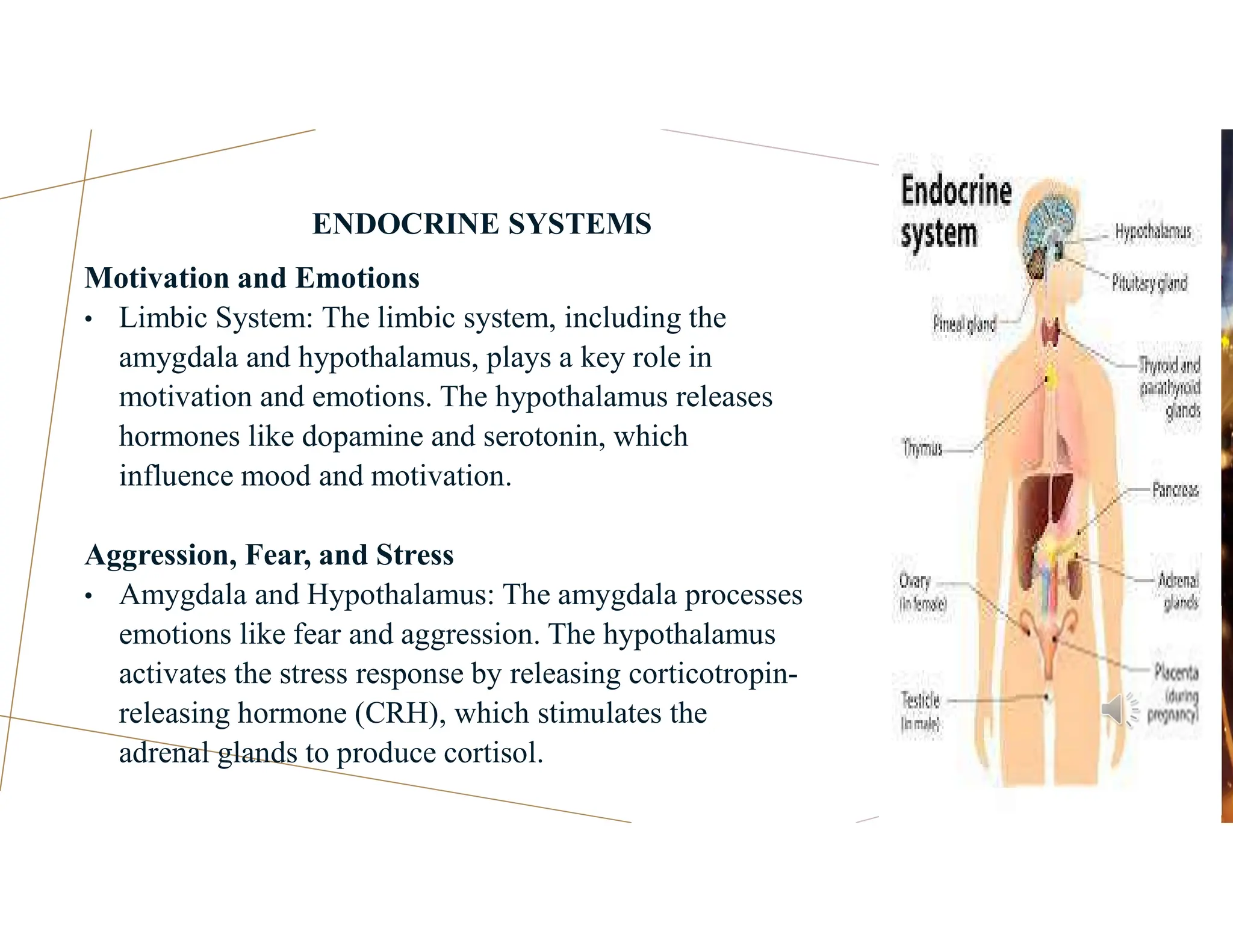
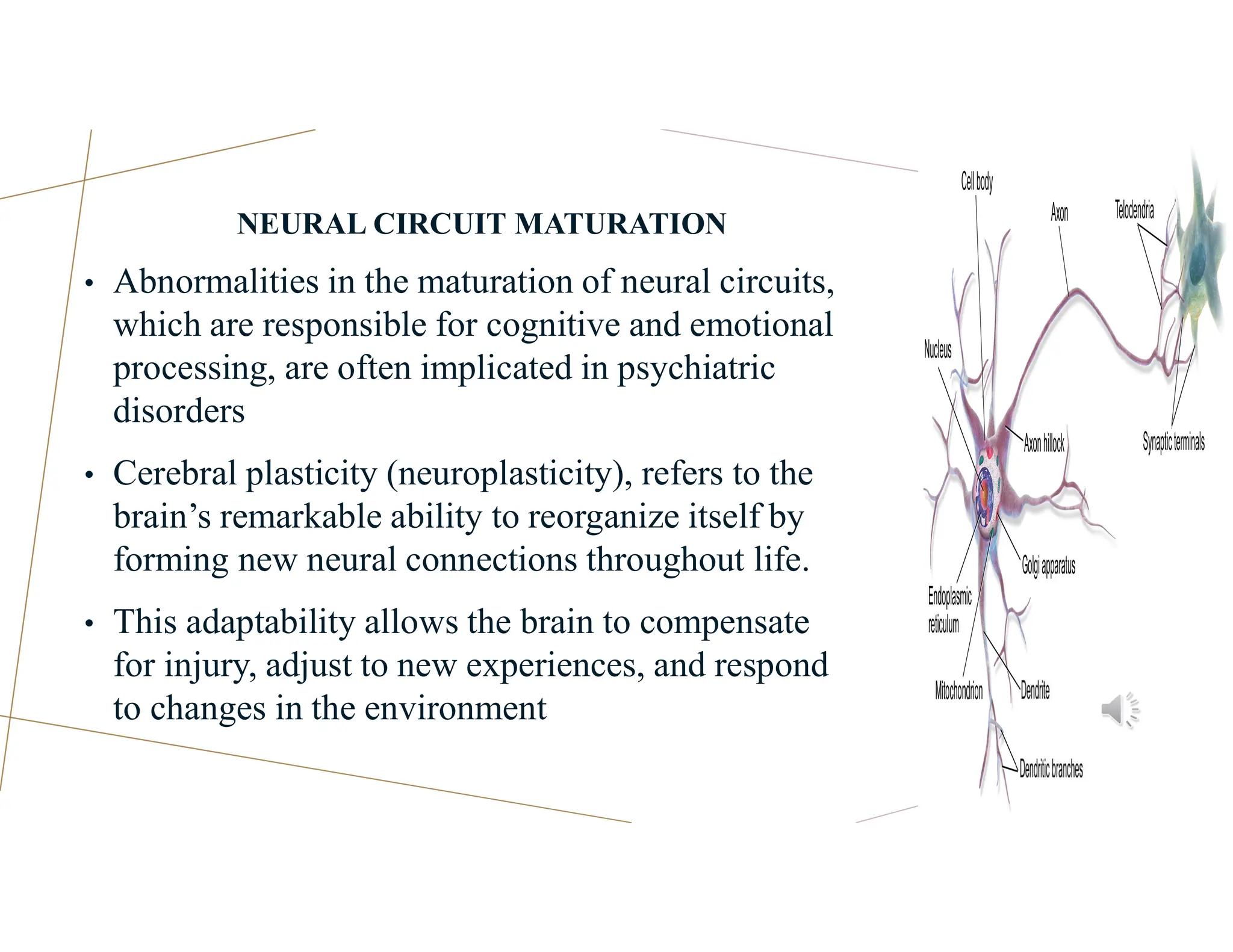
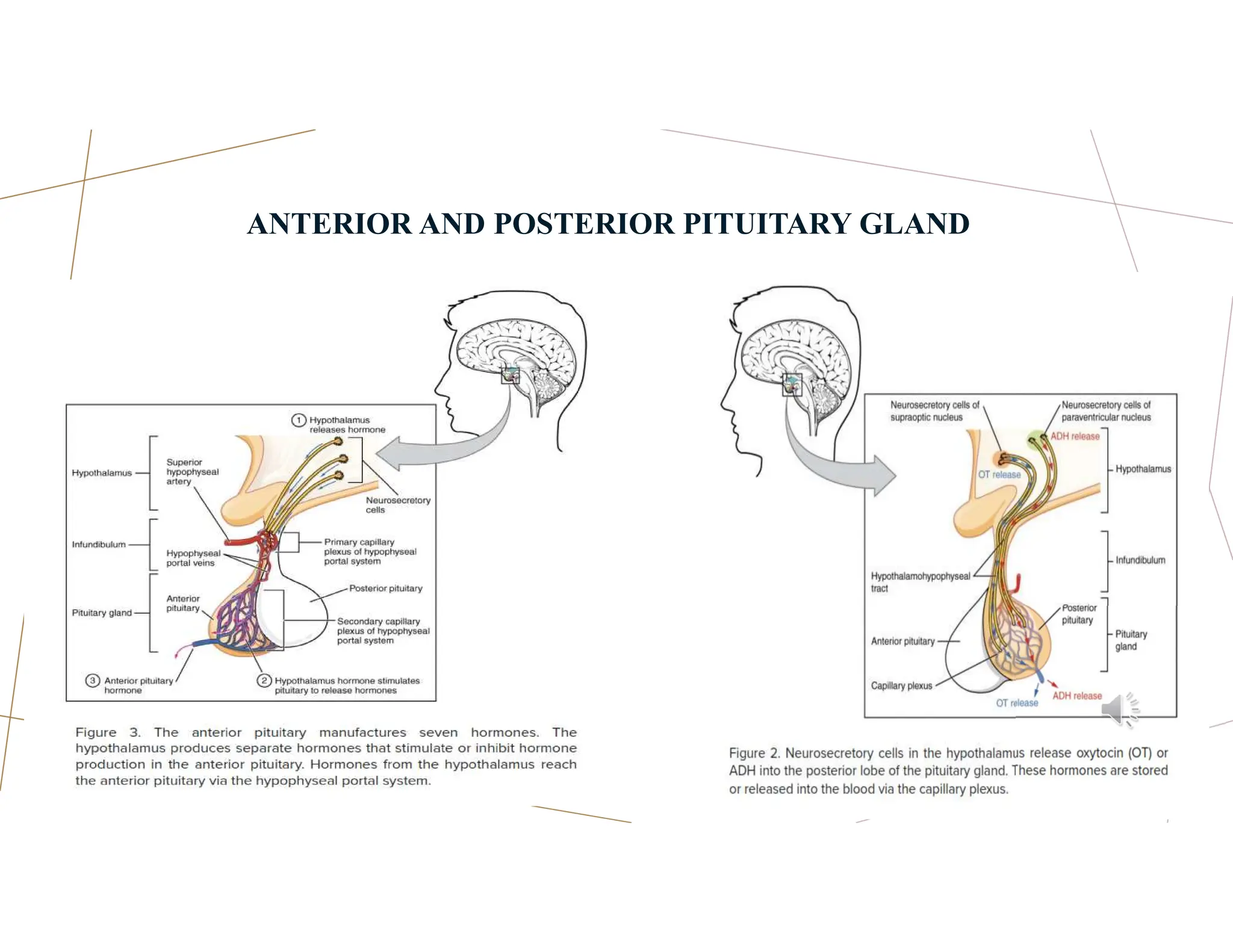
The document discusses neurophysiological processes, focusing on neuron physiology, resting and action potentials, and the neural and endocrine systems' pathways. It emphasizes the neurodevelopmental model of psychiatric disorders and cerebral plasticity, along with the importance of neurotransmitters in mental health. Additionally, it details the integration of neural and endocrine functions in regulating behaviors and overall homeostasis.