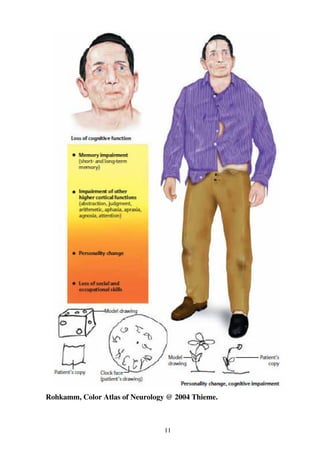
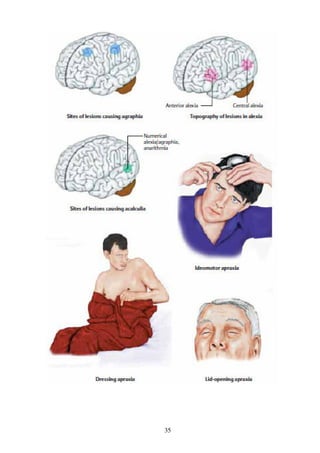
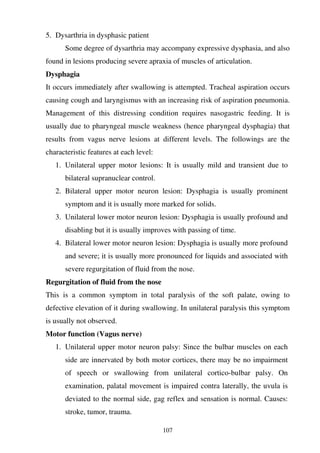
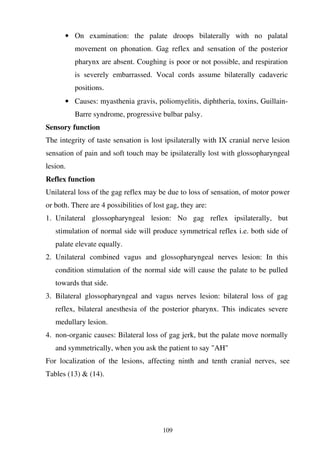
This document discusses examination of higher cerebral functions including level of consciousness, memory, orientation, judgement, reasoning, language, sensory functions, and motor functions. It provides details on testing various levels of consciousness from normal to impaired states like drowsiness, stupor, and coma. Memory is assessed using tests of immediate recall, recent memory, and remote memory. Related topics like persistent vegetative state, locked-in syndrome, and psychogenic unresponsiveness are also covered.