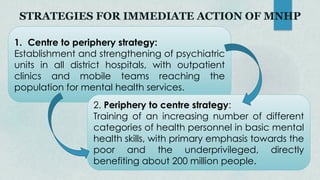
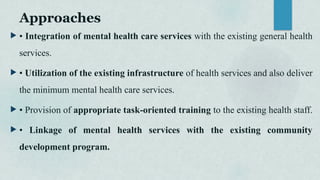
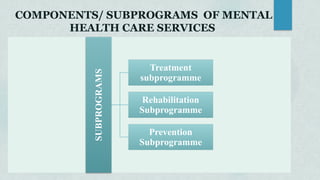
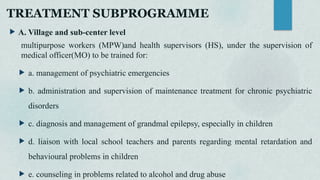
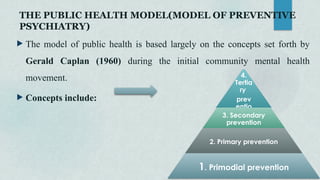
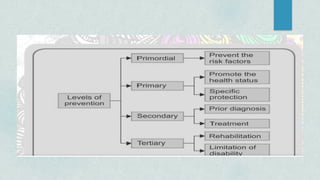
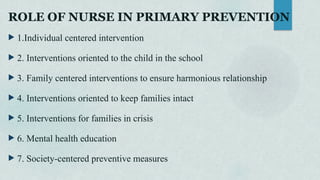
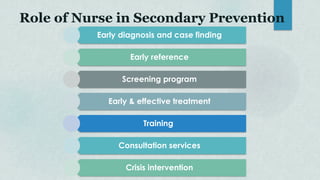
The document outlines the National Mental Health Program of India, launched in 1982, aimed at ensuring access to mental healthcare for vulnerable populations while integrating mental health services with general healthcare. It emphasizes prevention, treatment, and rehabilitation of mental disorders through community participation, training of health personnel, and establishment of mental health facilities. Various preventive measures and treatment strategies, including individual-centered interventions and community engagement, are discussed to enhance mental health awareness and support systems.