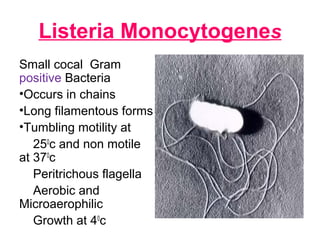
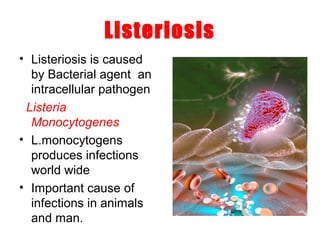
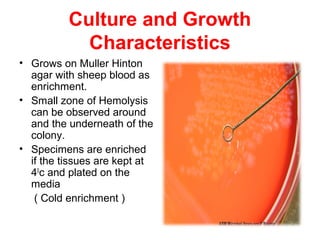
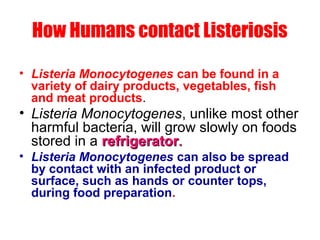
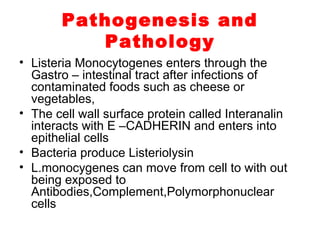
This document discusses Listeria monocytogenes, the bacterium that causes listeriosis. It affects pregnant women, newborns, elderly and immunocompromised individuals. The disease is contracted by eating contaminated food and has flu-like symptoms initially. It can later cause meningitis in newborns. Treatment involves antibiotics like ampicillin. Pregnant women are advised to avoid foods like hot dogs, soft cheeses and deli meats to prevent listeriosis.