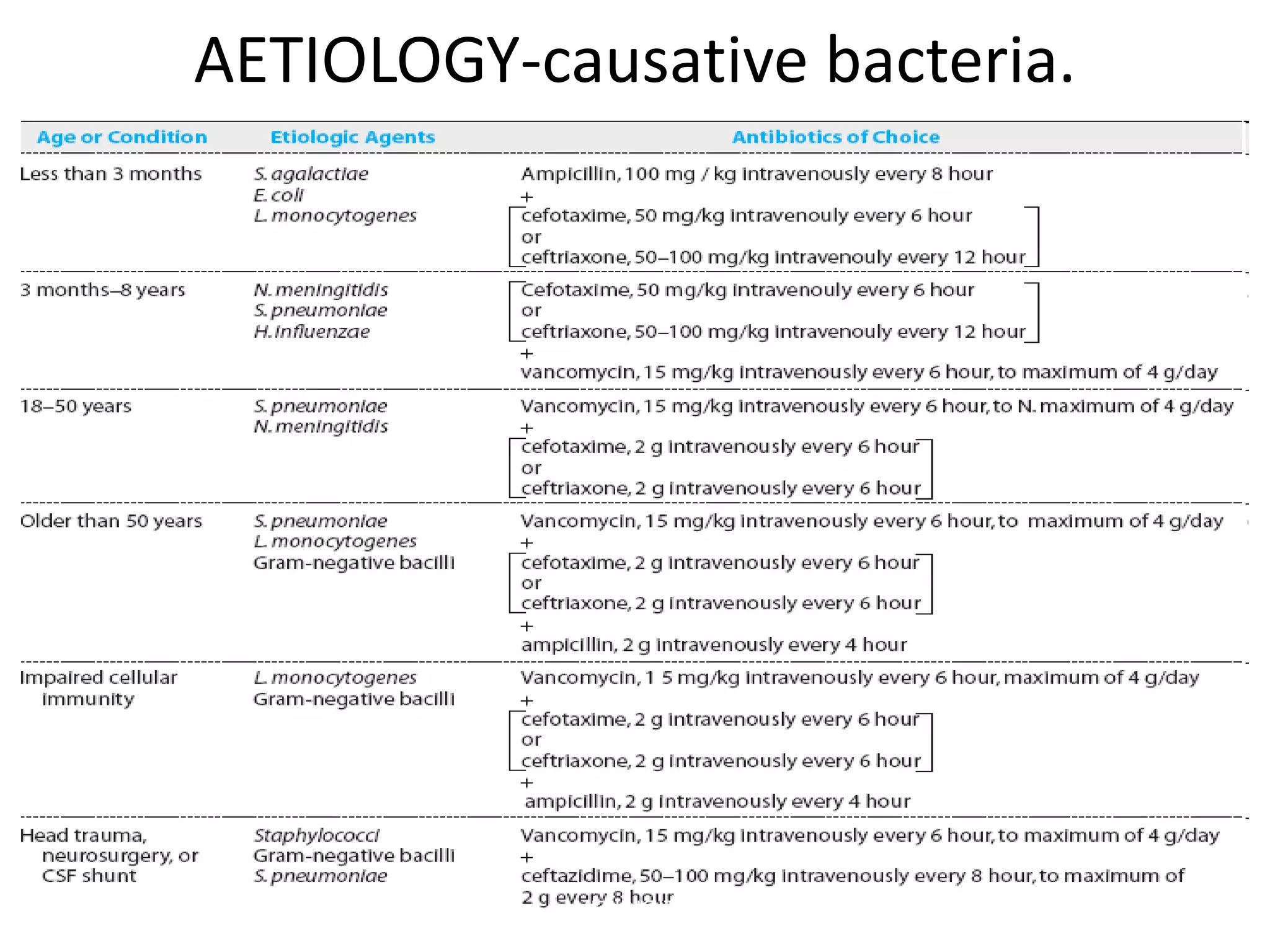
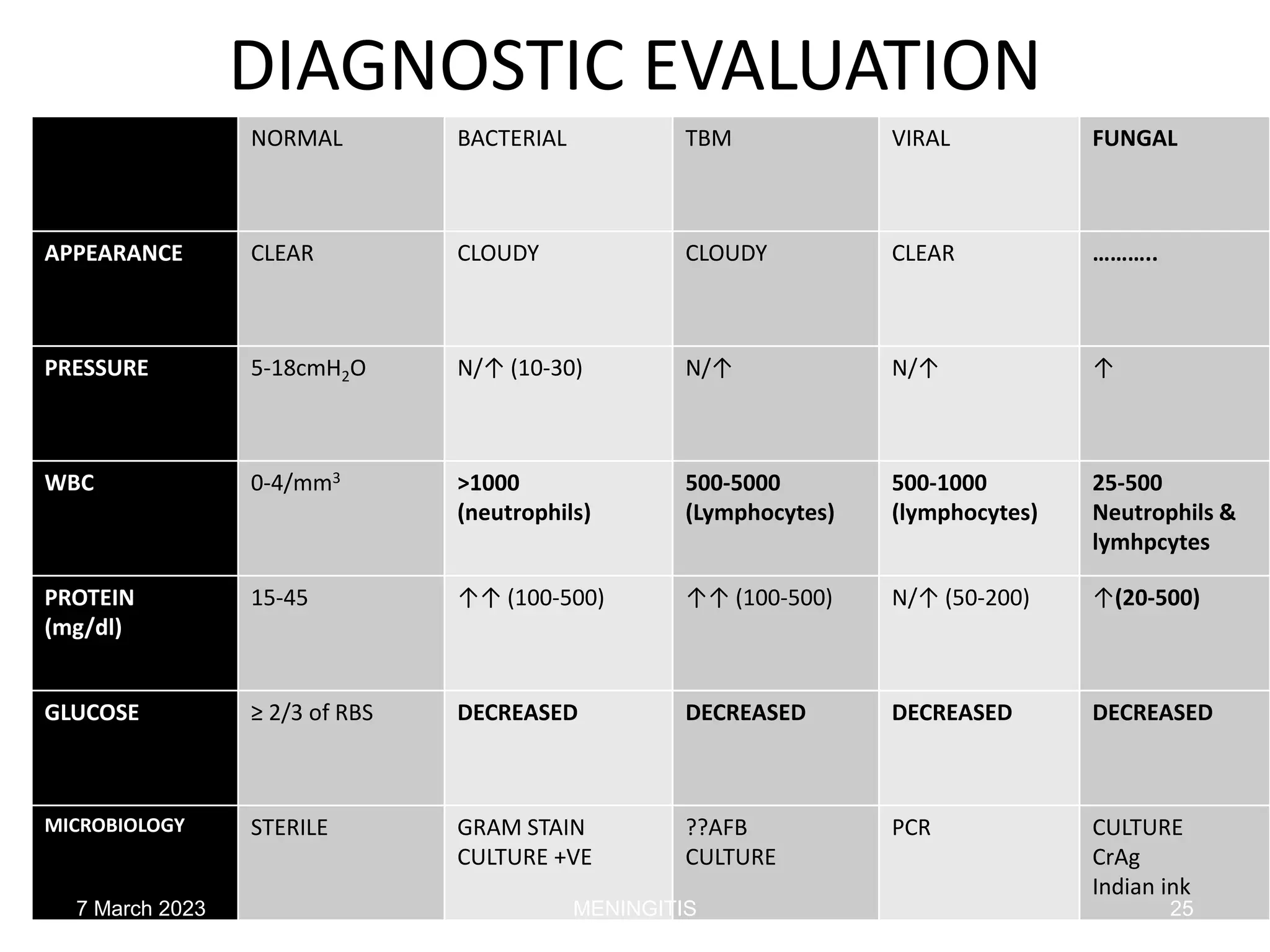
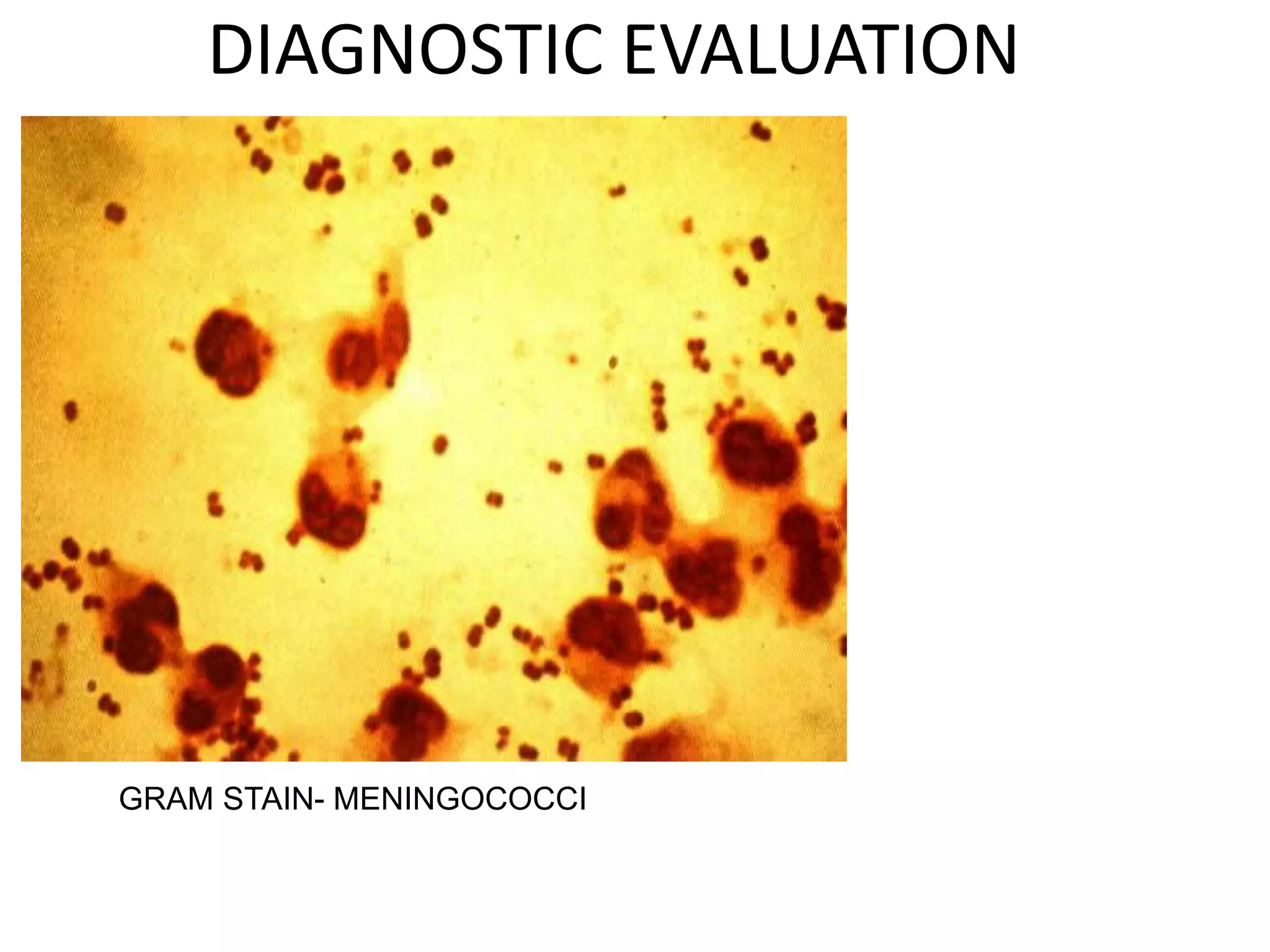
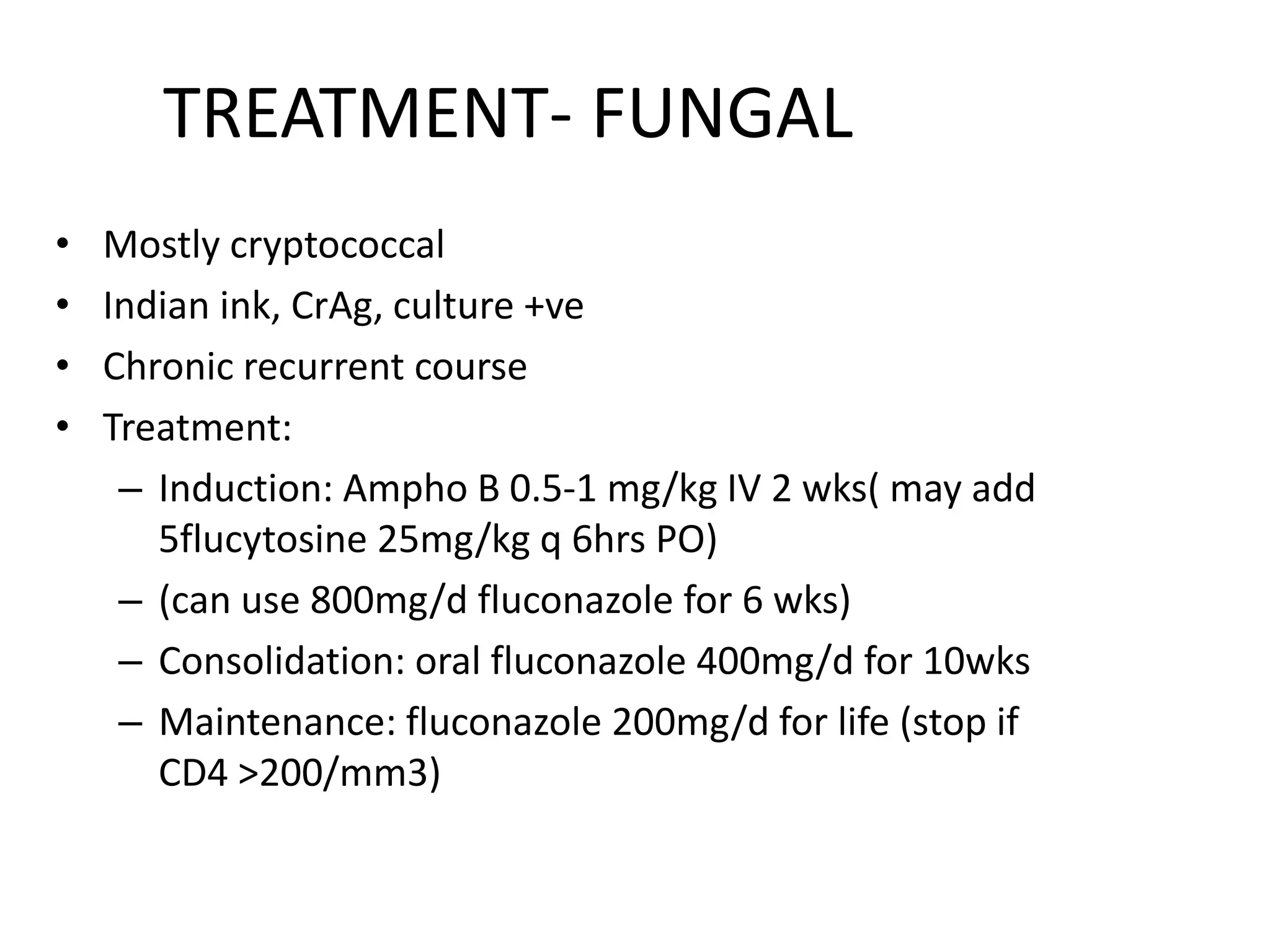
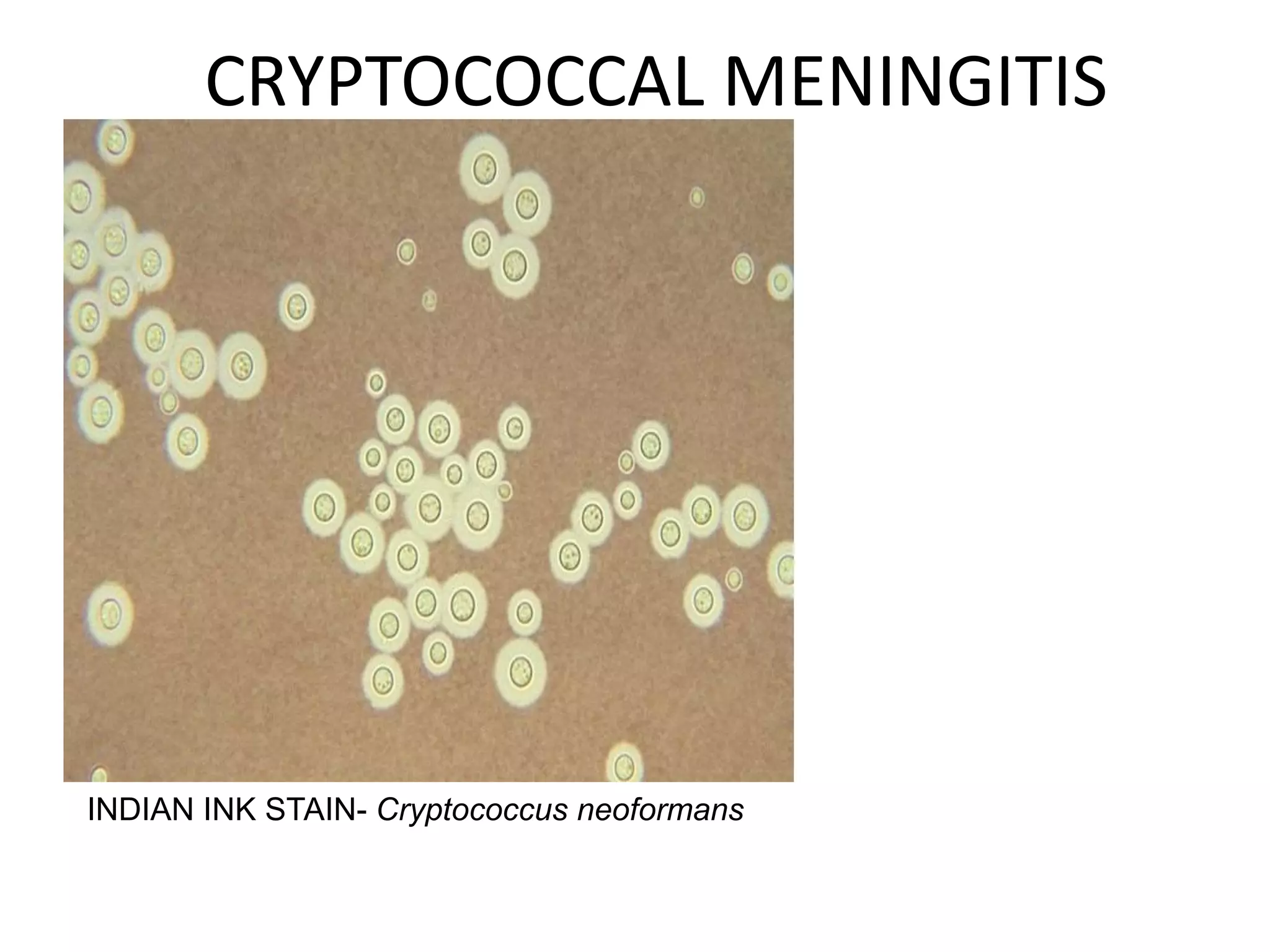
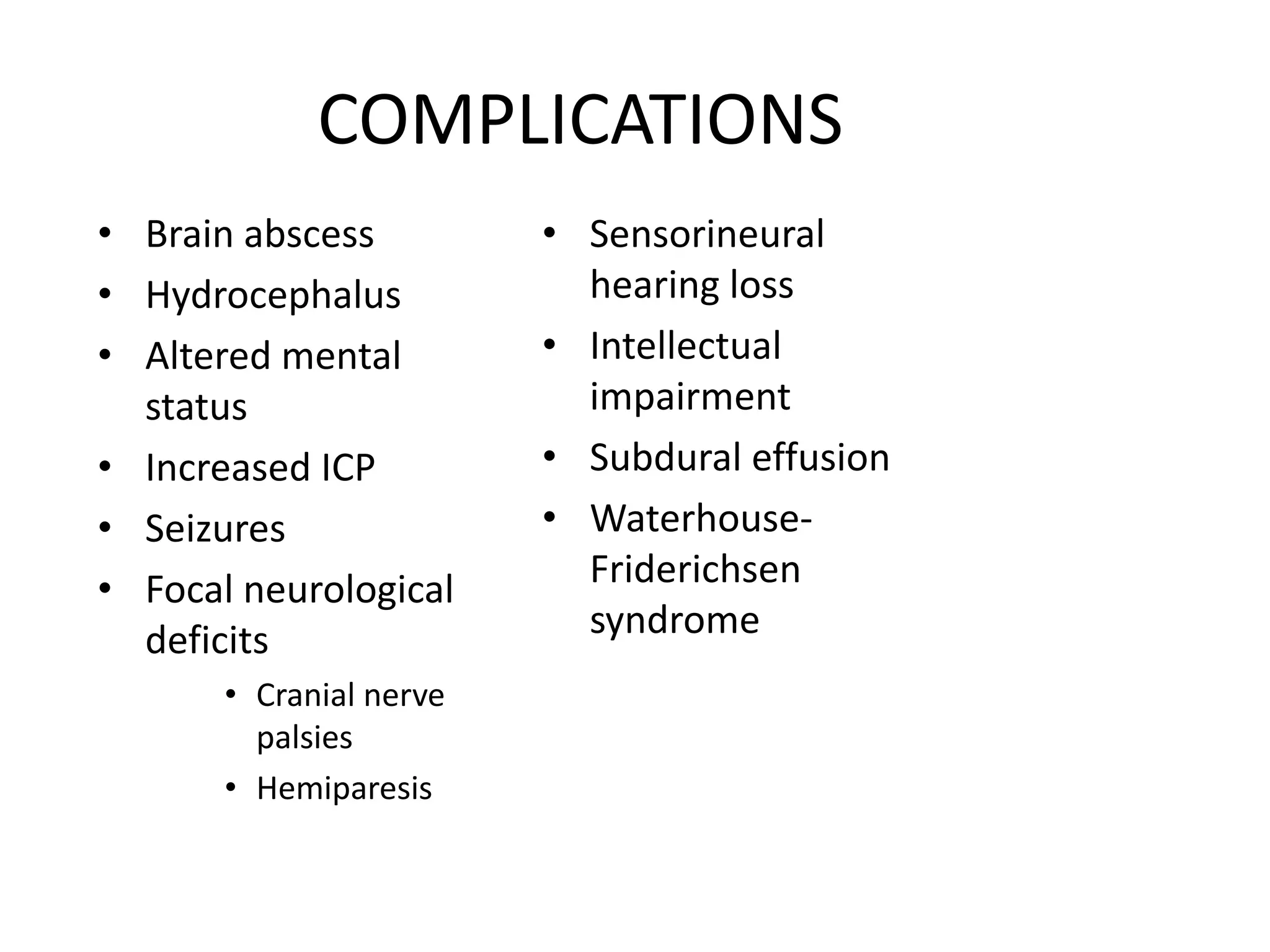
Meningitis is an inflammation of the meninges that can be caused by bacterial, viral, fungal or non-infectious etiologies. The most common bacterial causes are Streptococcus pneumoniae, Neisseria meningitidis, and group B streptococci. Clinical presentation includes fever, headache, neck stiffness, and altered mental status. Diagnosis involves examination of cerebrospinal fluid which shows pleocytosis and elevated proteins. Treatment depends on the identified cause but commonly includes antibiotics and steroids. Complications can include brain abscesses, hydrocephalus, and neurological deficits if not treated promptly.