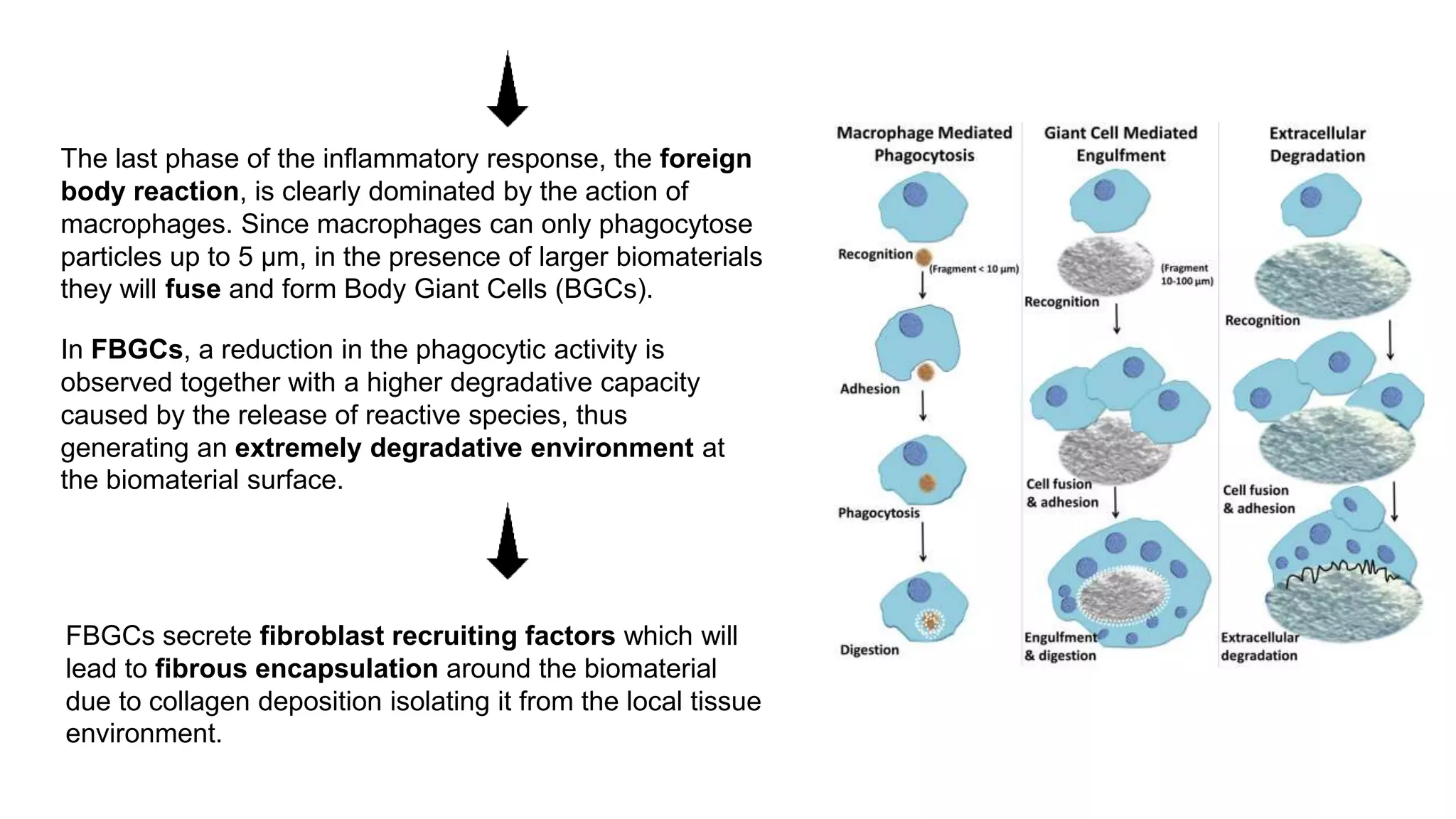
Macrophages play a central role in the body's inflammatory response to implanted biomaterials. After biomaterial implantation, macrophages are triggered by proteins that adsorb to the material's surface. They also respond to "danger signals" released by injured cells at the implant site. Macrophages recruit other immune cells and release inflammatory mediators, driving the acute and chronic inflammation phases. During the foreign body reaction phase, macrophages form foreign body giant cells that work to degrade and encapsulate the biomaterial through secretion of reactive species and fibroblast growth factors.
![What are macrophages and what is their role?
• Crucial component of innate immunity
• Central role in inflammation and host defense
• Specialized in the phagocytosis and neutralization
of cellular debris and potentially hazardous agents,
including pathogens.
• Non migratory tissue specific macrophages monitor
local environment.
• Orchestrate inflammatory reactions through chemokines and
cytokines, which recruit and activate neutrophils,
monocytes, and lymphocytes.
• In response to an inflammatory stimulus, these cells also
produce large amounts of effector molecules, including
several growth factors, such as for example platelet-derived
growth factors and fibroblast growth factors.
• Surface receptors: scavenger receptors, pattern recognition
receptors [Toll-like receptors (TLRs), C-type lectin receptors,
RIG-I-like receptors, nod-like receptors], cytokine receptors,
and adhesion molecules](https://image.slidesharecdn.com/macrophagesandbiomaterials-221120140242-f28b180d/75/Macrophages-and-Biomaterials-pptx-2-2048.jpg)