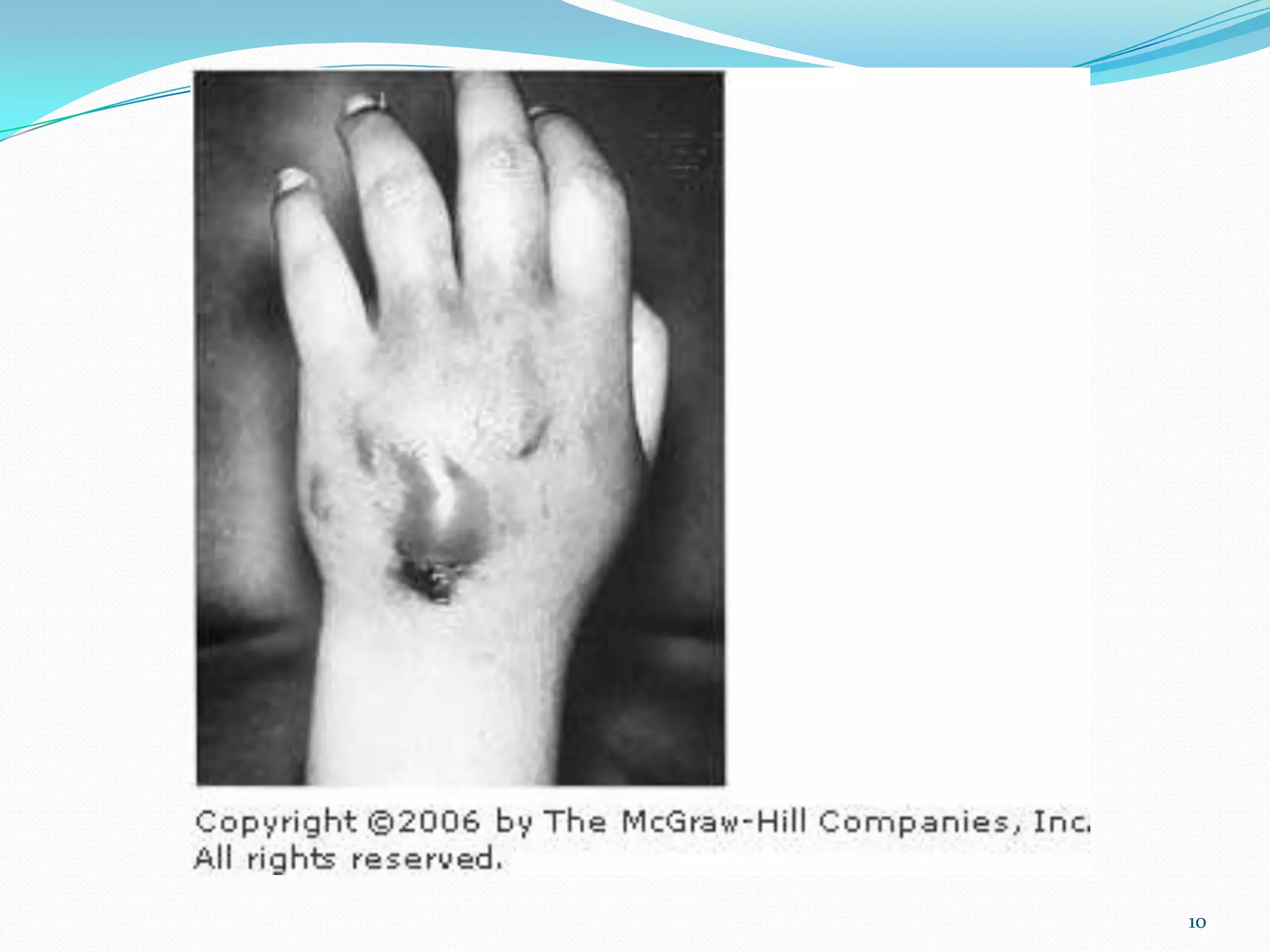
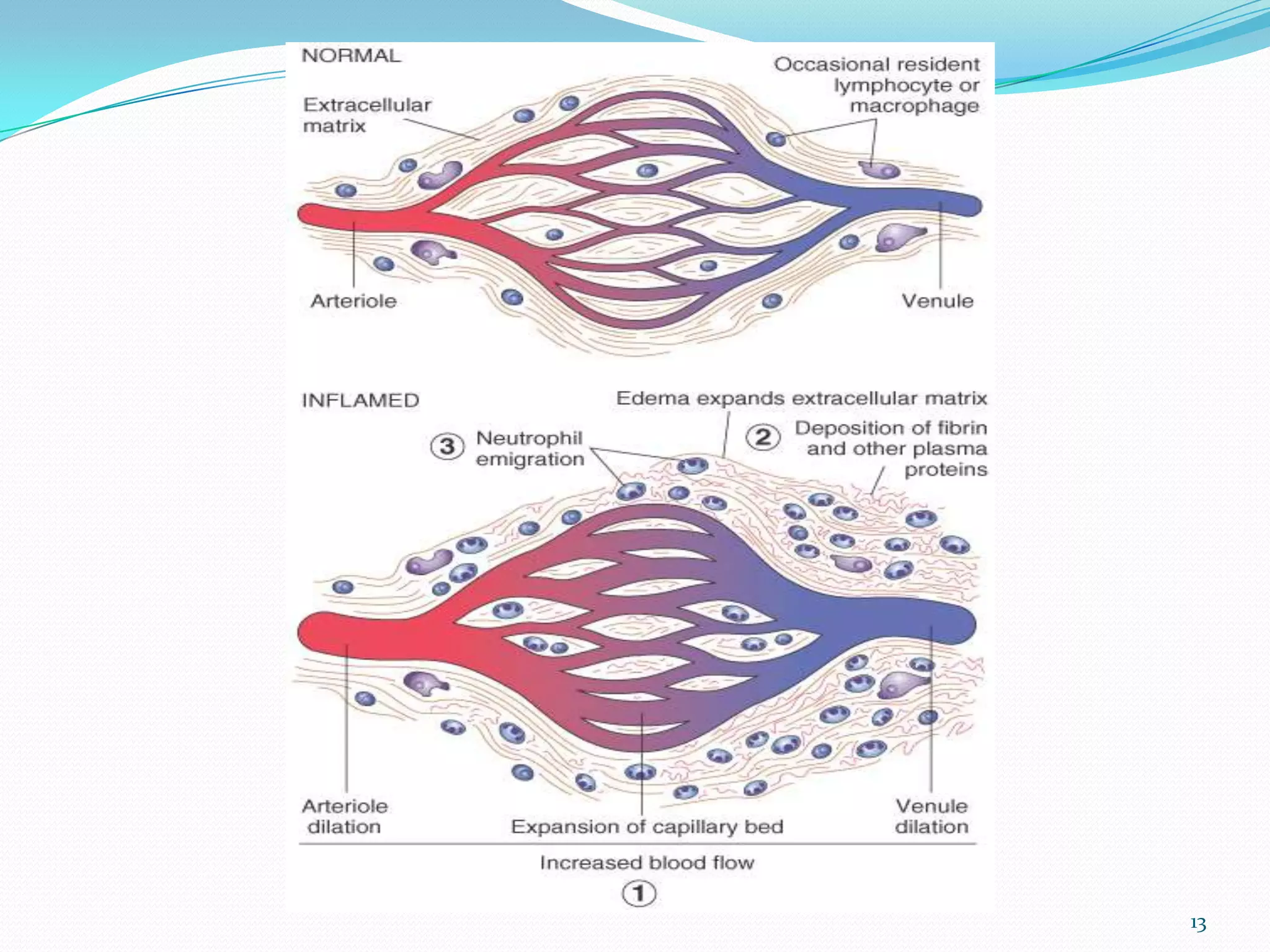
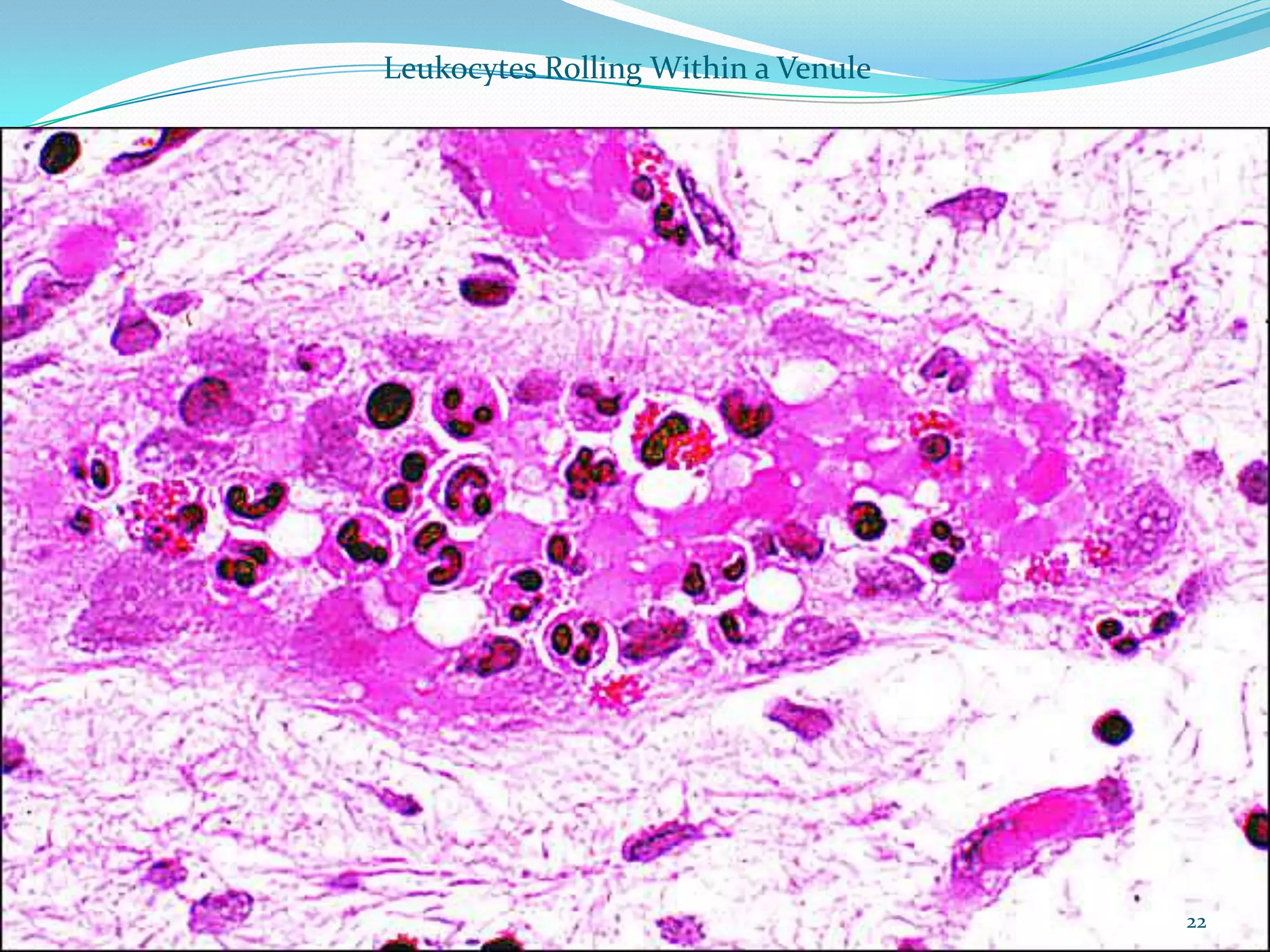
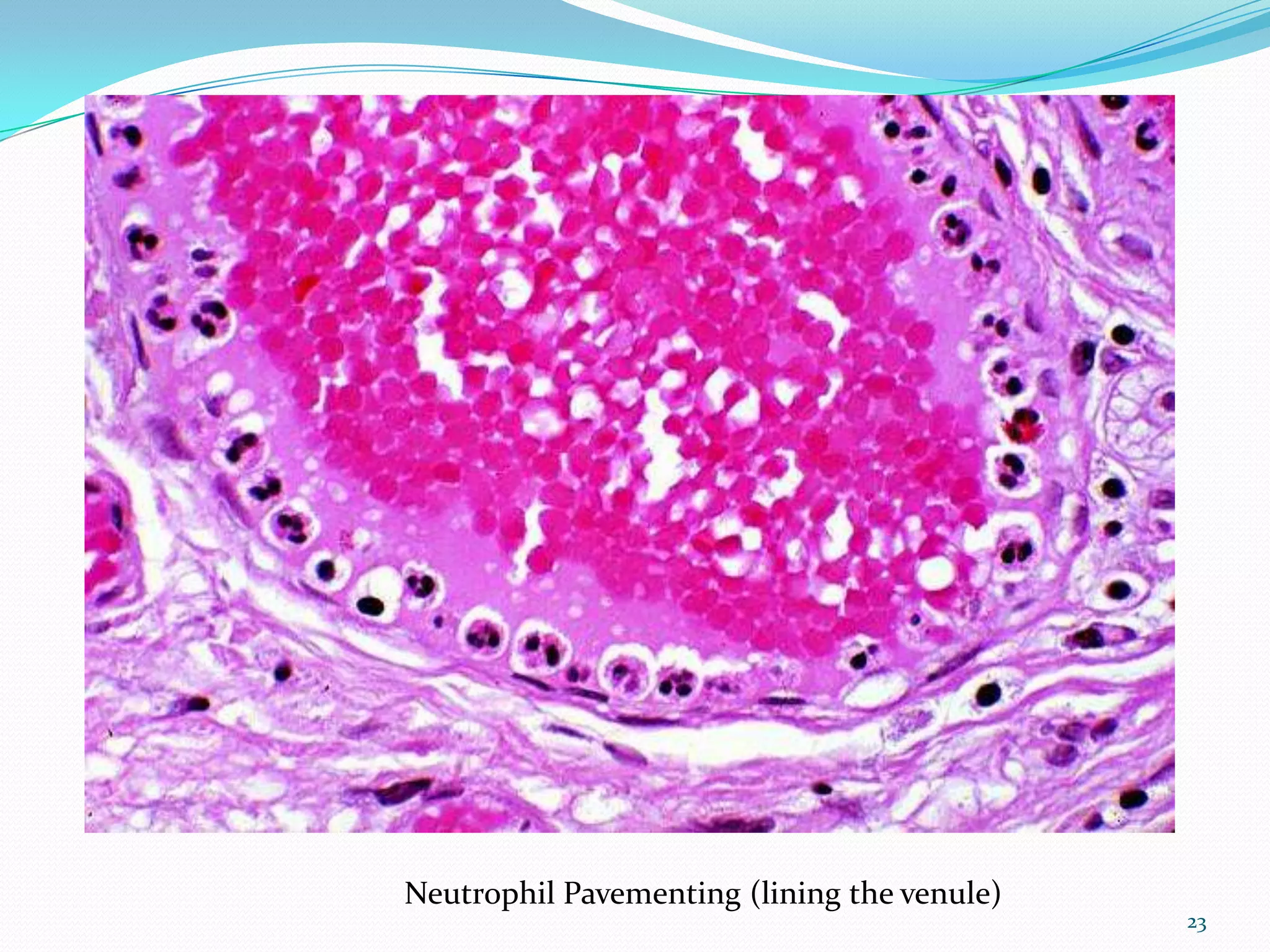
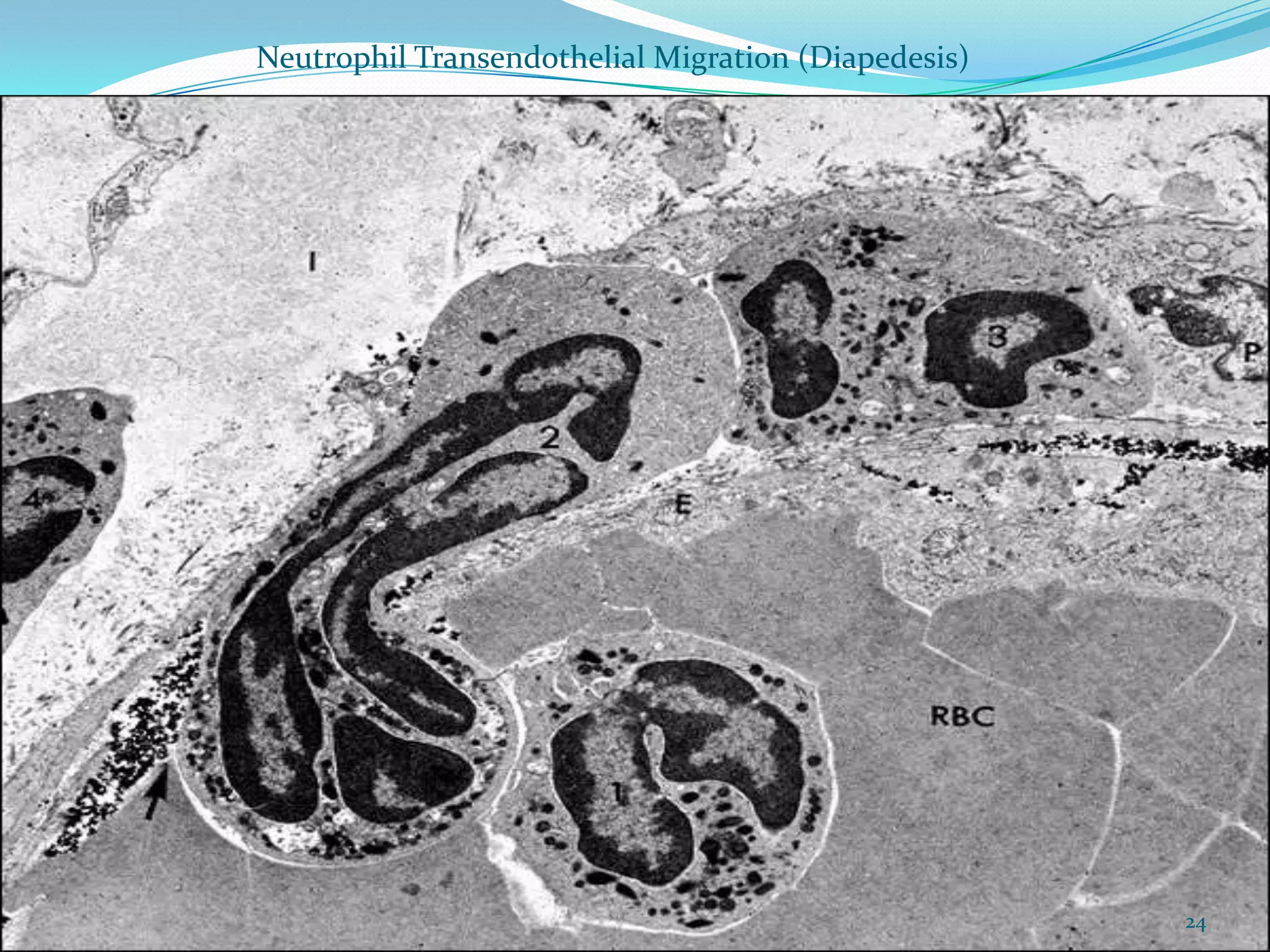
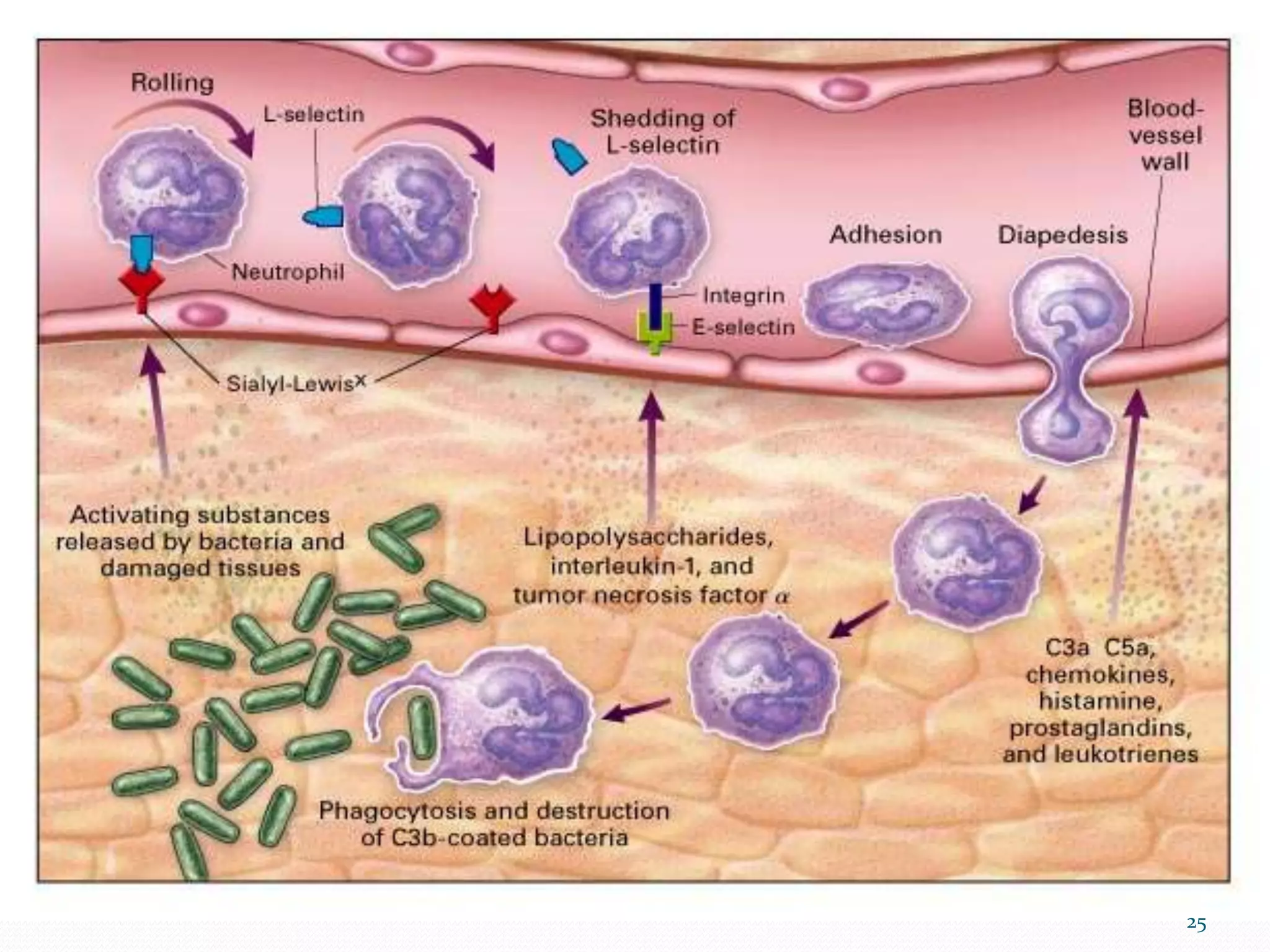
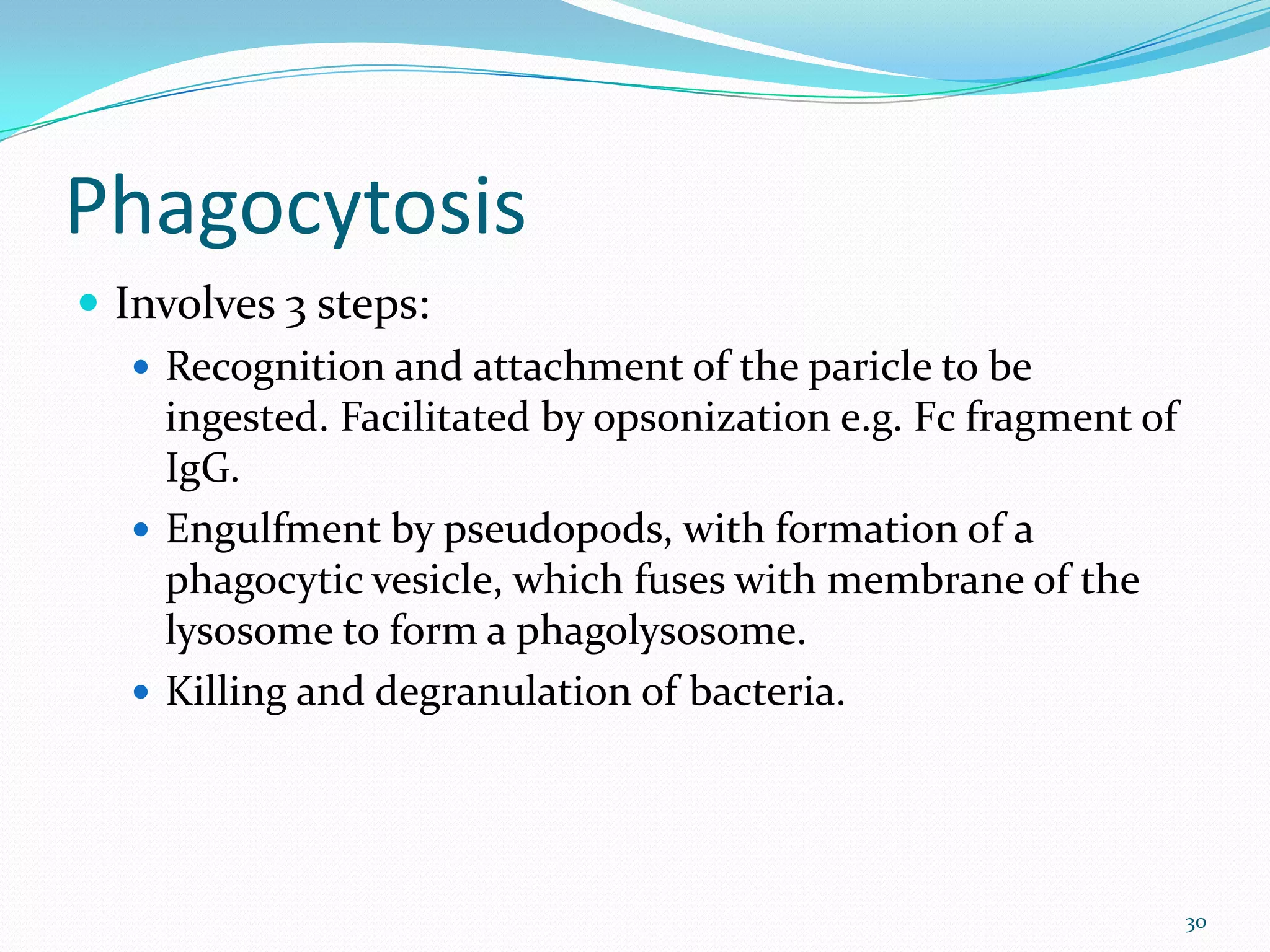
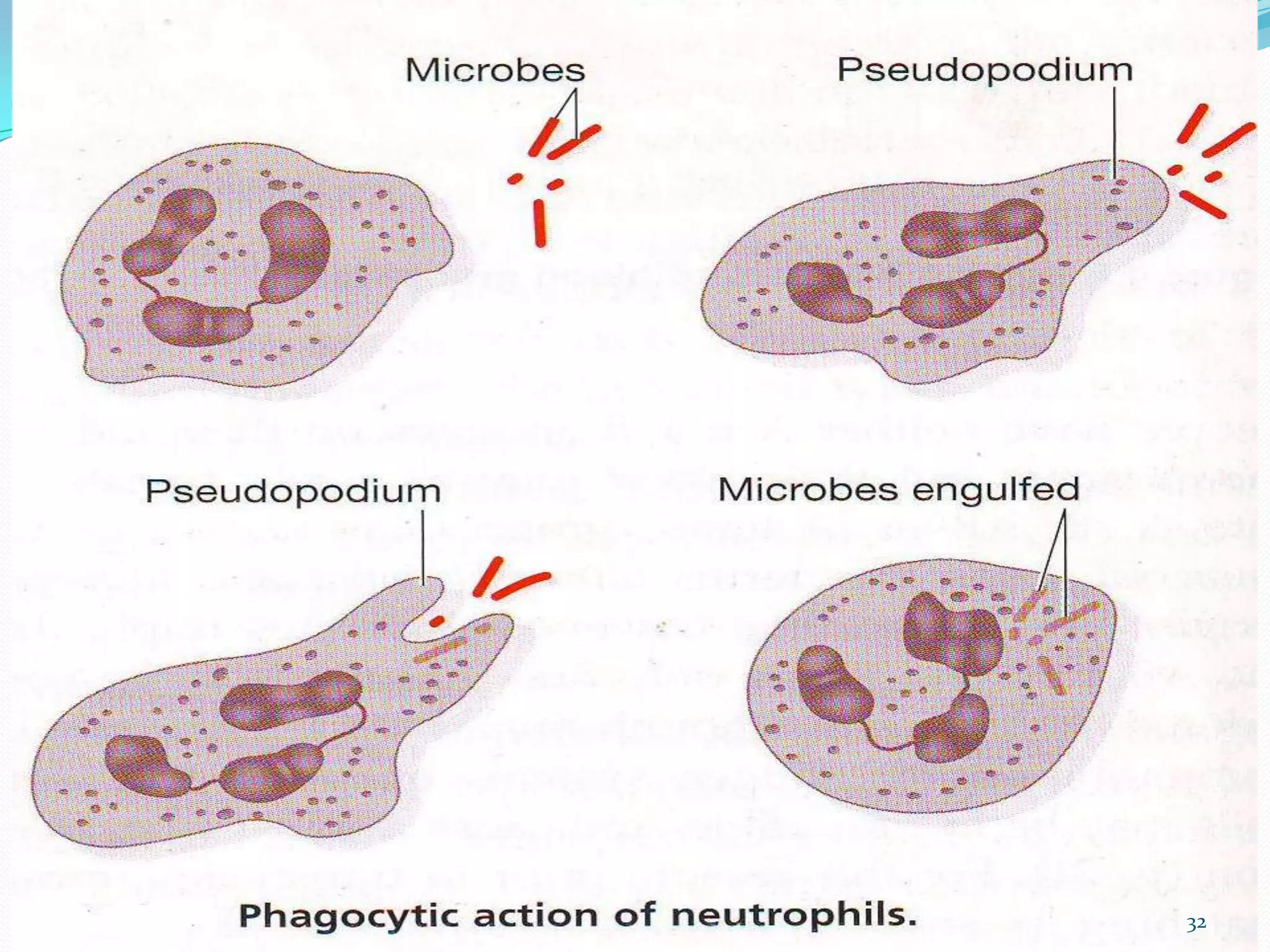
The document outlines the process and mechanisms of acute inflammation, including definitions of key terms like exudation and edema, and details the roles of inflammation in response to injury. It describes the major components of acute inflammation, such as changes in vascular flow, the recruitment and activation of leukocytes, and the cellular events involved in phagocytosis. Furthermore, it highlights potential outcomes of acute inflammation, which can range from complete resolution to chronic inflammation or tissue scarring.