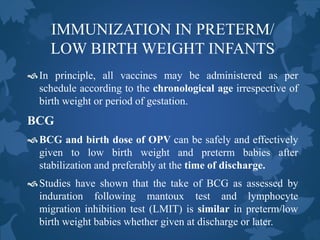
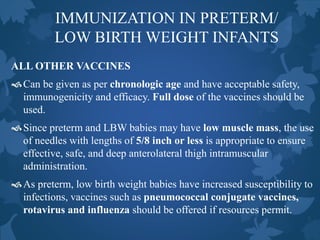
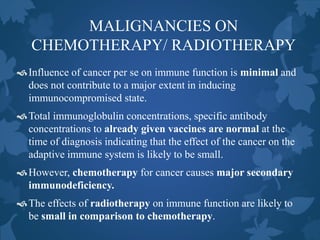
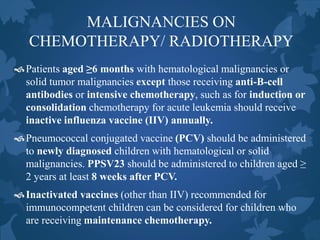
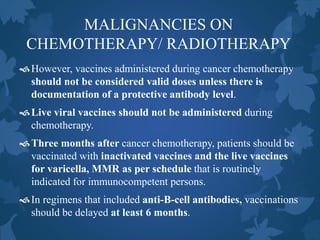
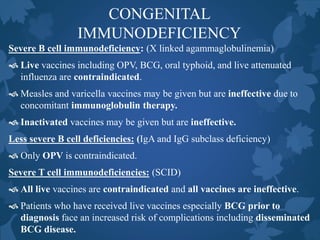
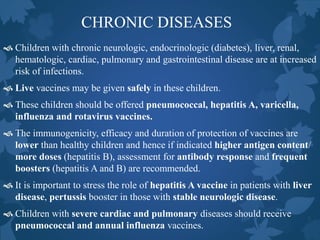
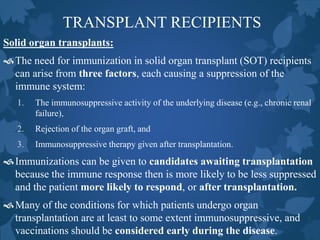
This document discusses special situations and adverse events following immunization. It provides guidance on vaccinating preterm/low birth weight infants, those receiving corticosteroids or immunosuppressive therapy, children with malignancies, congenital immunodeficiencies, chronic diseases, allergies, bleeding disorders, or acute illness. It recommends that most vaccines can be administered according to chronological age for preterm/low birth weight infants. It also provides specific guidance on contraindications and precautions for different groups.













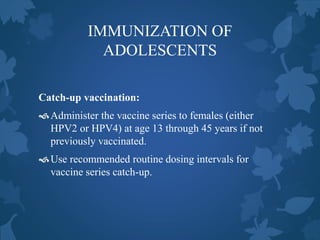
![IMMUNIZATION OF
ADOLESCENTS
Routine vaccination:
Minimum age: 9 years
HPV4 [Gardasil] and HPV2 [Cervarix] are licensed and available.
Either HPV4 (0, 2, 6 months) or HPV2 (0, 1, 6 months) is
recommended in a 3-dose series for females aged 11 or 12 years.
HPV4 can also be given in a 3-dose series for males aged 11 or 12
years, but not yet licensed for use in males in India.
The vaccine series can be started beginning at age 9 years.
Administer the second dose 1 to 2 months after the first dose and the
third dose 6 months after the first dose (at least 24 weeks after the first
dose).](https://image.slidesharecdn.com/immunization-specialsituationsandaefi-141218015441-conversion-gate02/85/Immunization-special-situations-and-AEFI-59-320.jpg)