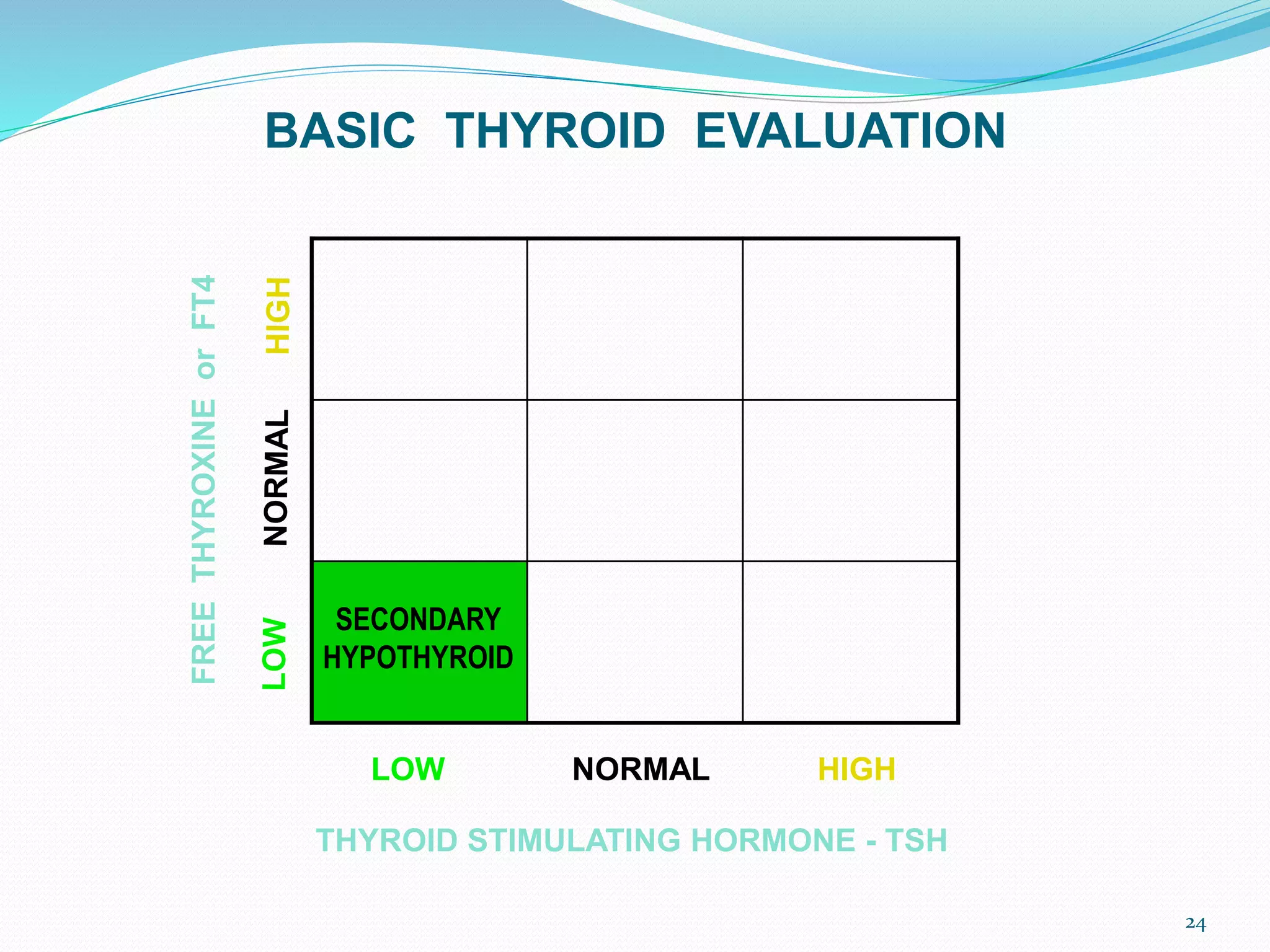
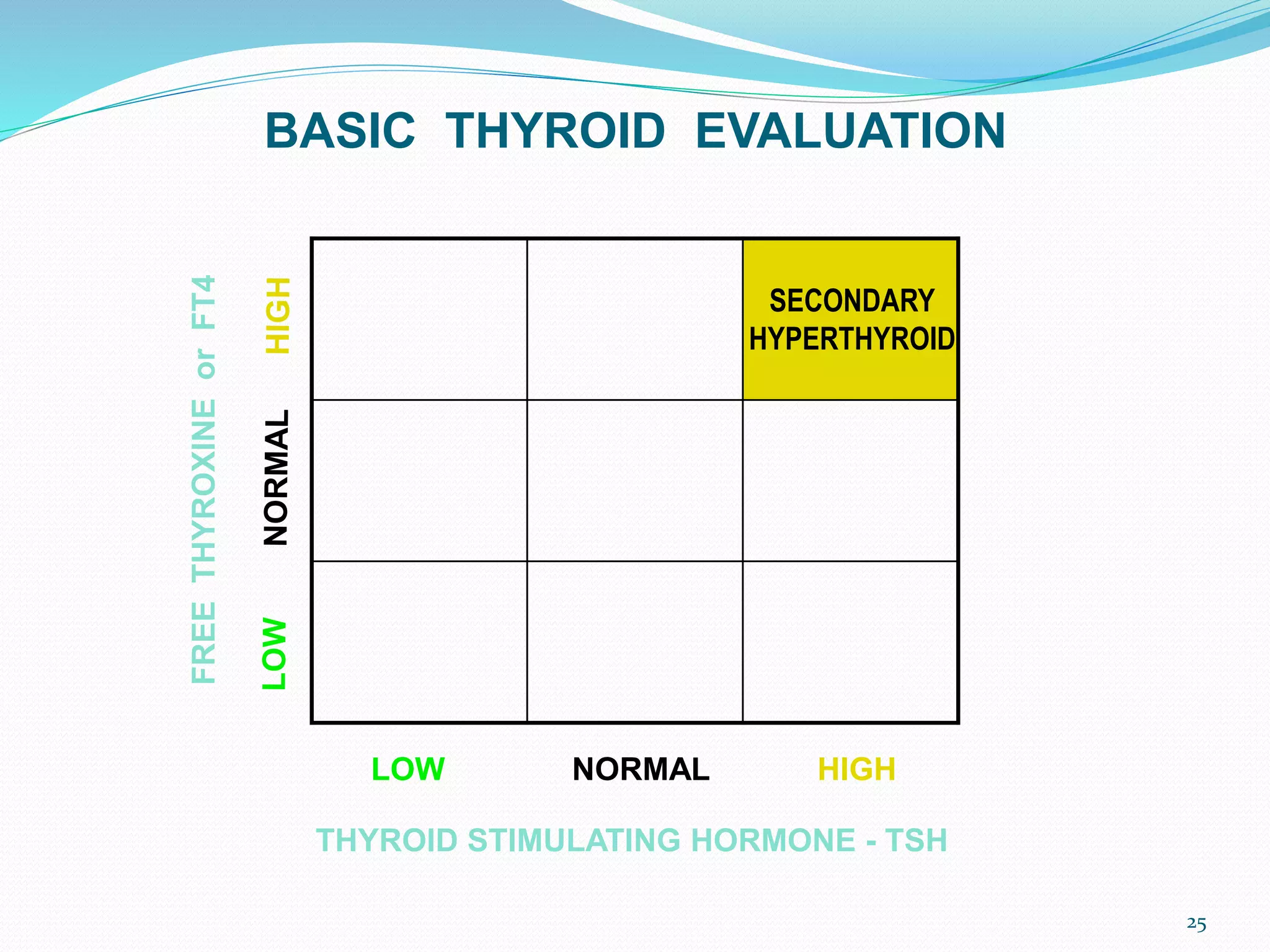
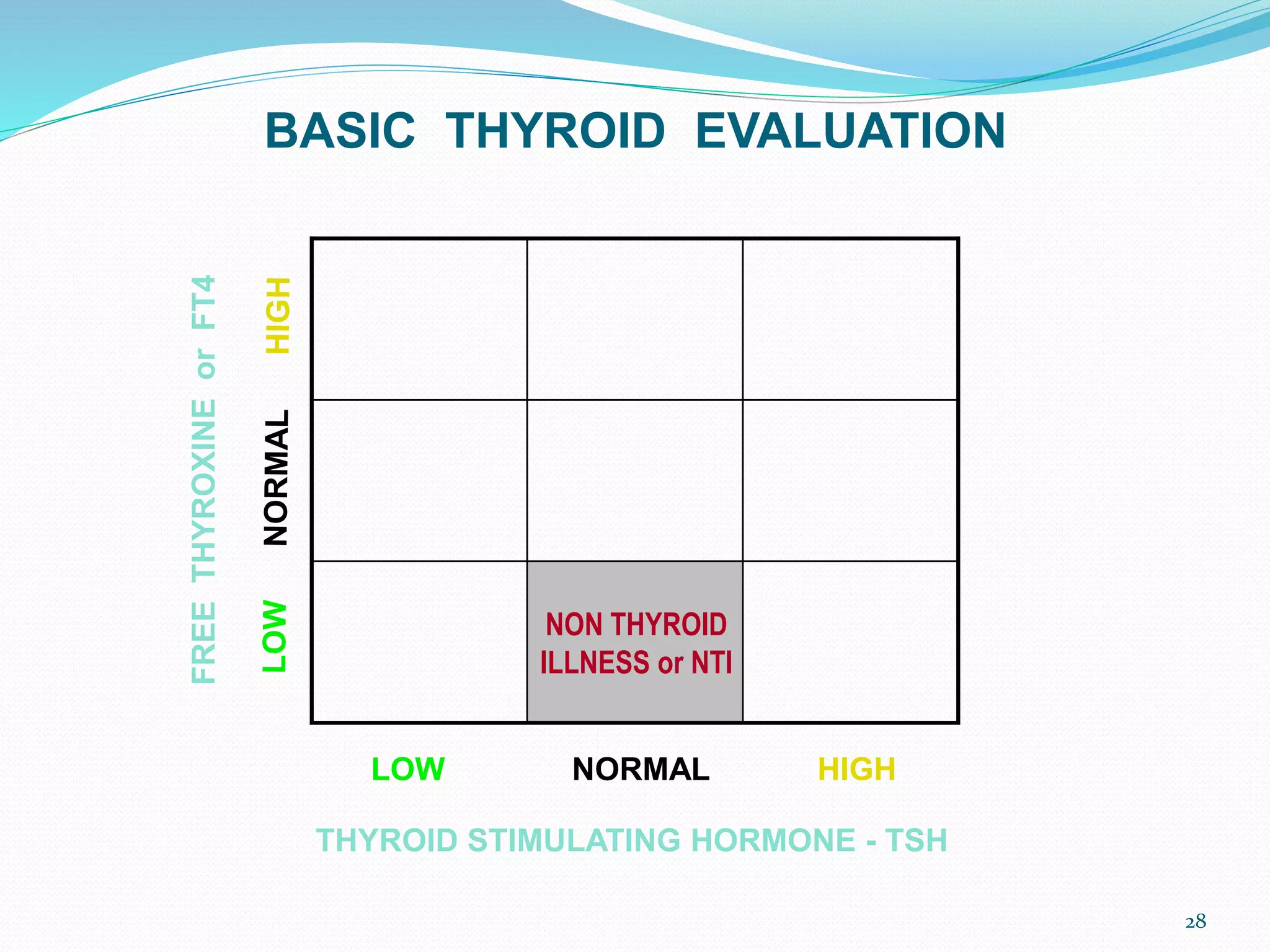
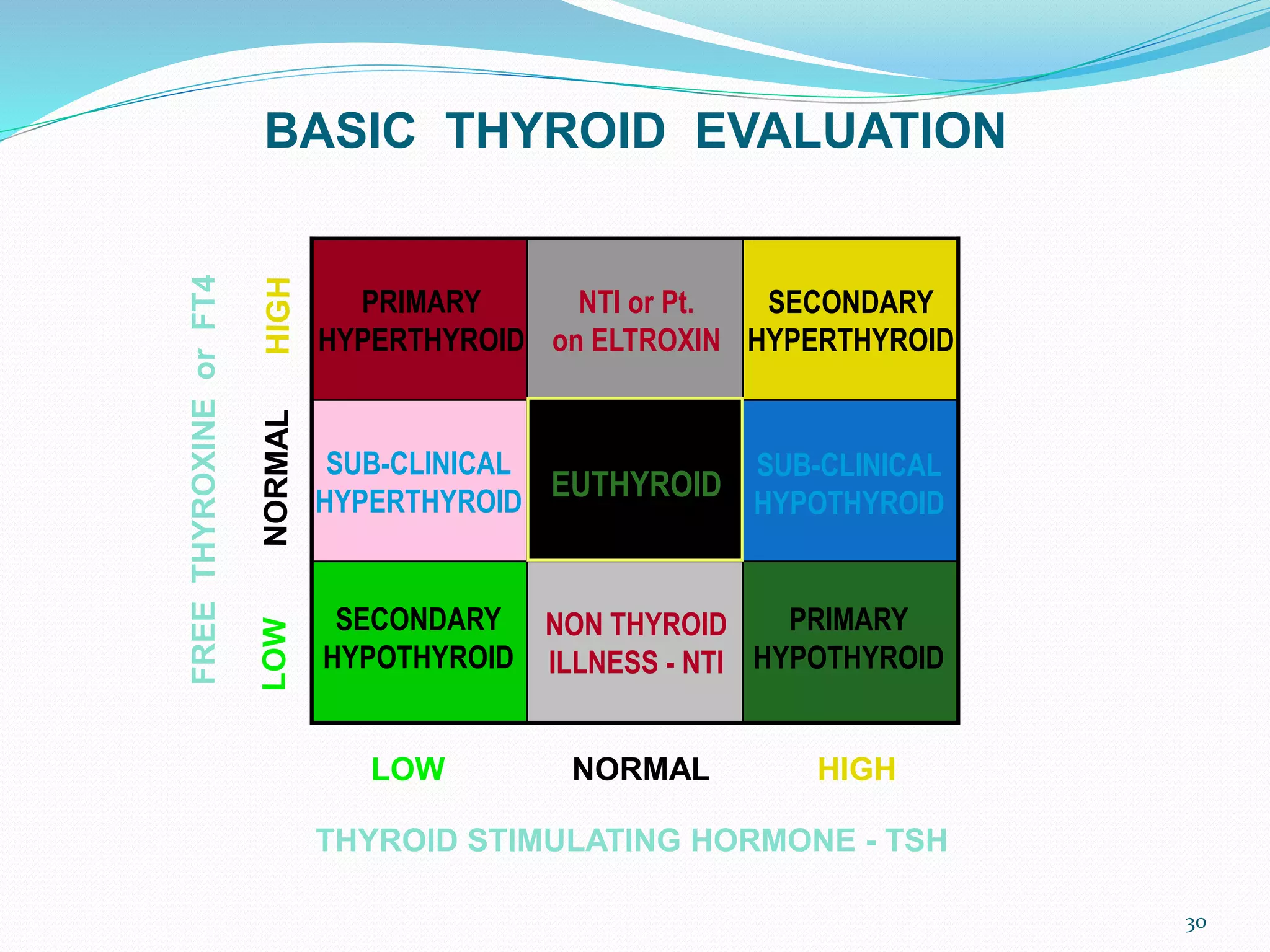
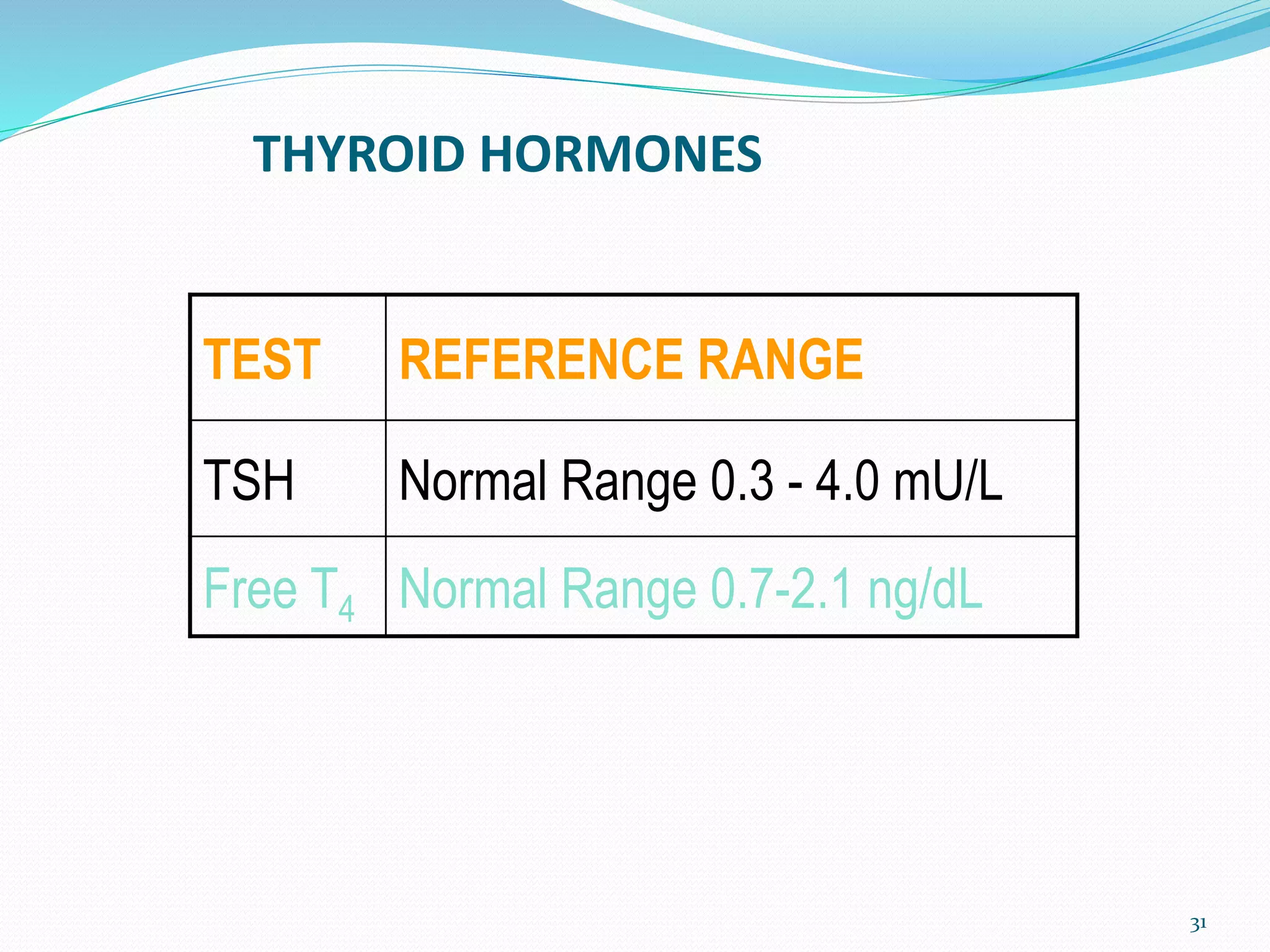
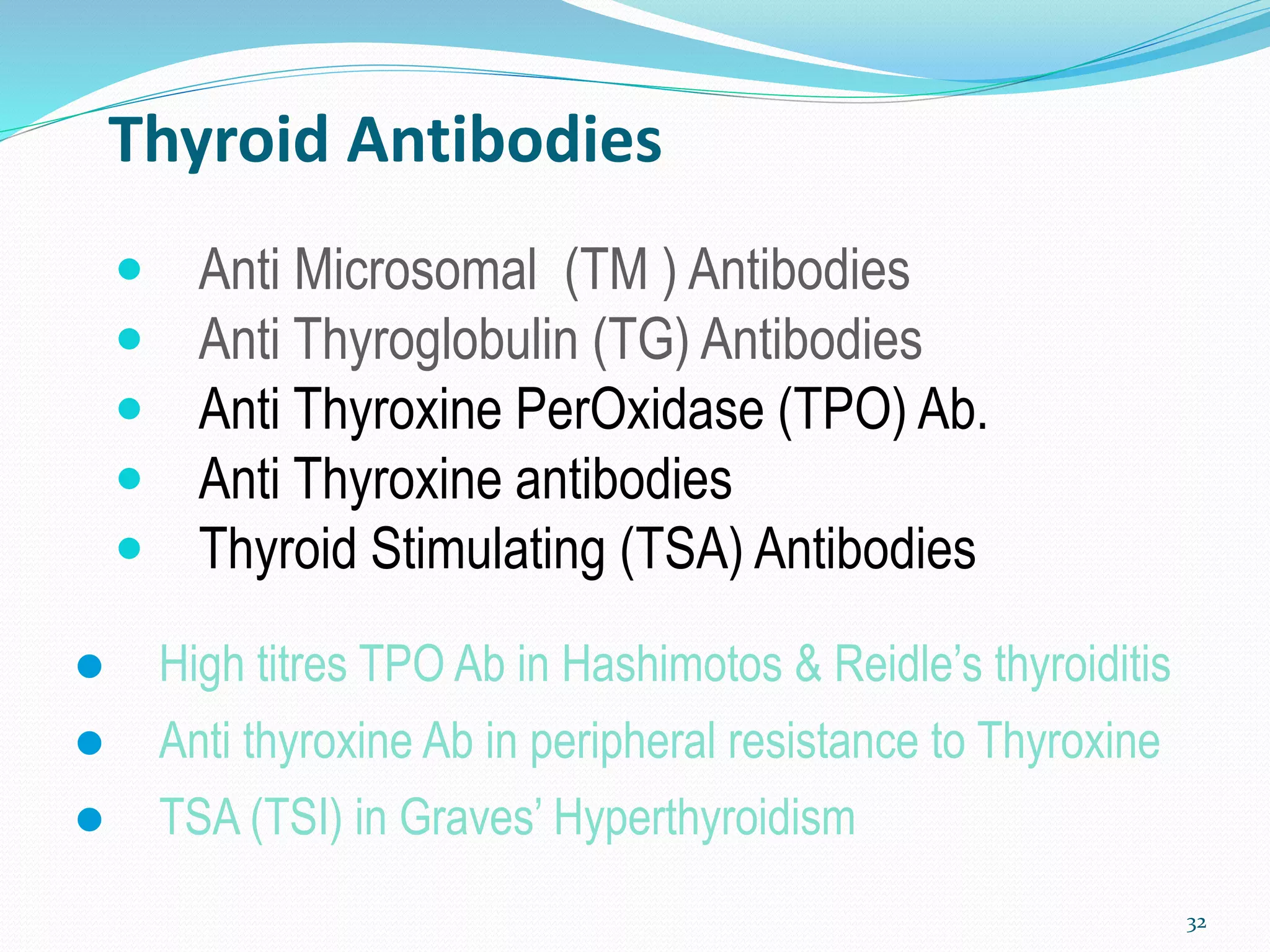
The document discusses the thyroid gland and hypothyroidism. It notes that the thyroid gland regulates vital body functions through hormones like T3 and T4. Hypothyroidism is the most common endocrine disease and is often underdiagnosed. It presents with symptoms like fatigue, weight gain, and menstrual irregularities. Diagnosis involves low free T4 and high TSH levels. Treatment is typically lifelong levothyroxine supplementation to replace thyroid hormones. The goal is to alleviate symptoms and maintain normal TSH levels.