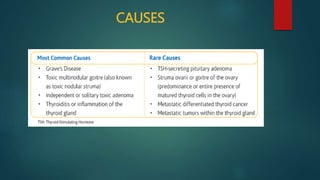
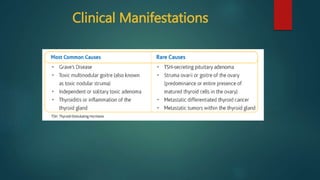
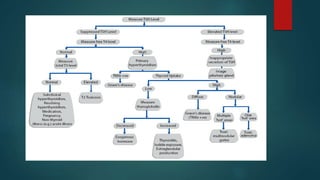
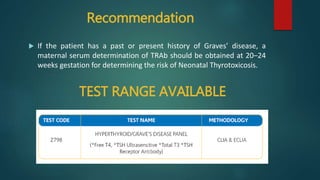
Hyperthyroidism, also known as thyrotoxicosis, results from elevated thyroid hormones in the blood and causes hypermetabolism. Graves' disease is the most common cause, an autoimmune disorder where thyroid receptor antibodies stimulate excess thyroid hormone production. Women are more frequently affected than men. Laboratory tests show suppressed TSH and increased thyroid hormone levels. Graves' disease in pregnancy can cause fetal and neonatal hyperthyroidism or hypothyroidism if not properly managed.