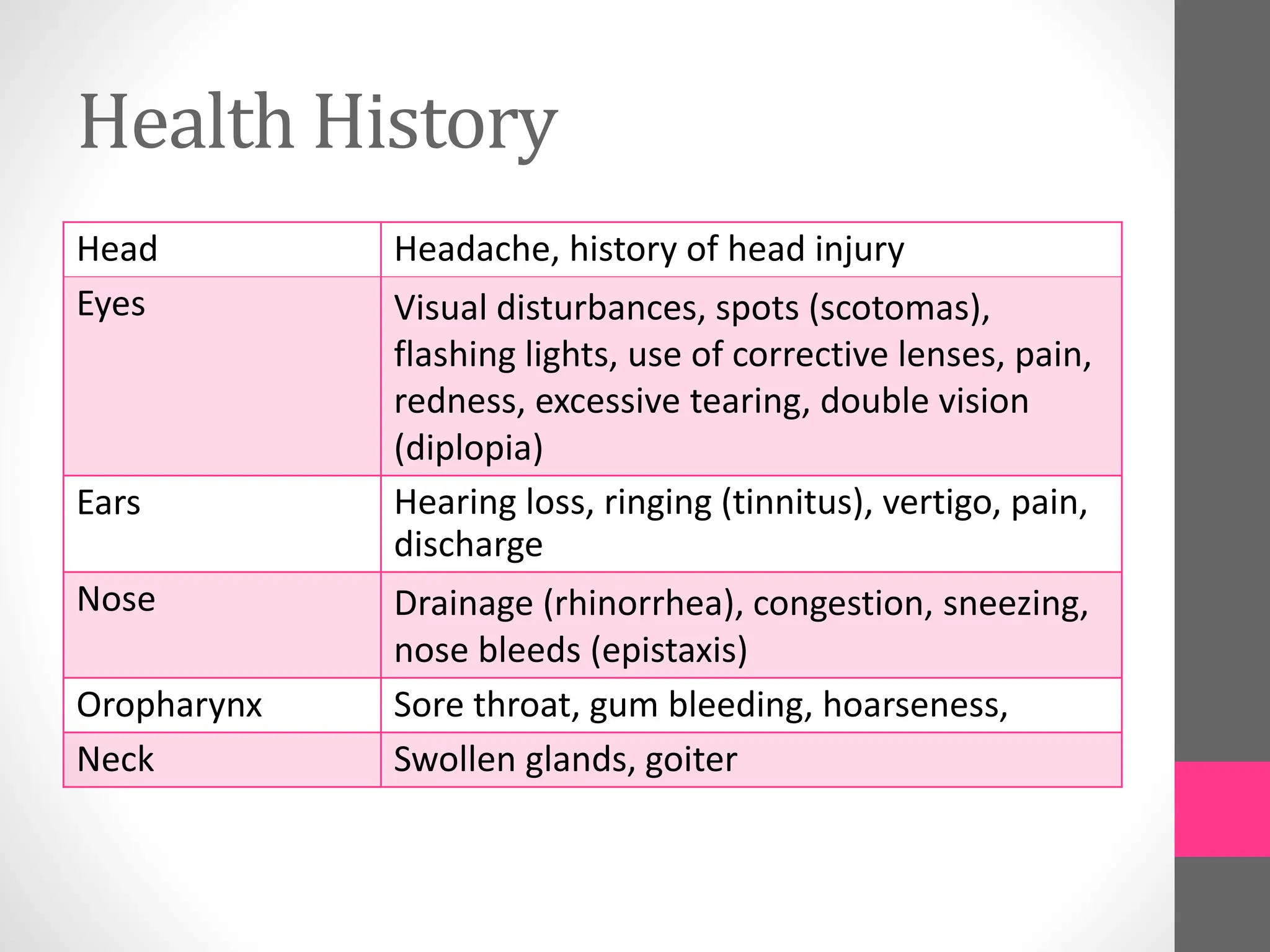
This document provides instructions and objectives for assessing the head, eyes, ears, nose, mouth and throat (HEENT). Key points include:
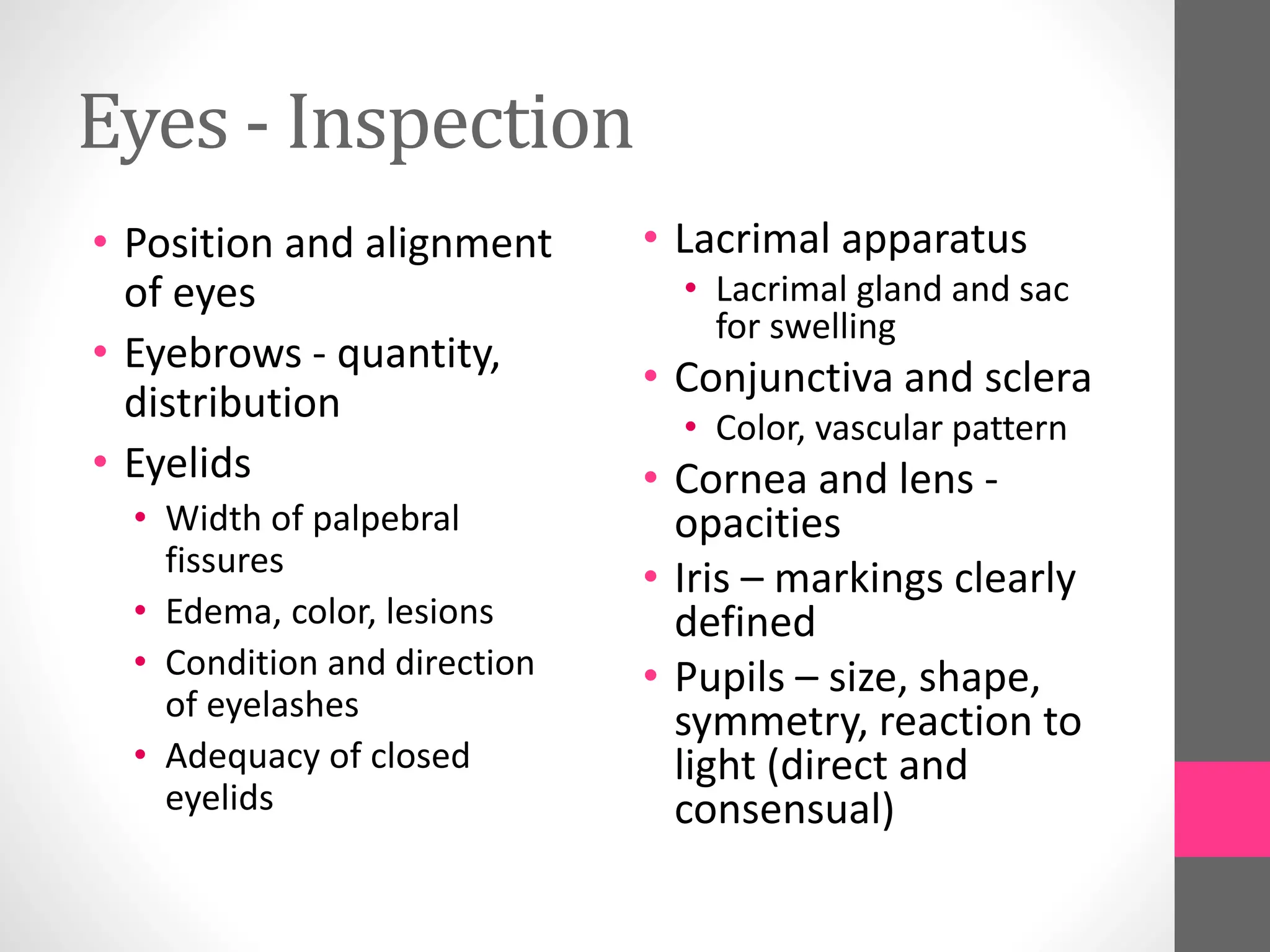
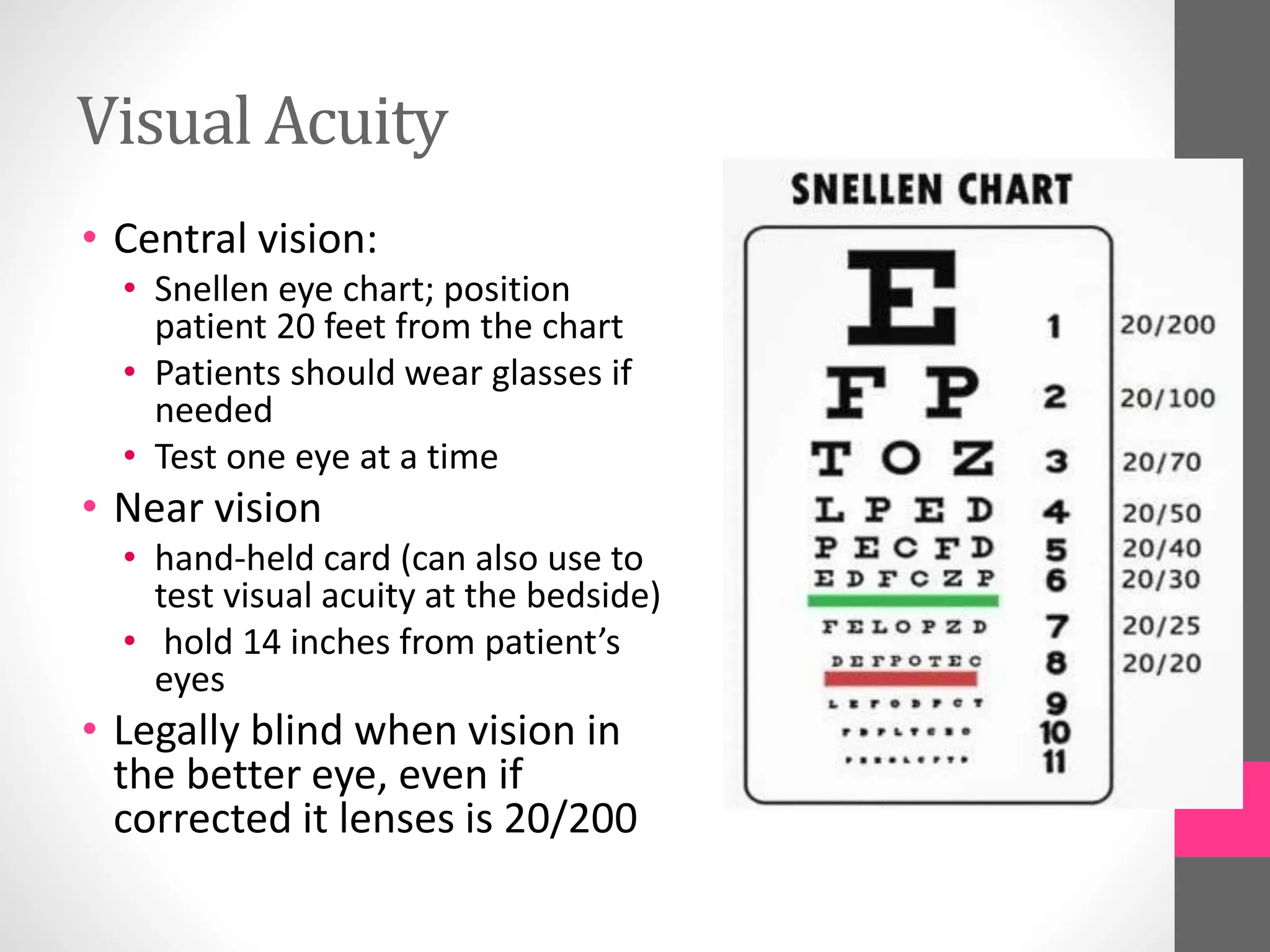
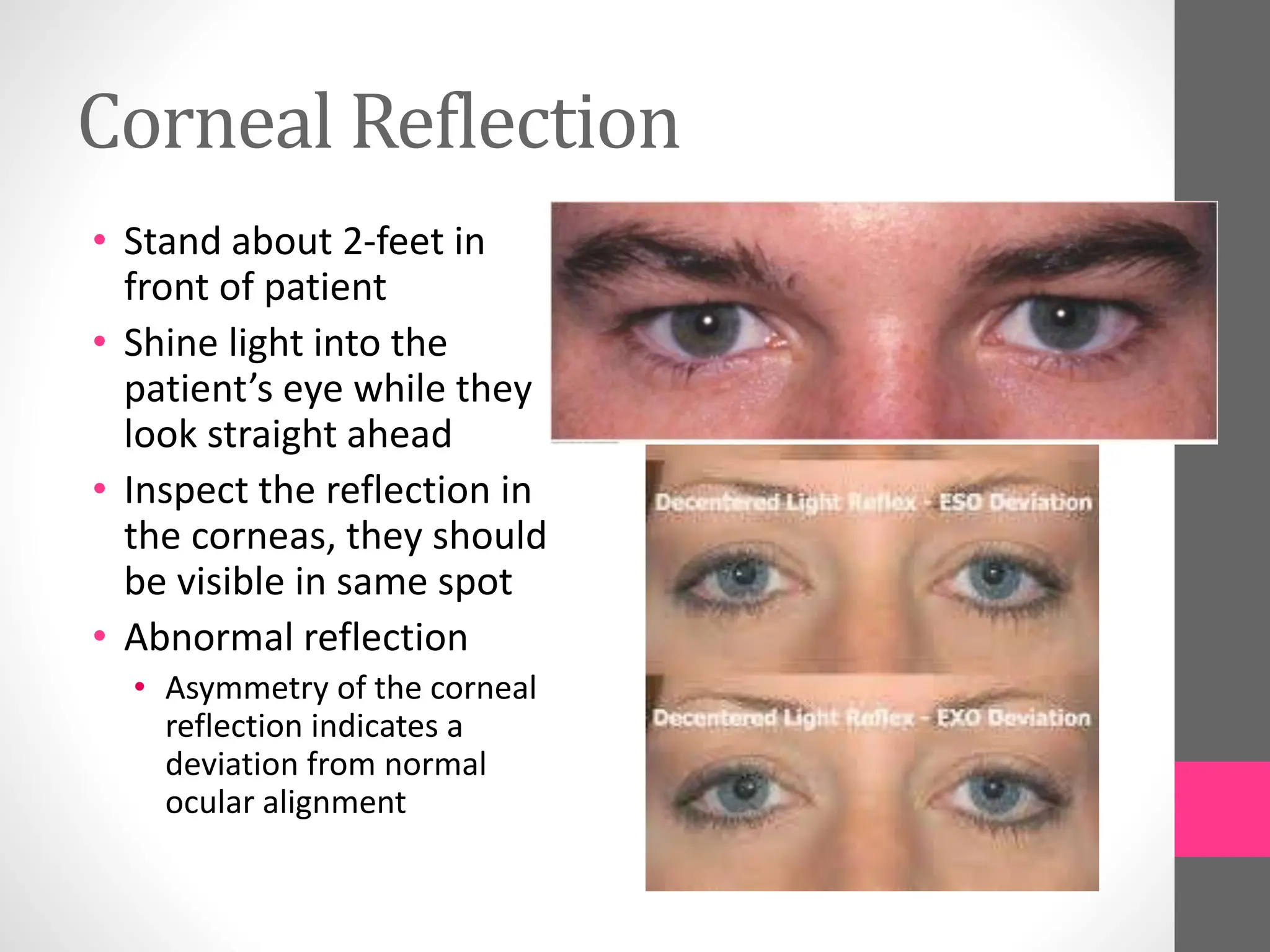
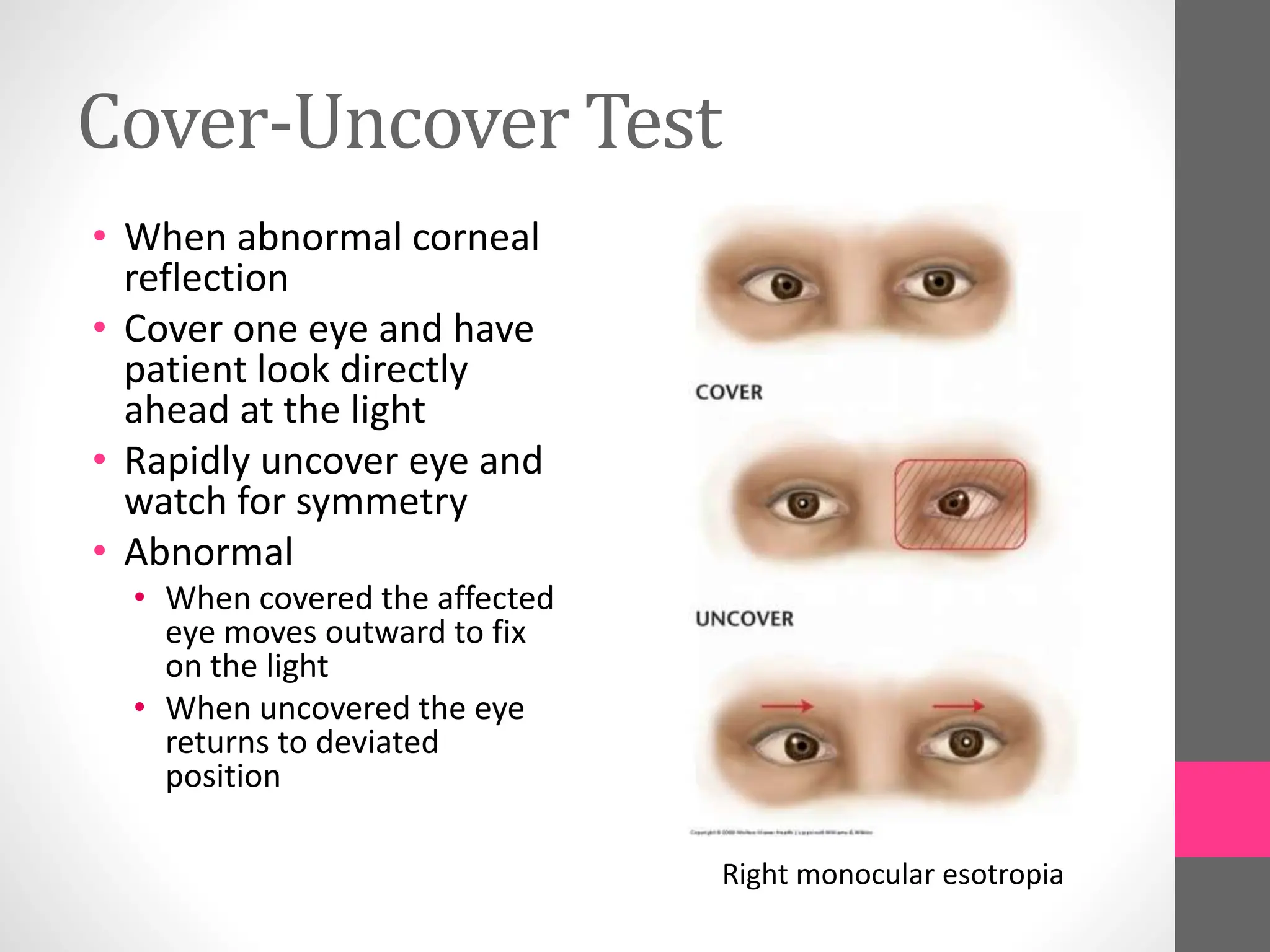
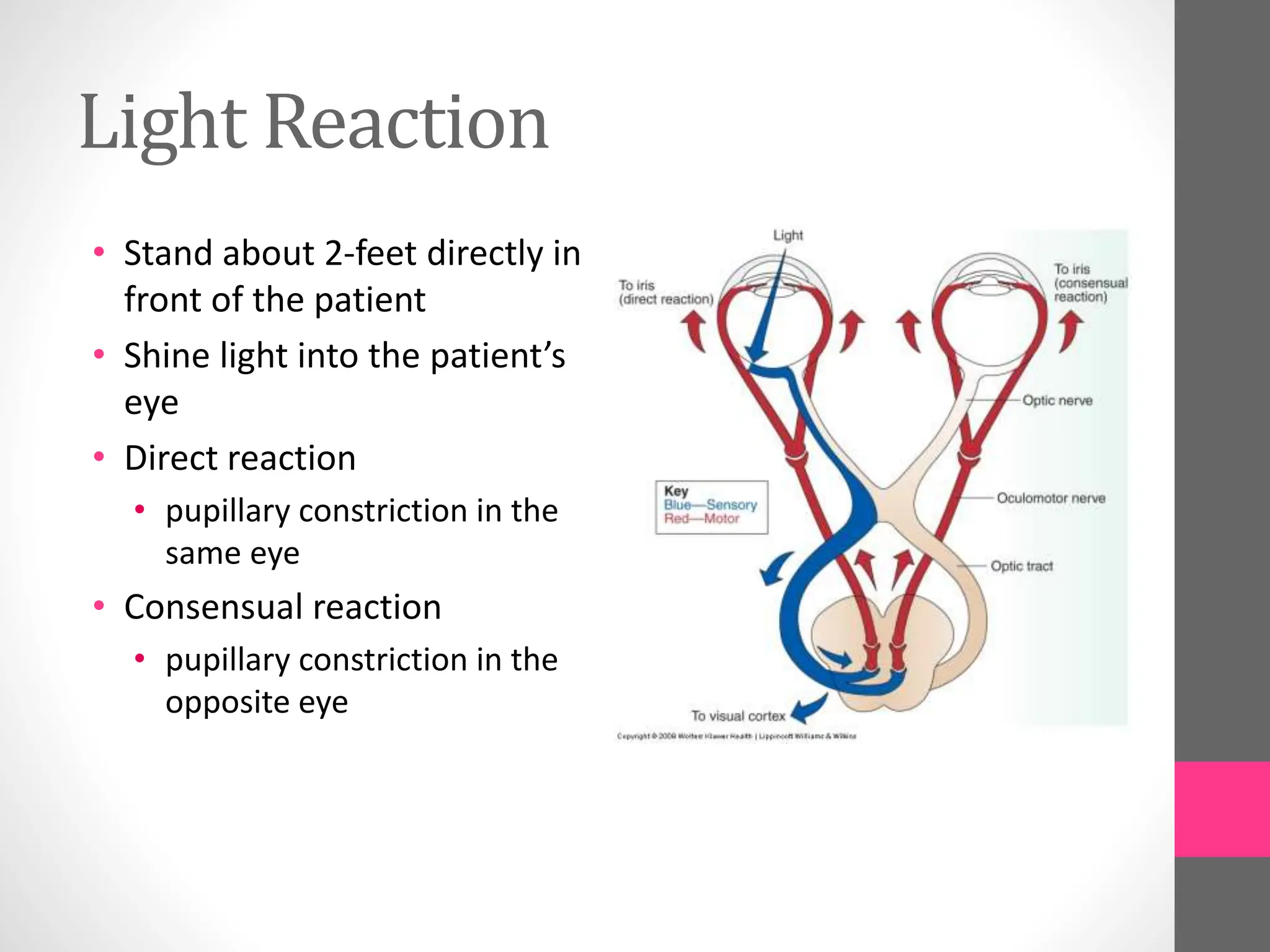
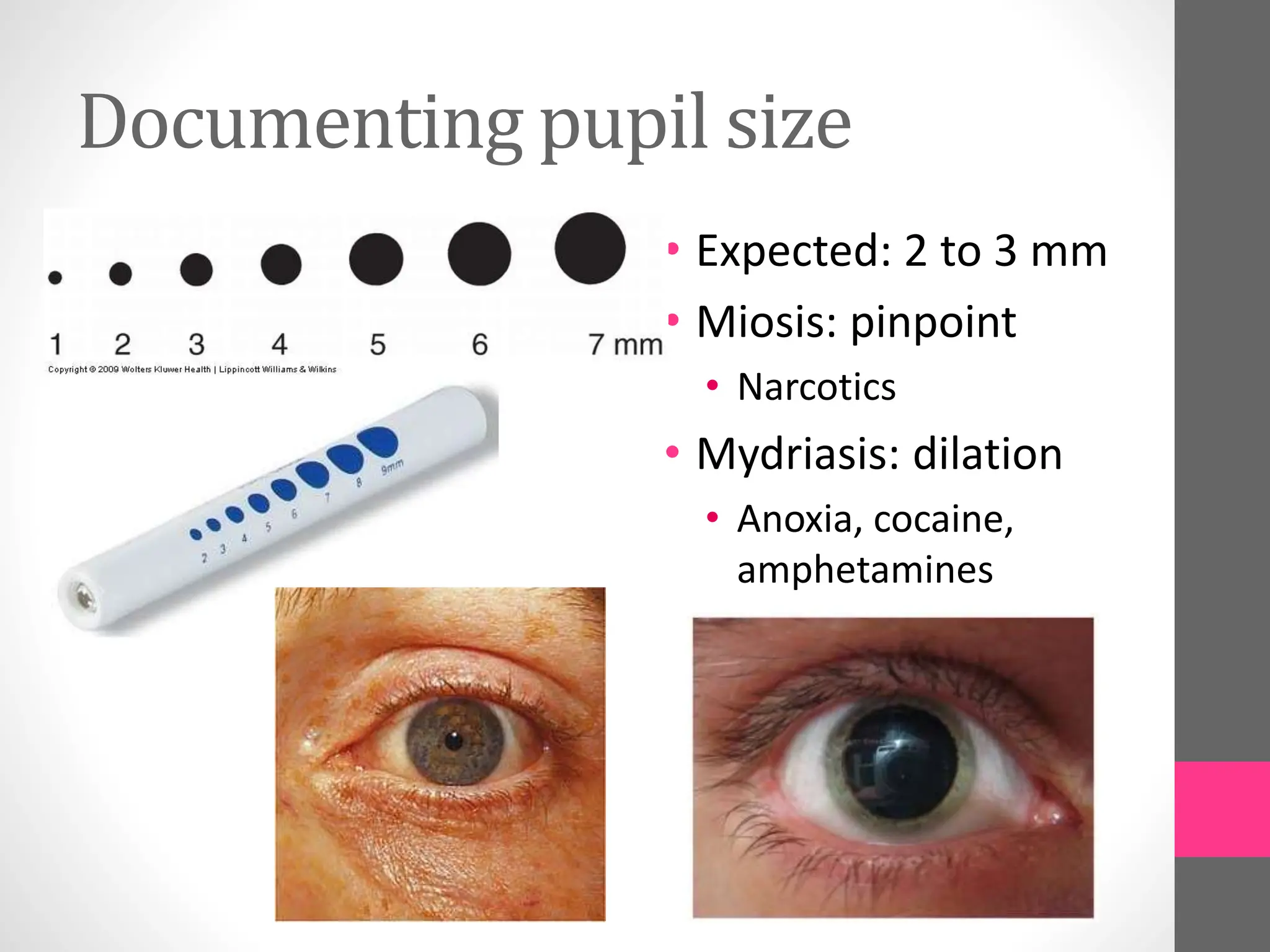
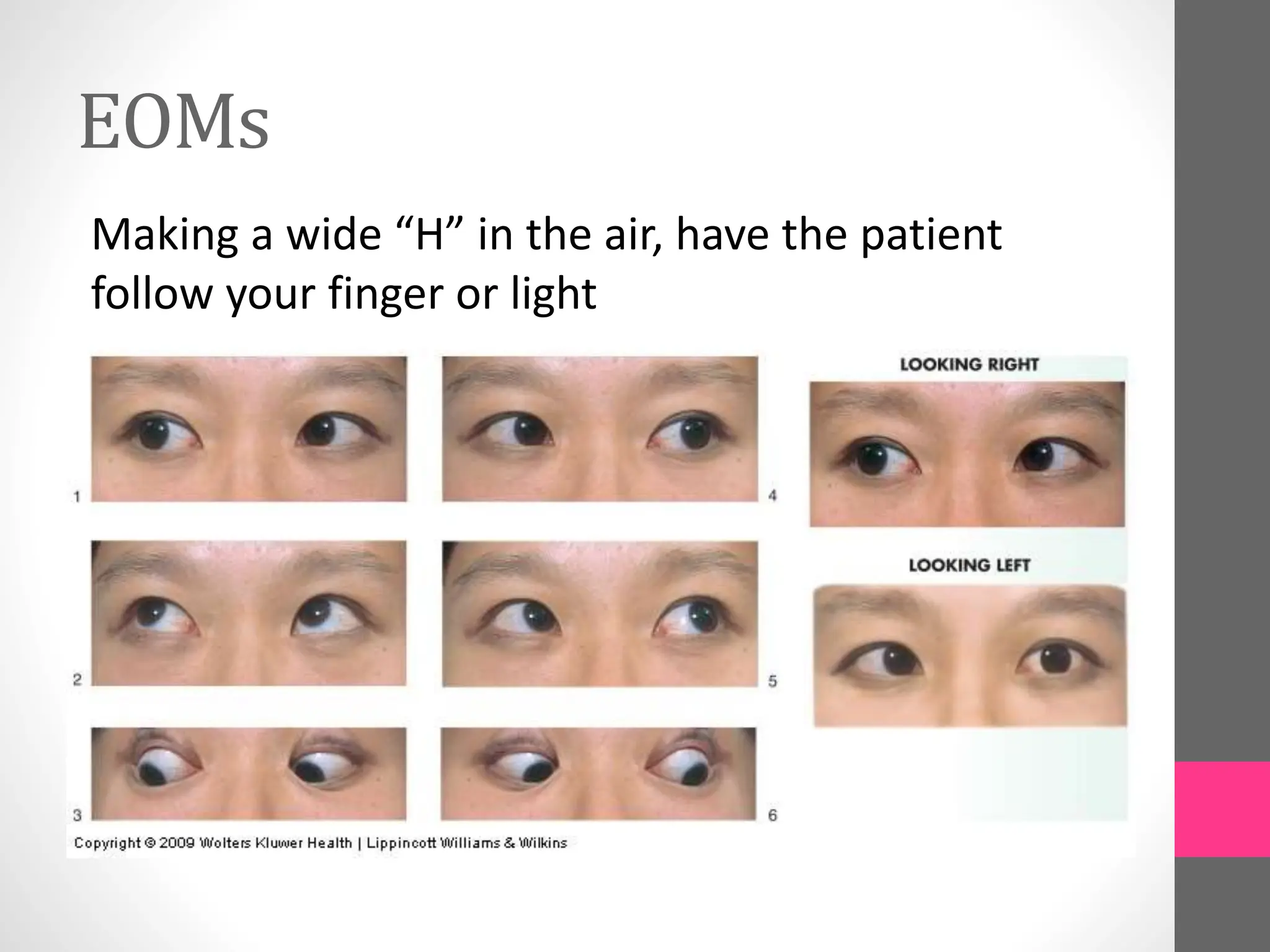
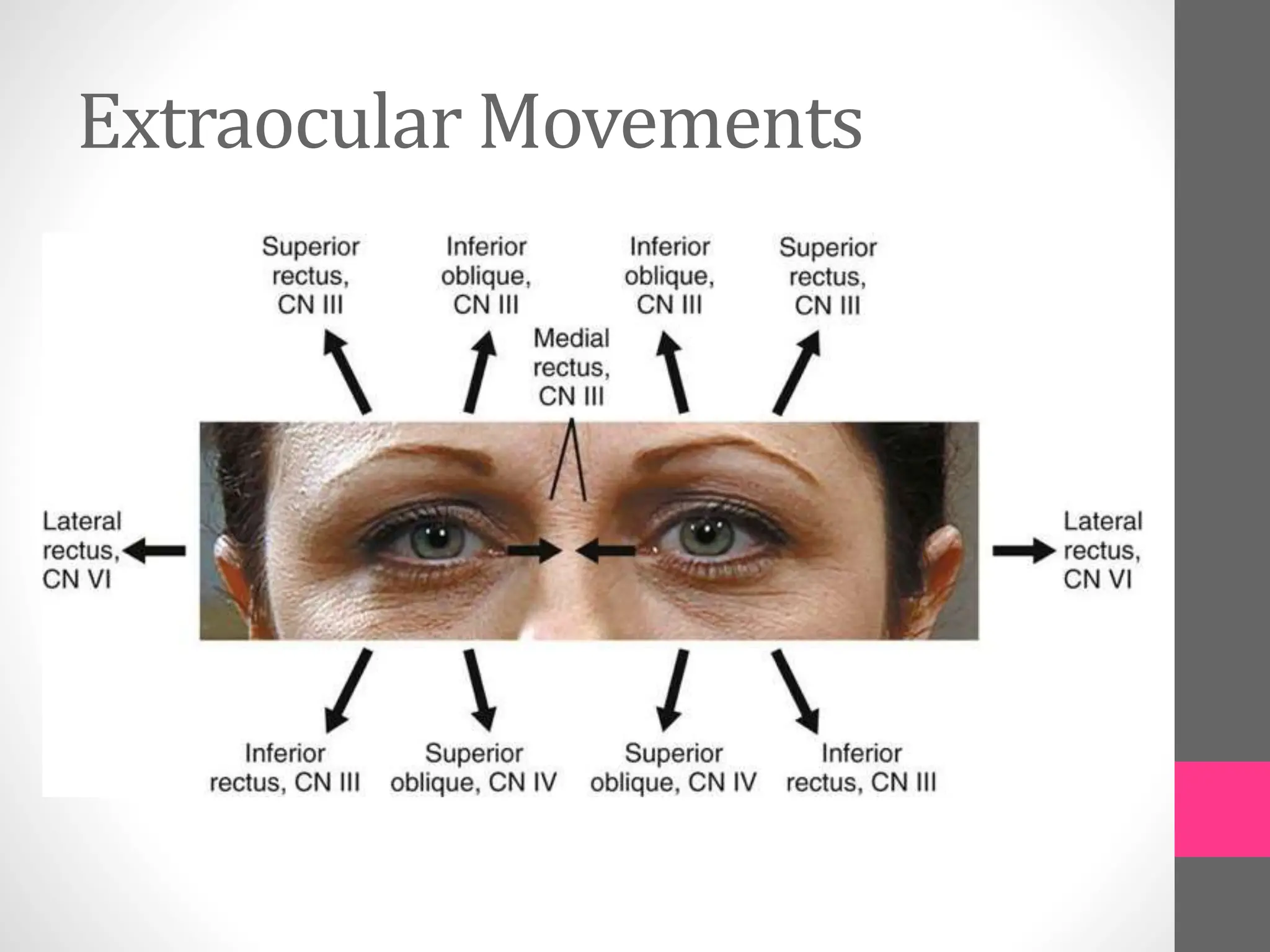
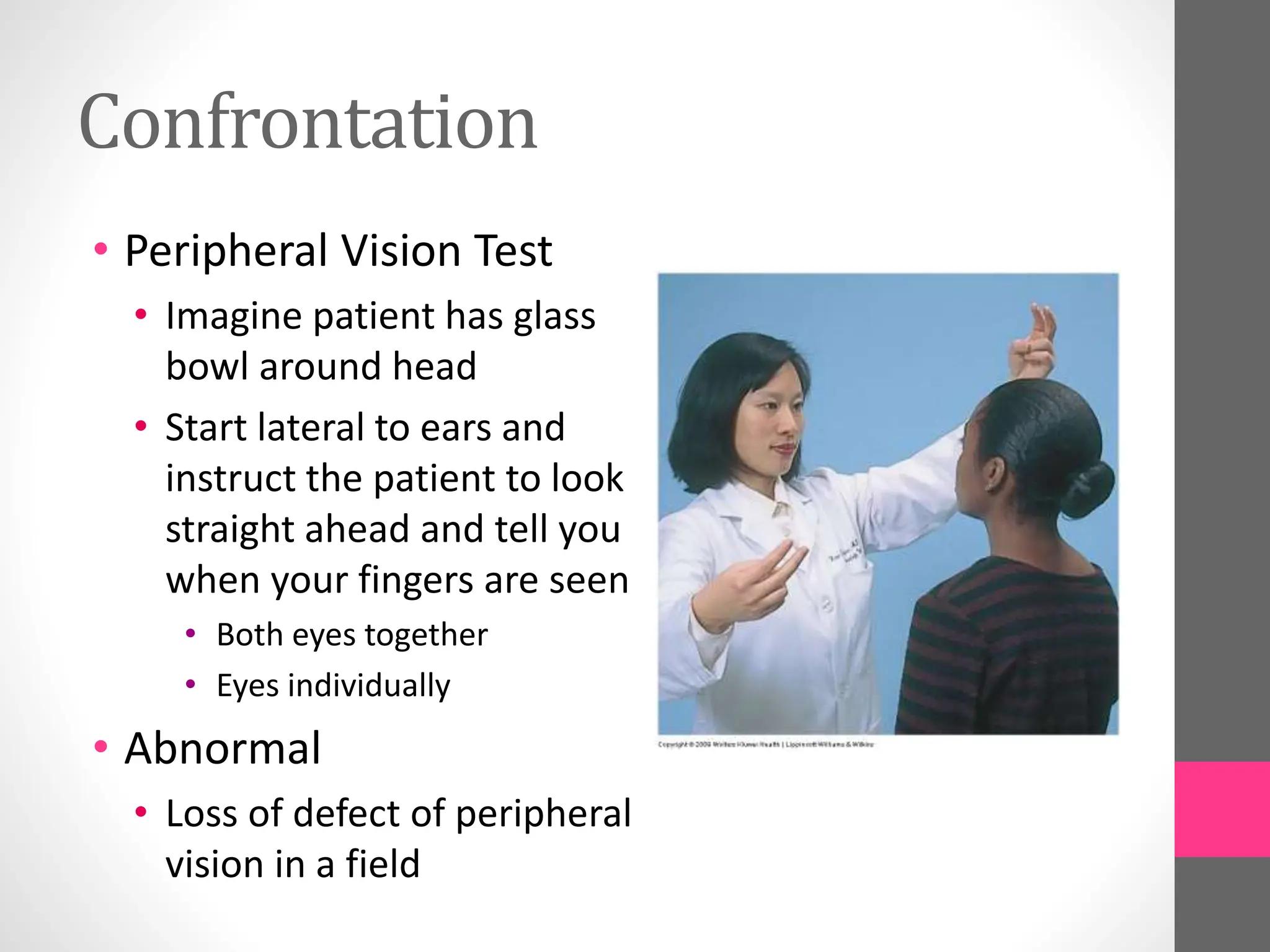
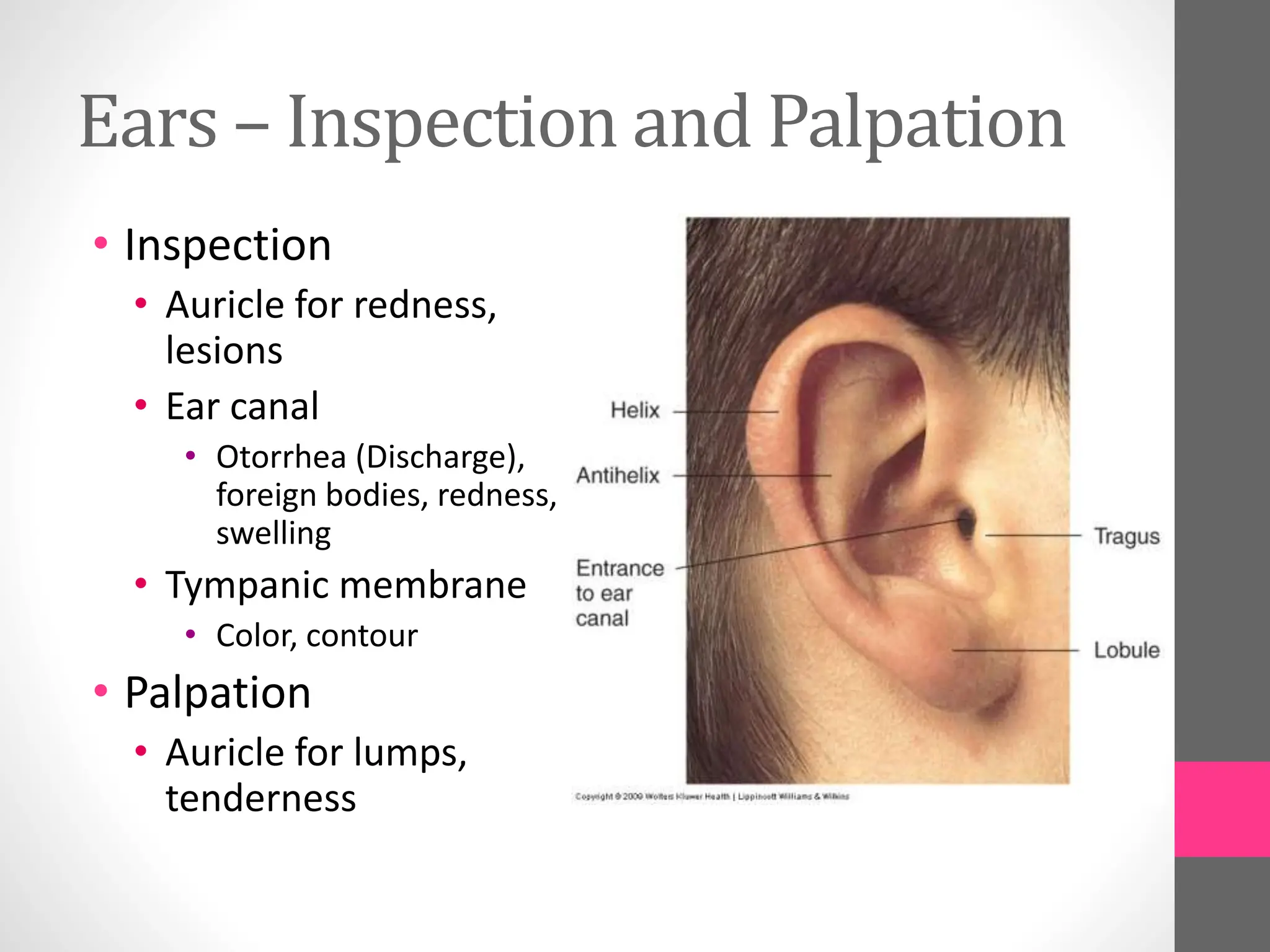
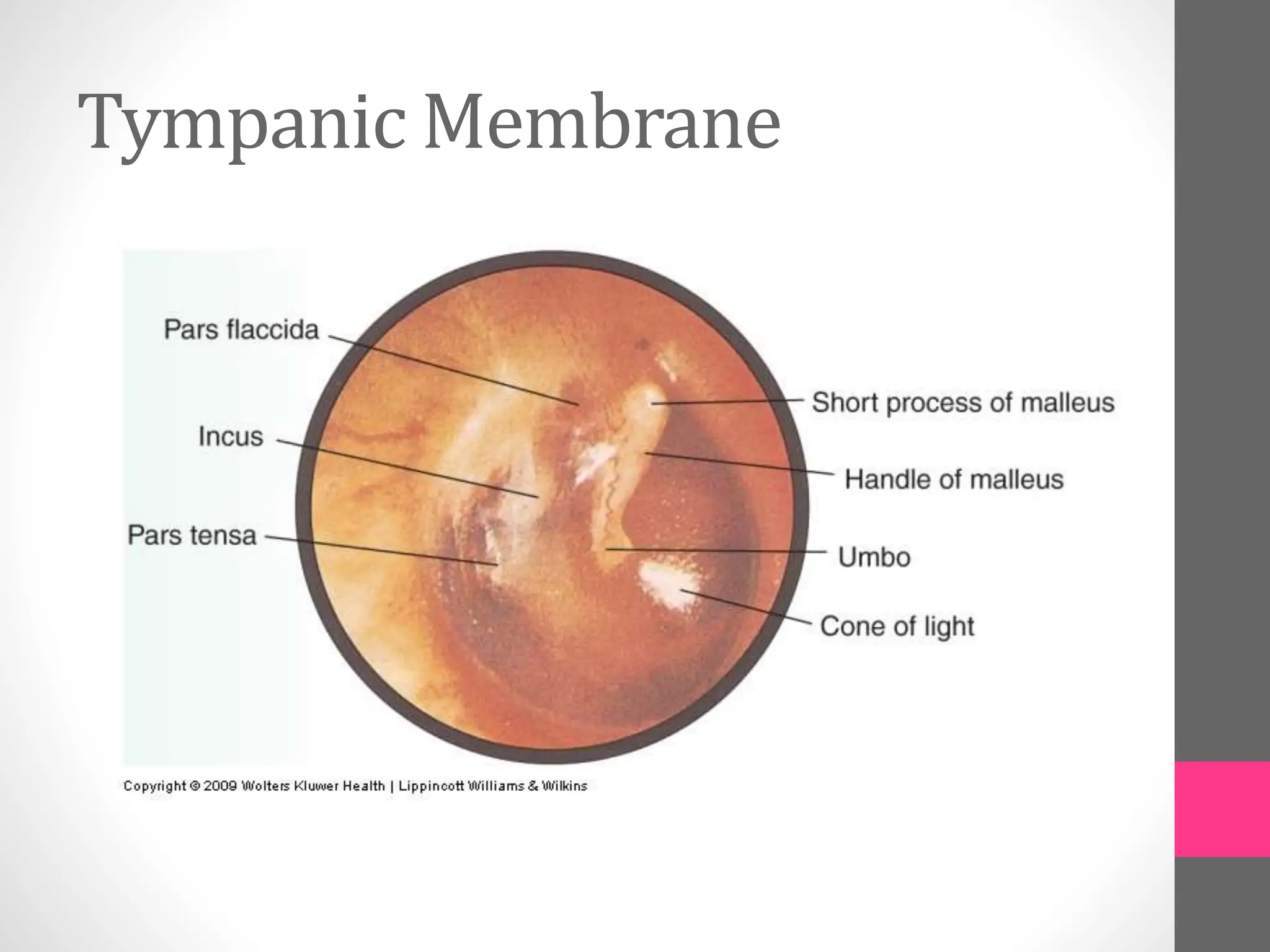
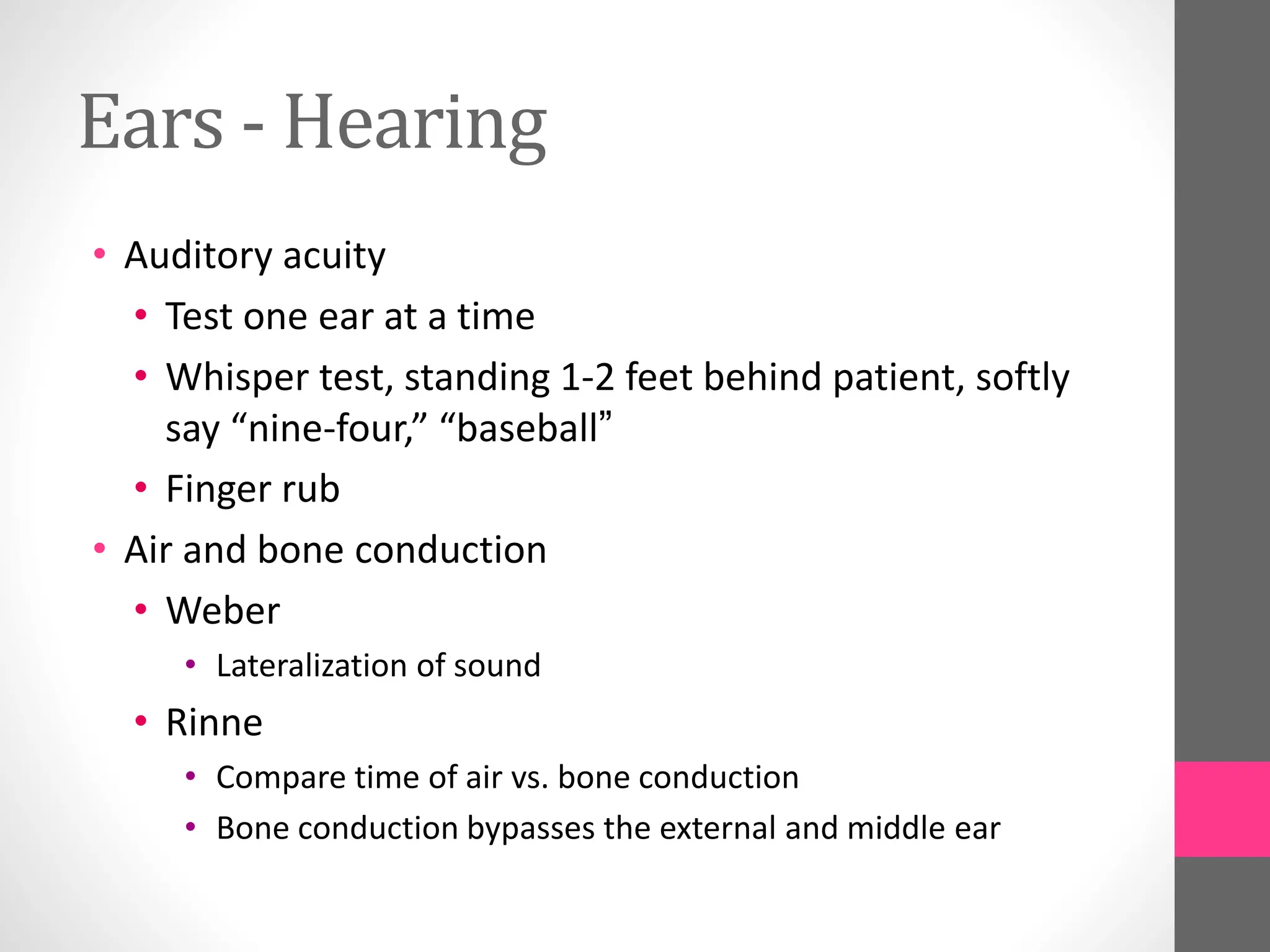
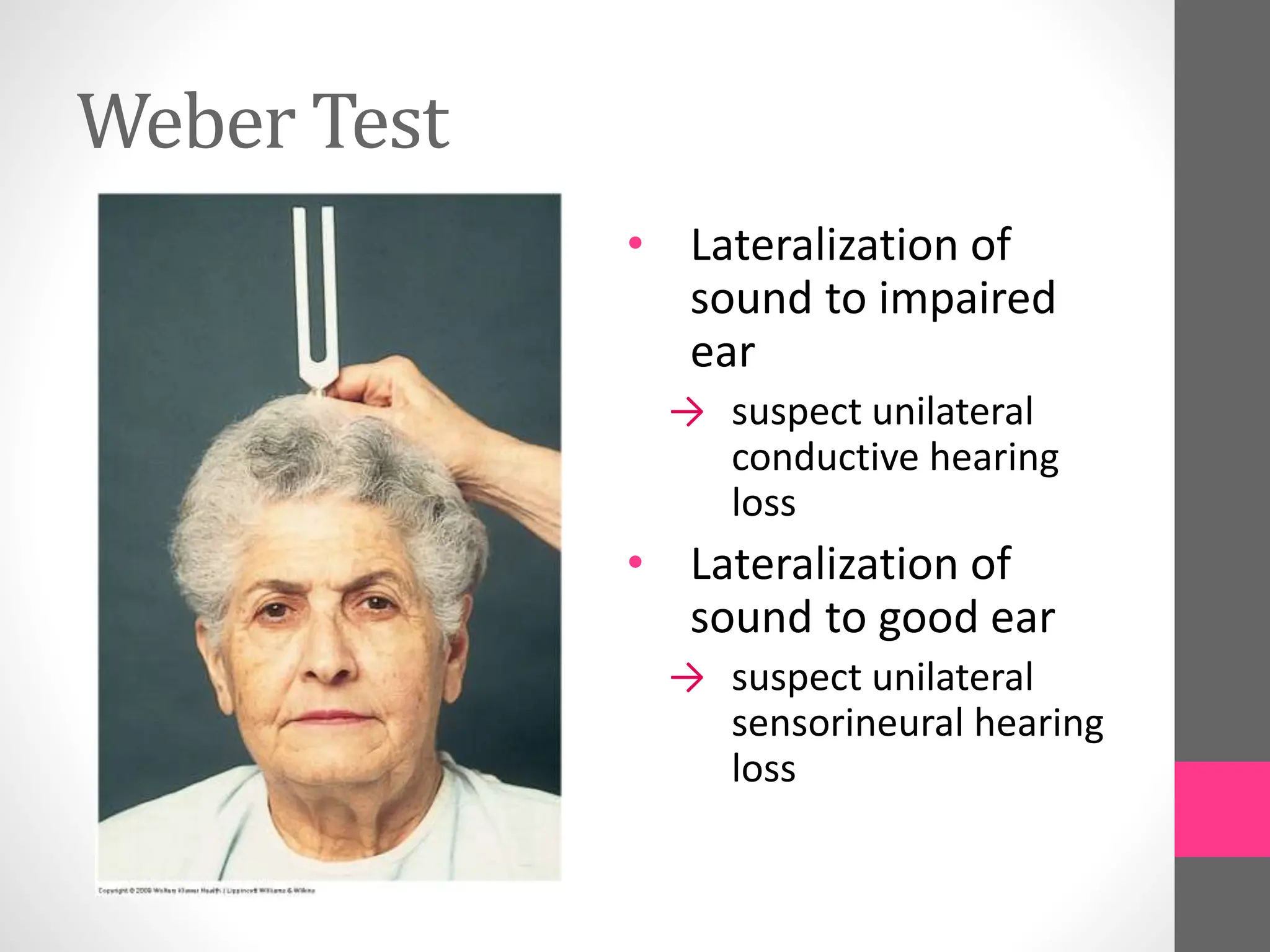
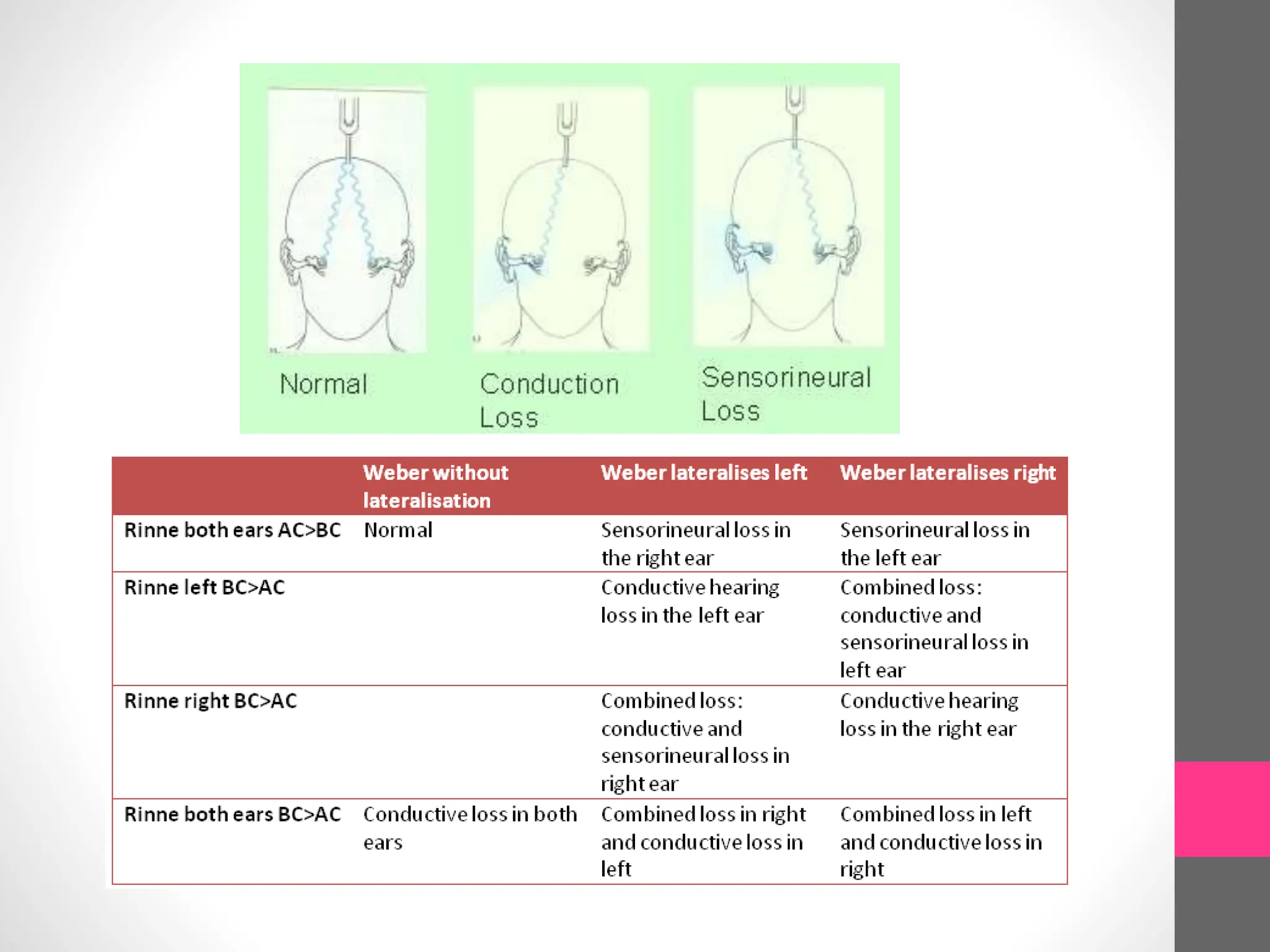
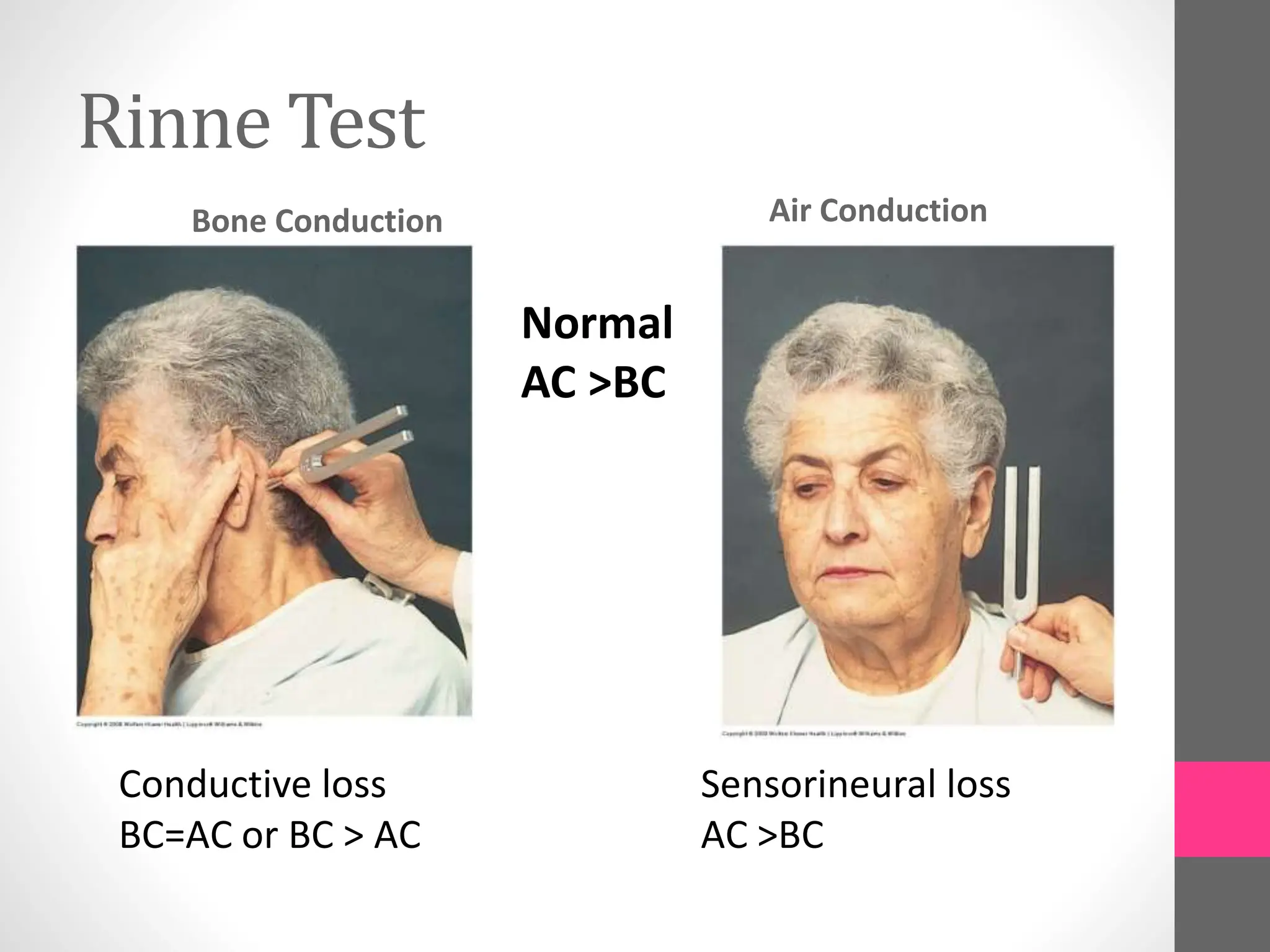
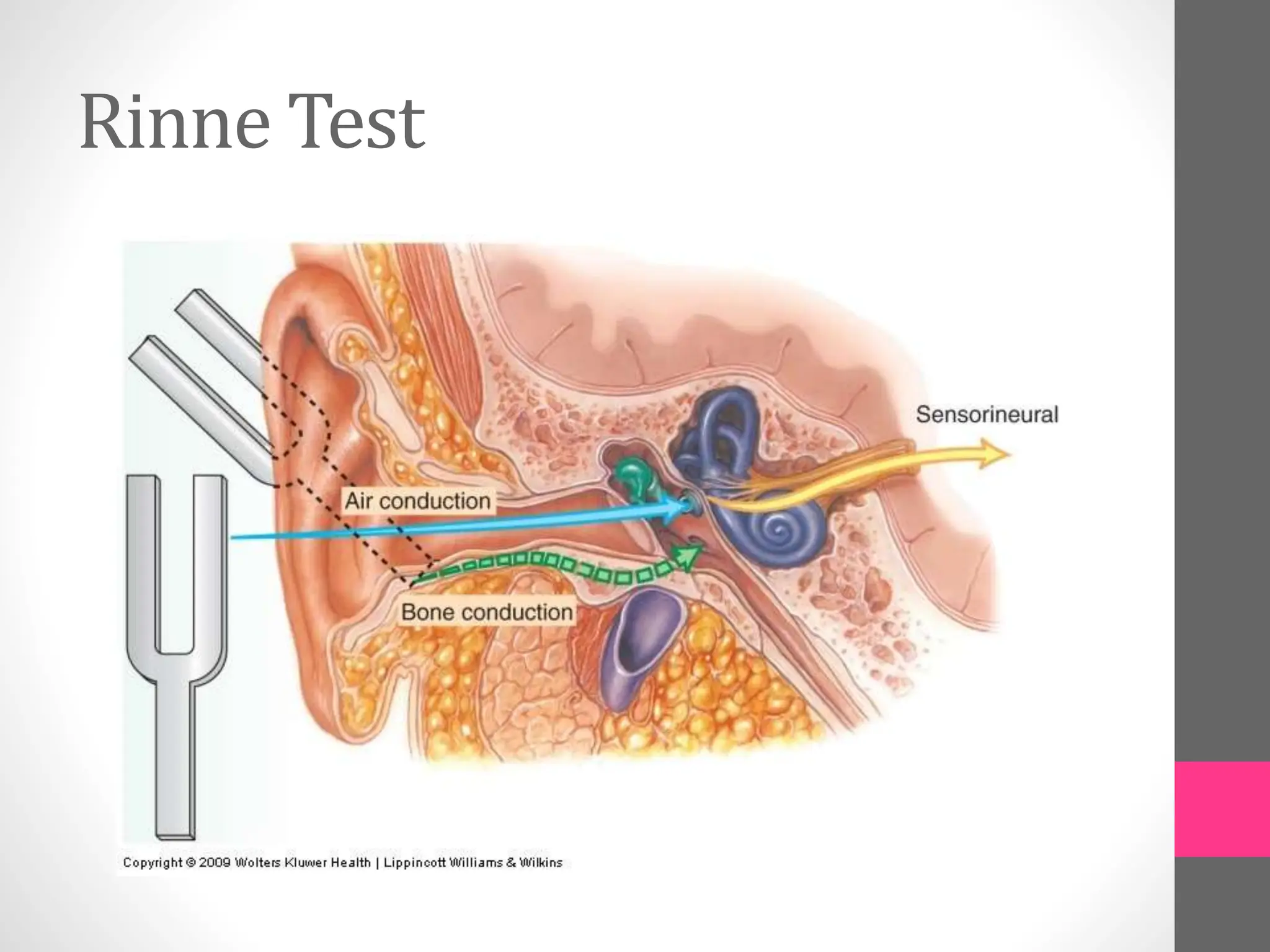
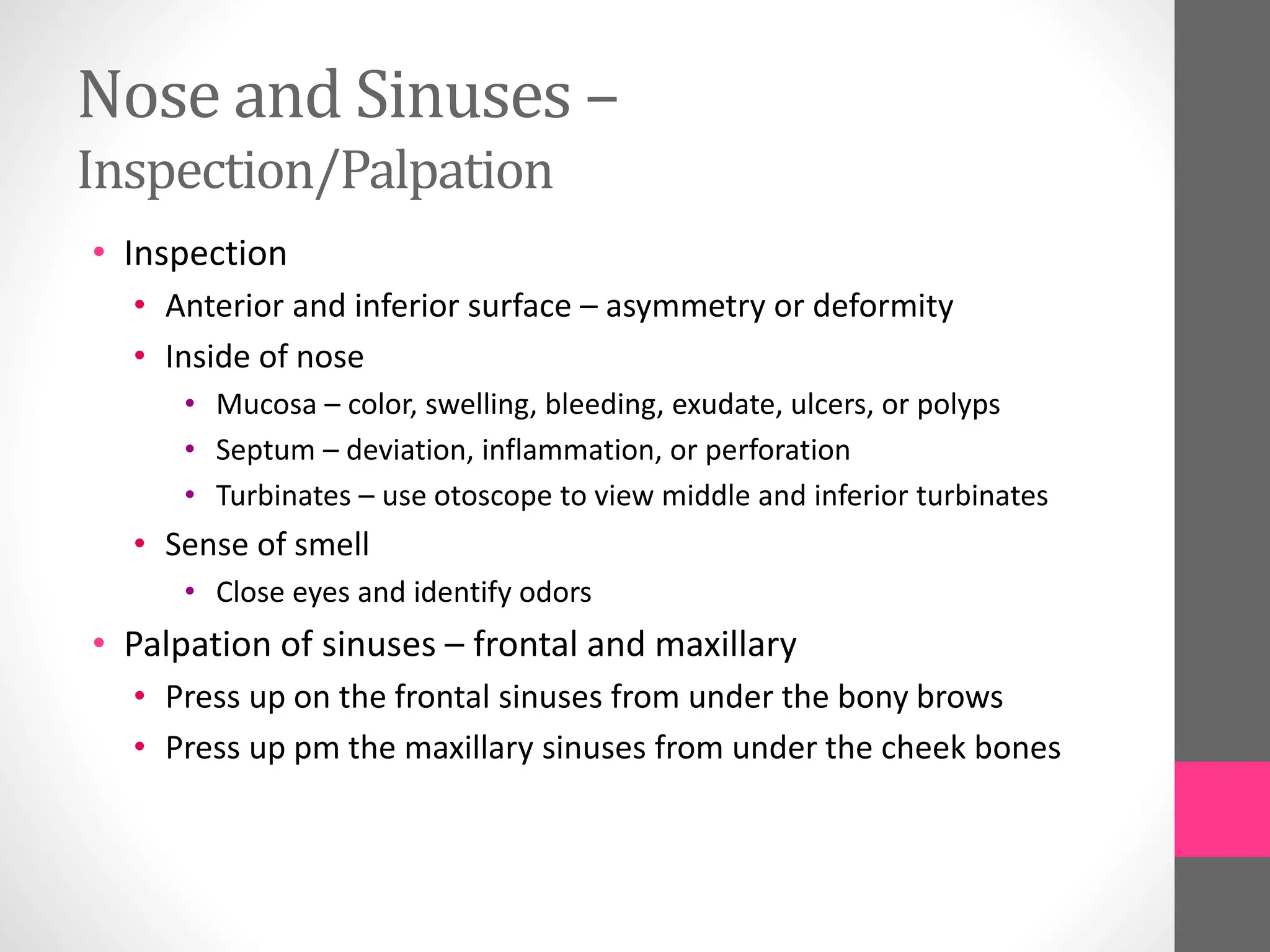
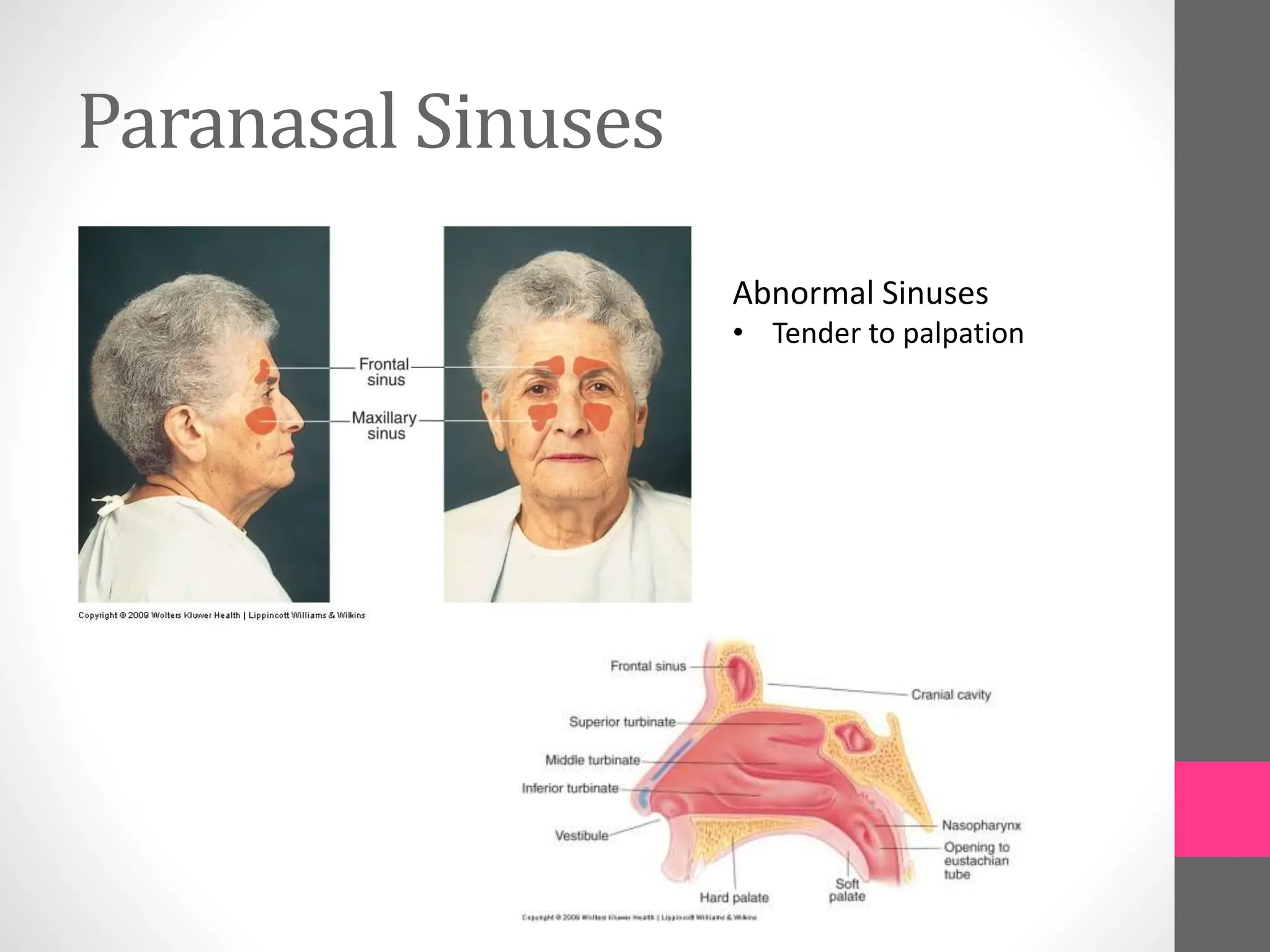
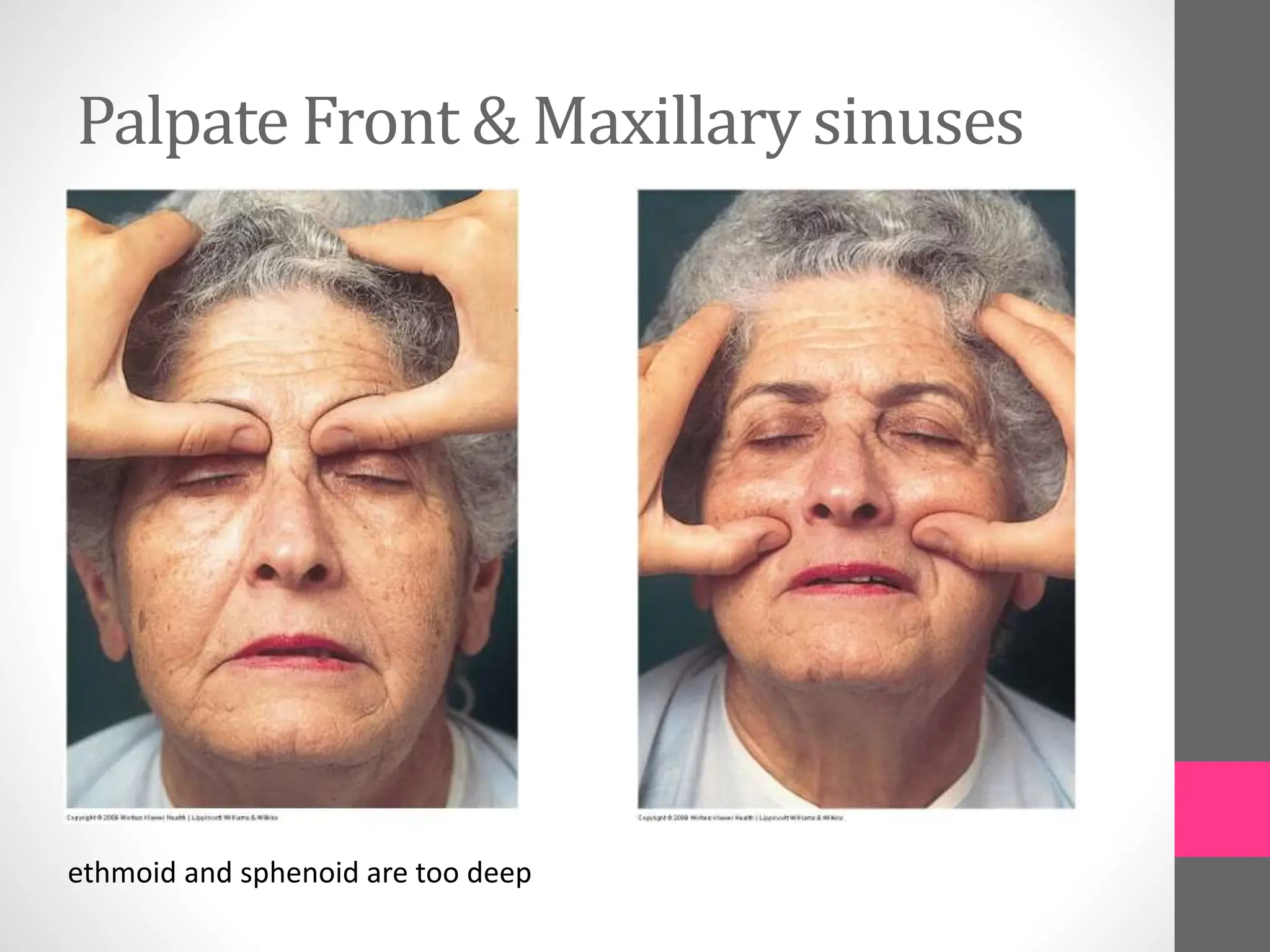
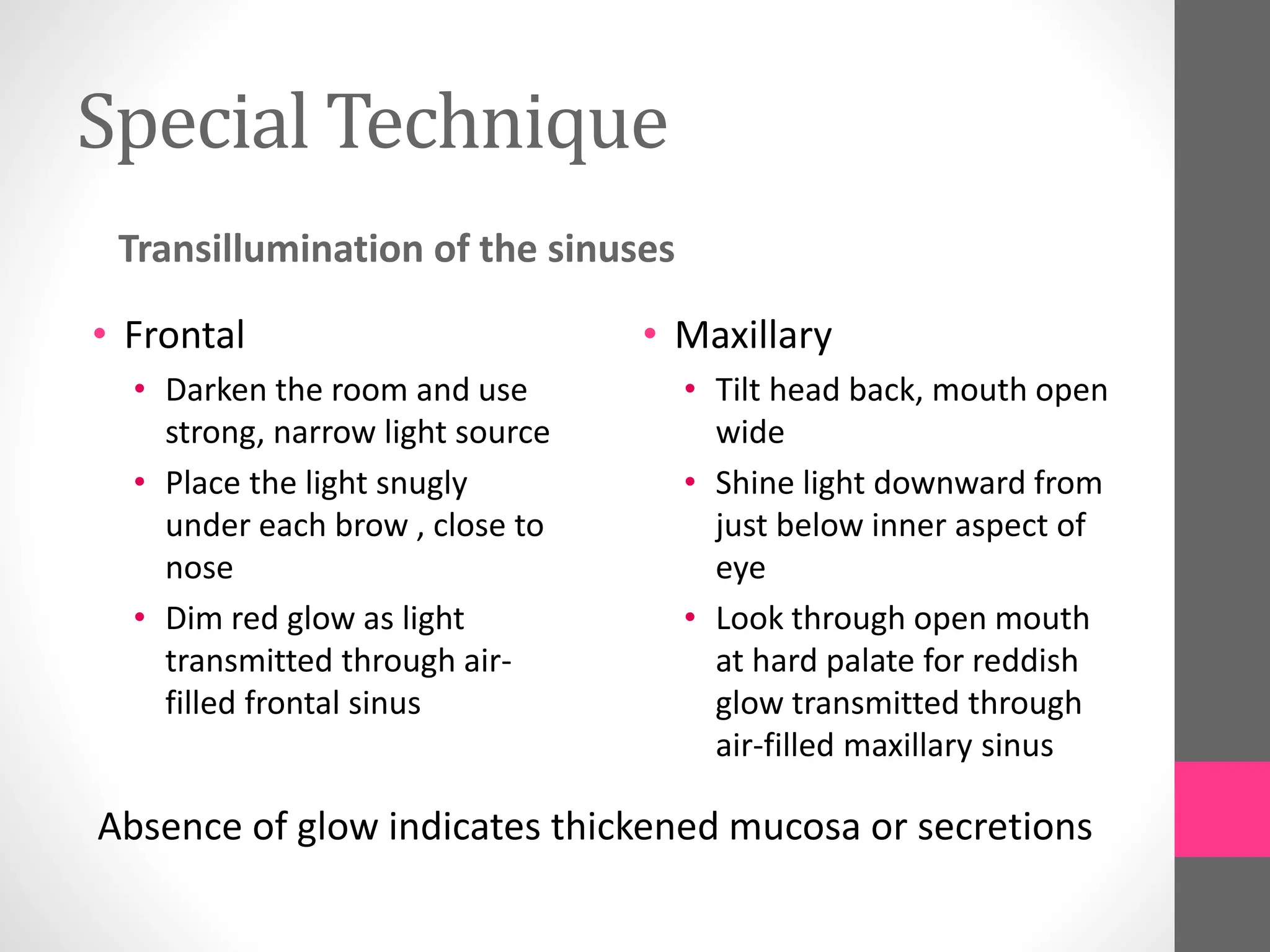
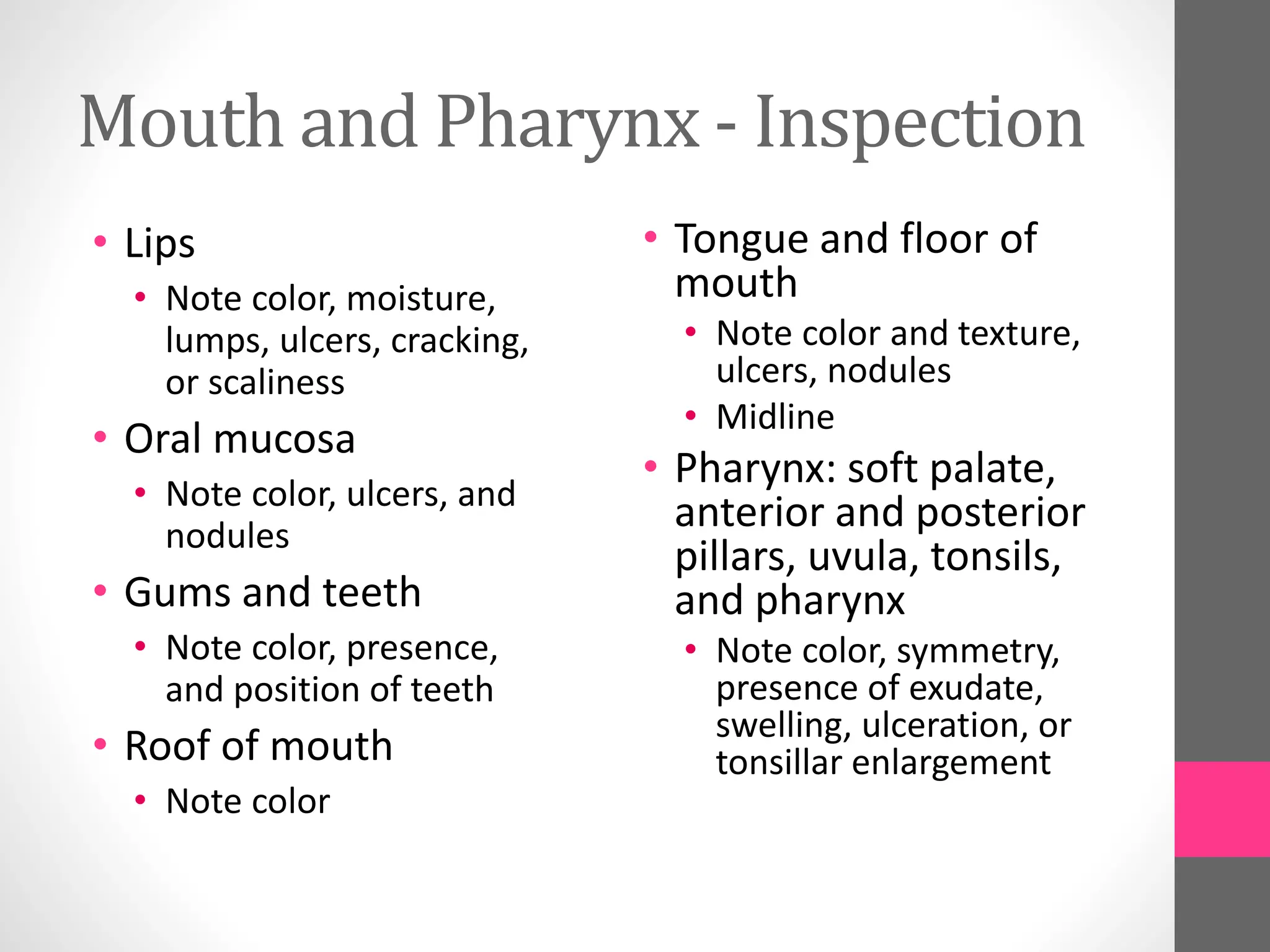
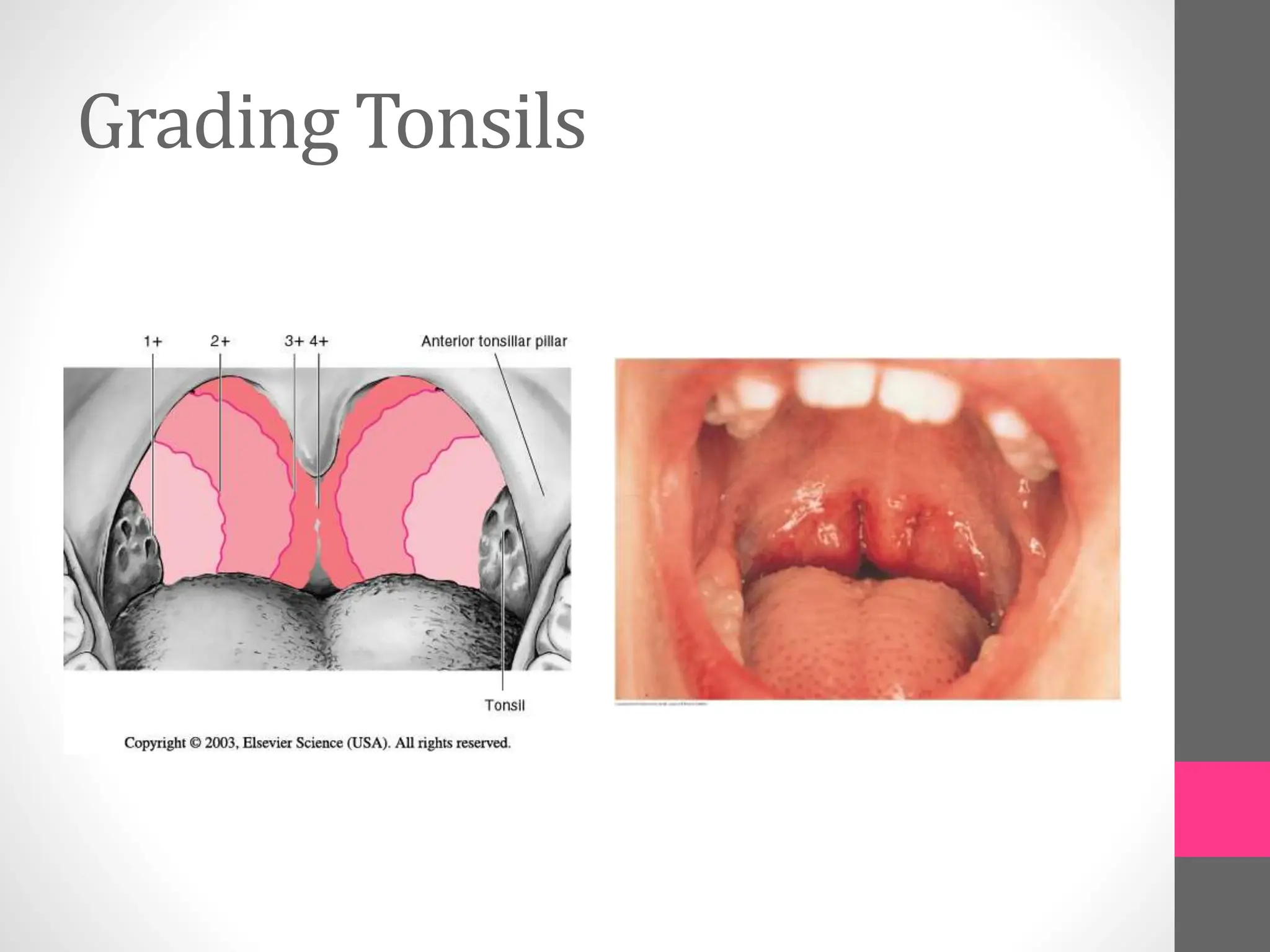
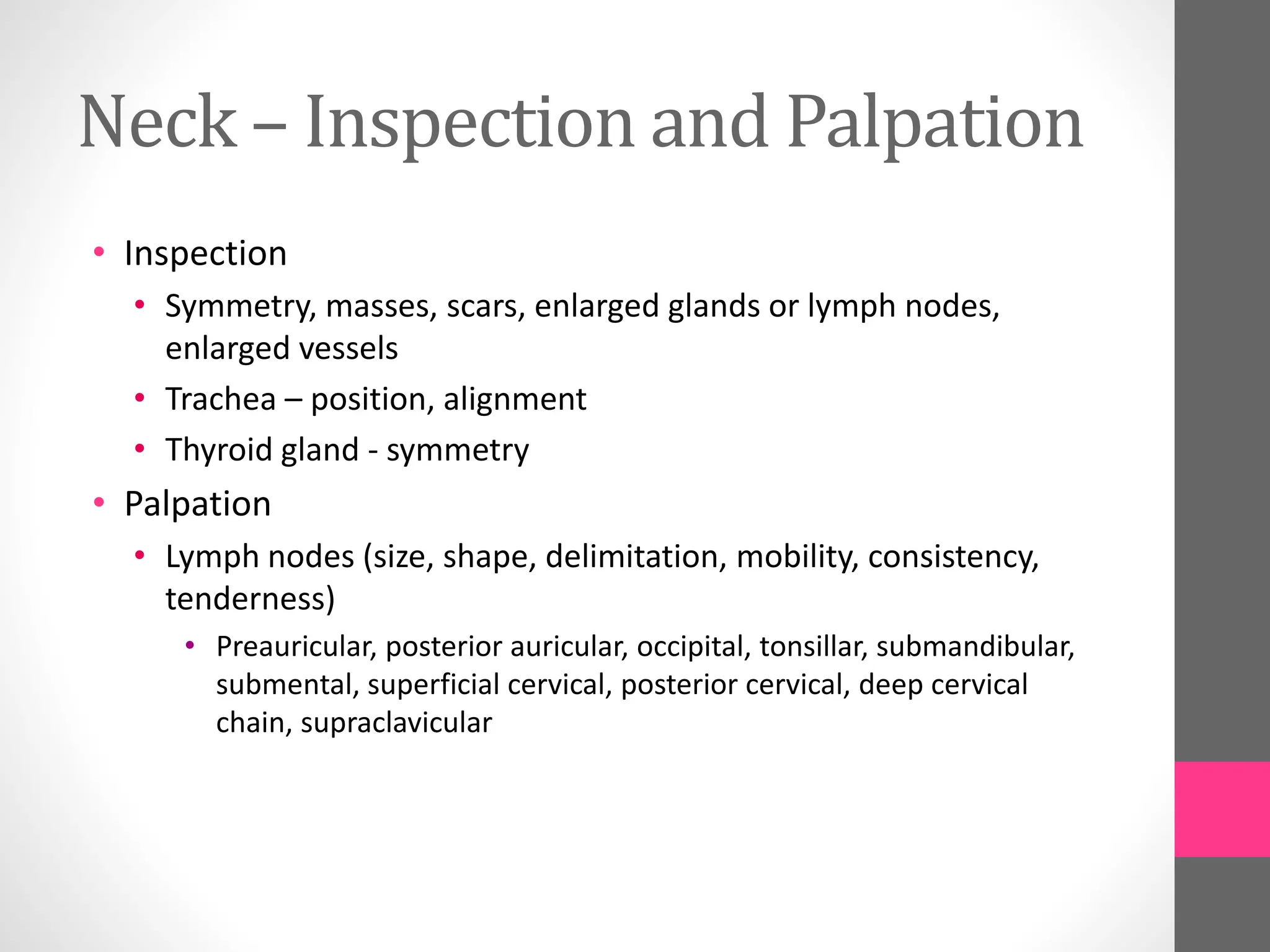
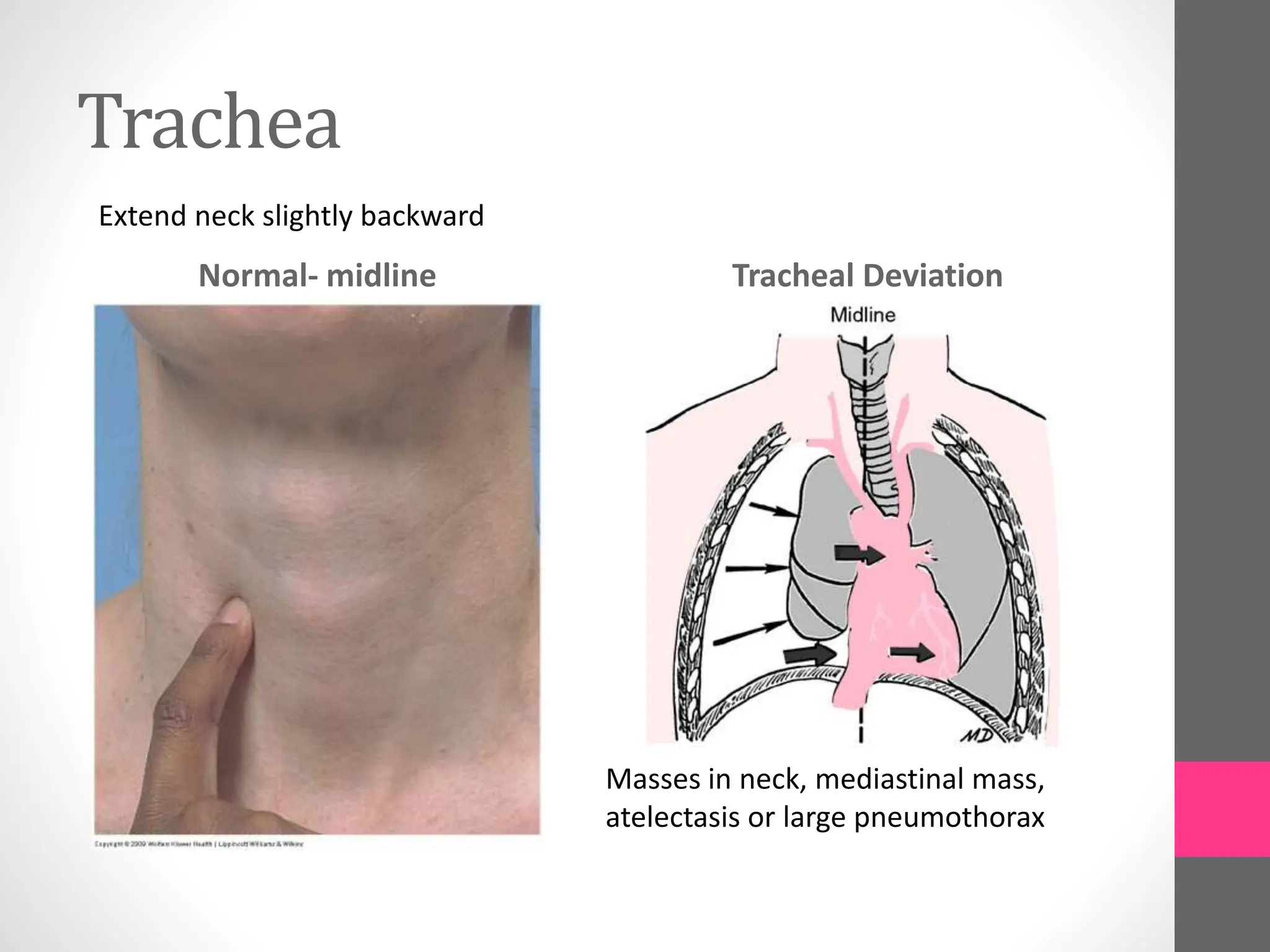
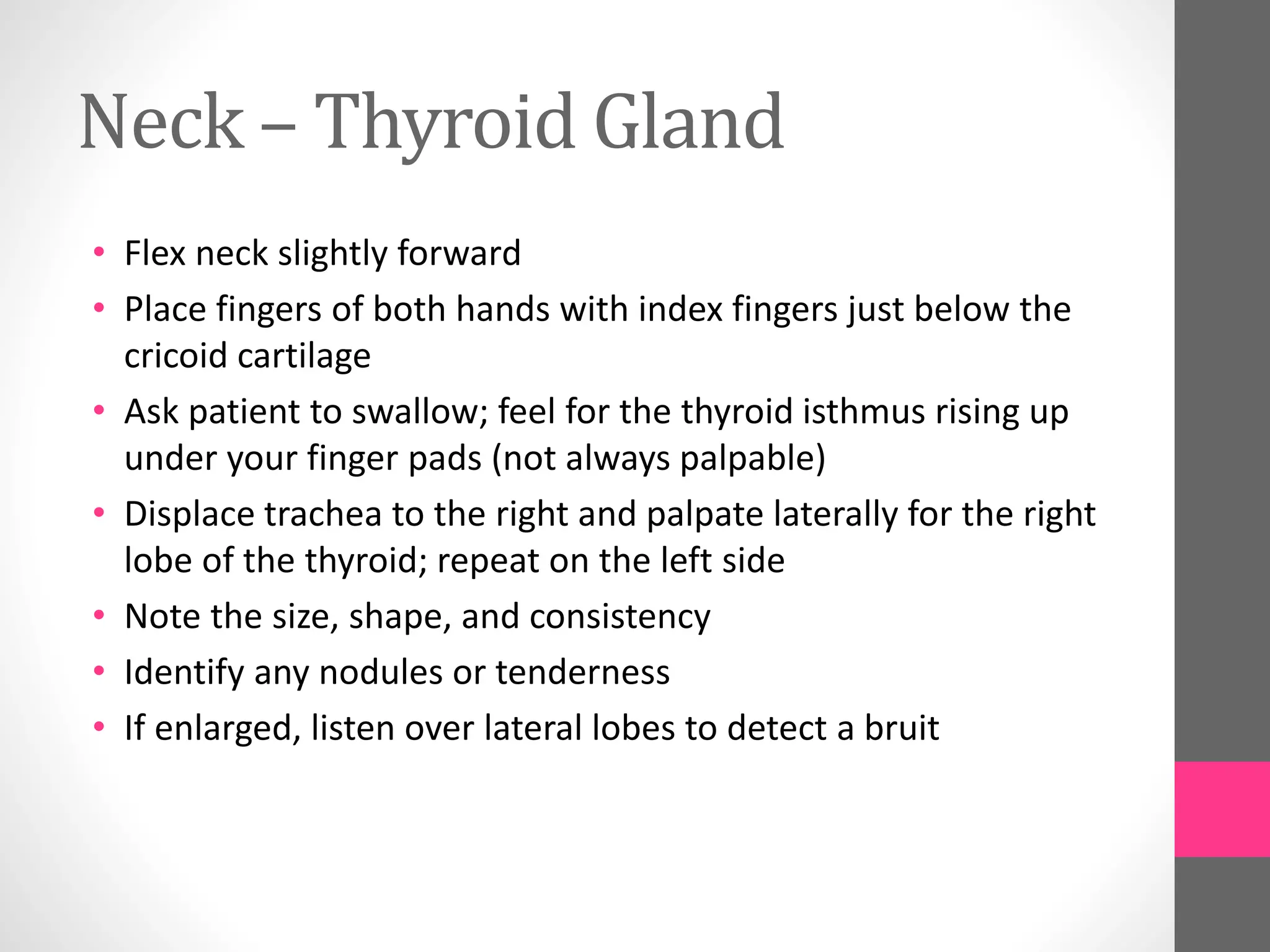
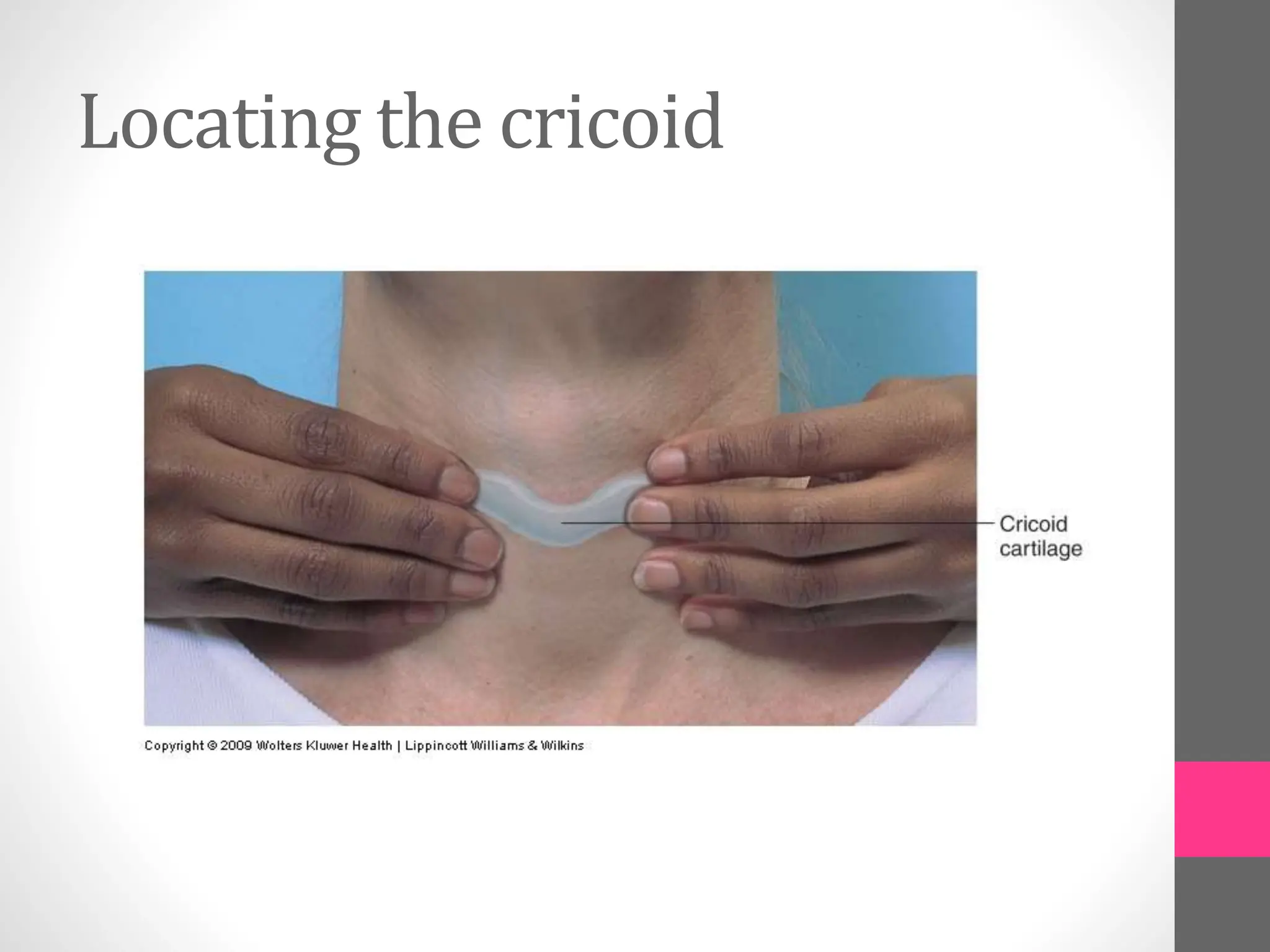
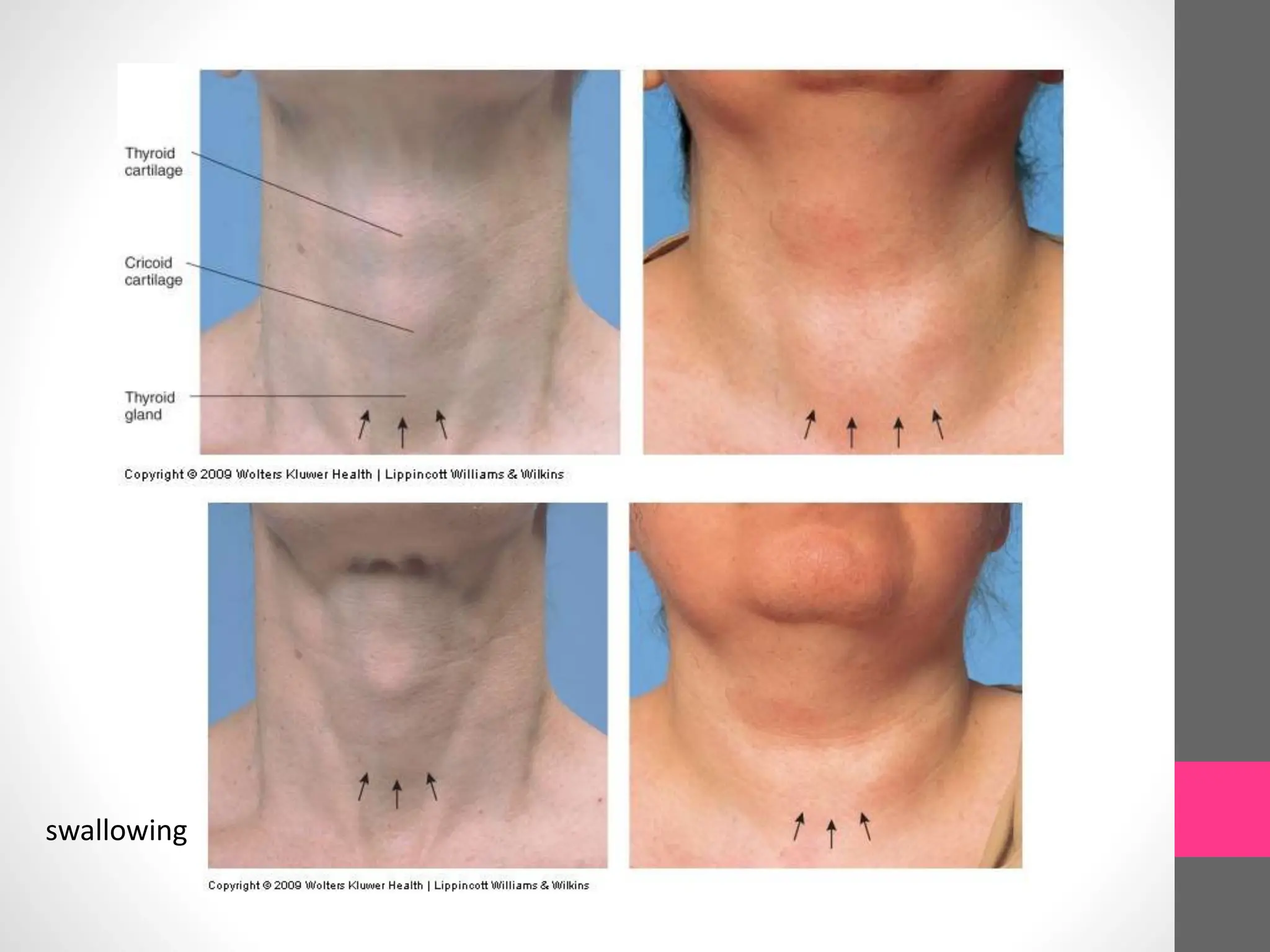
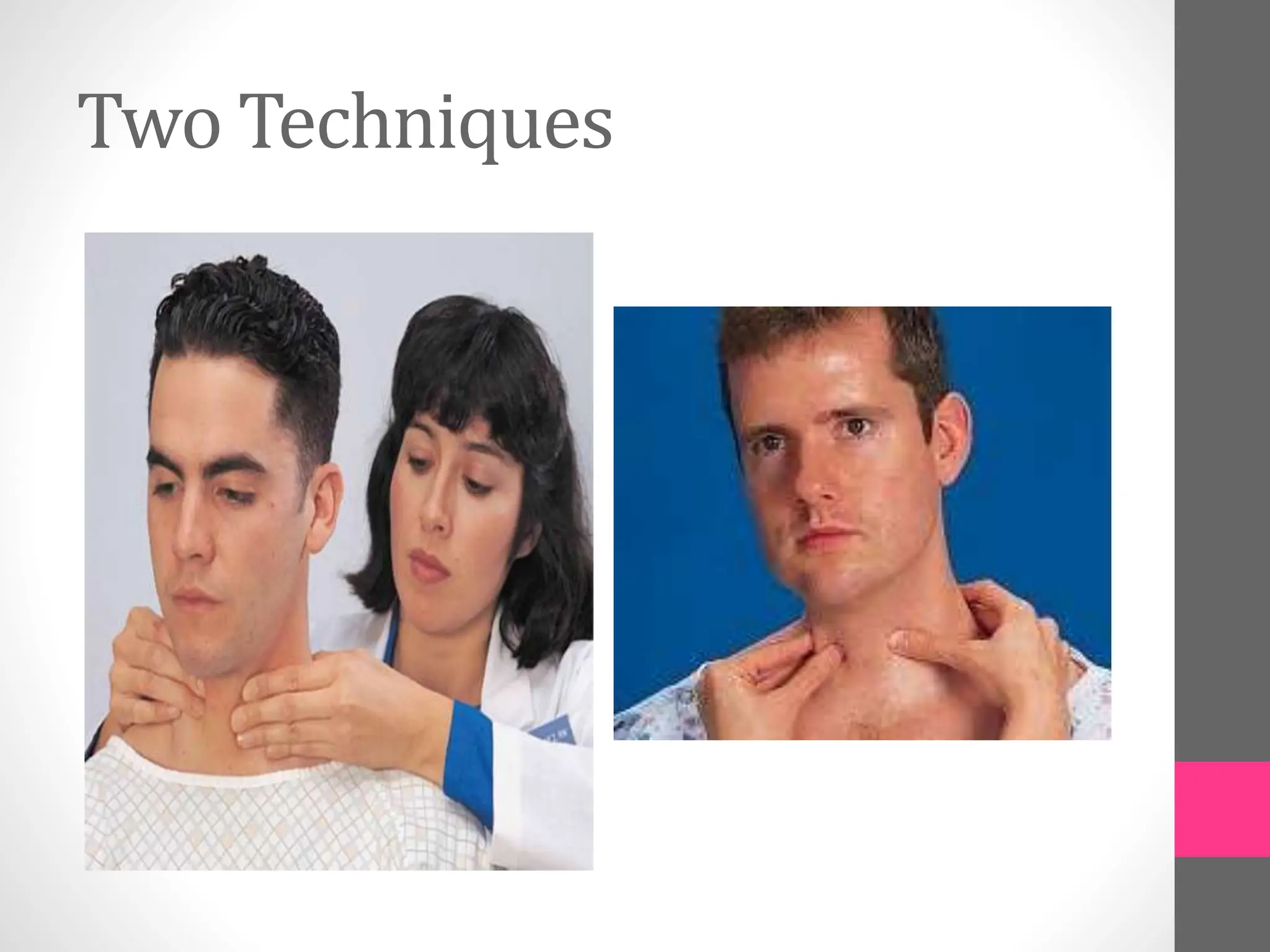
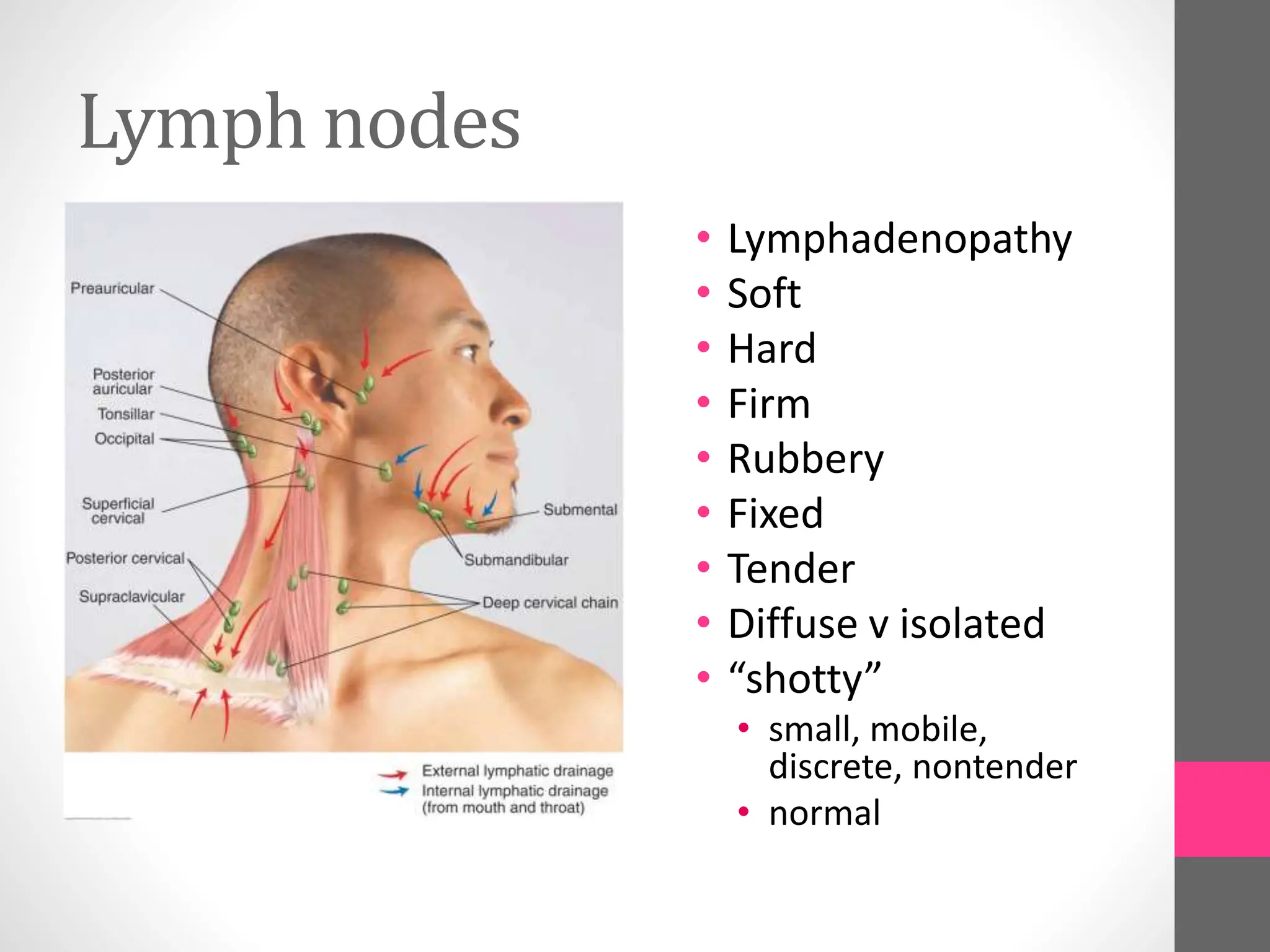
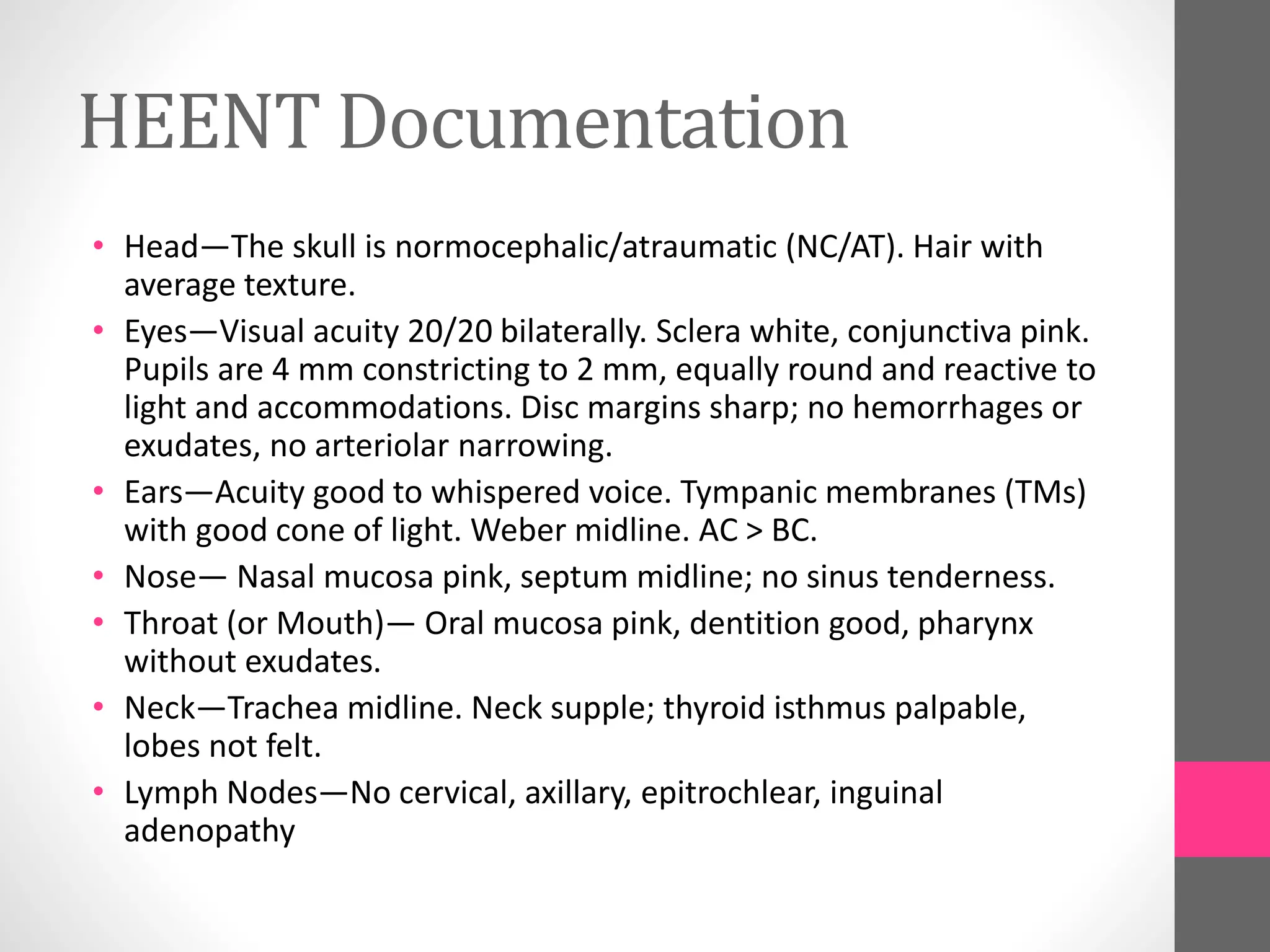
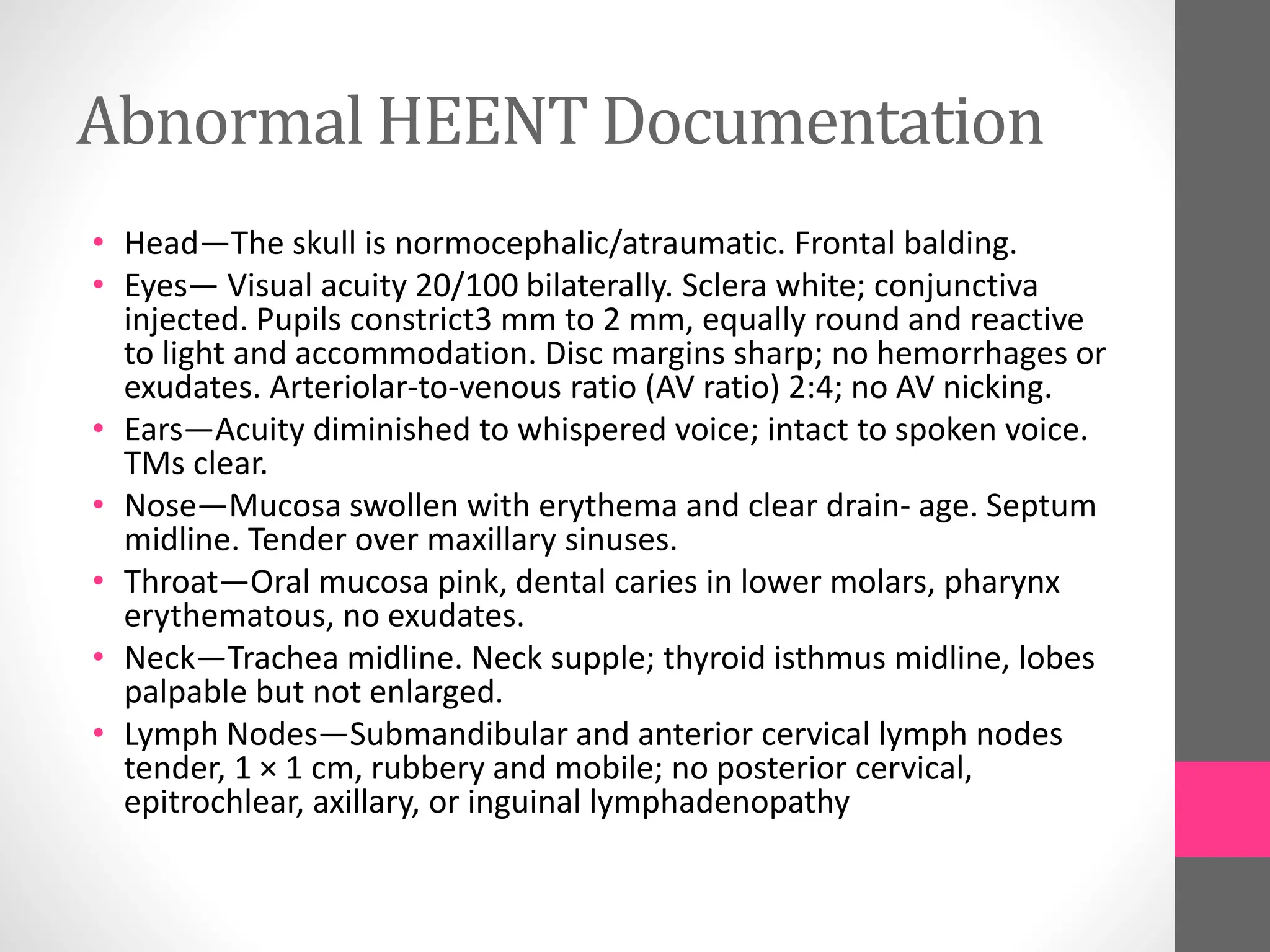
1. Techniques are described for examining each area, including inspection, palpation, relevant history questions and specific tests like visual acuity, visual fields and hearing.
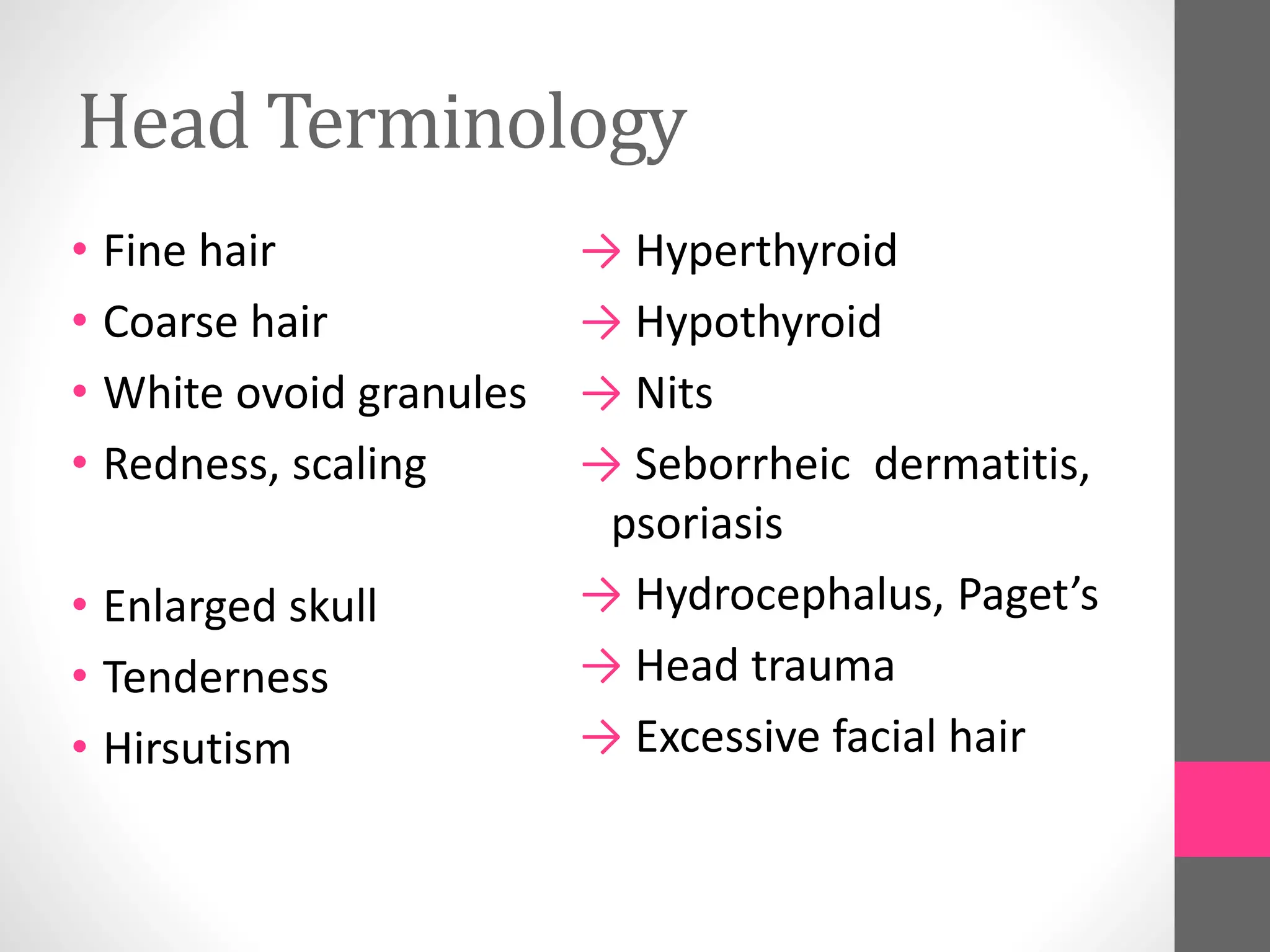
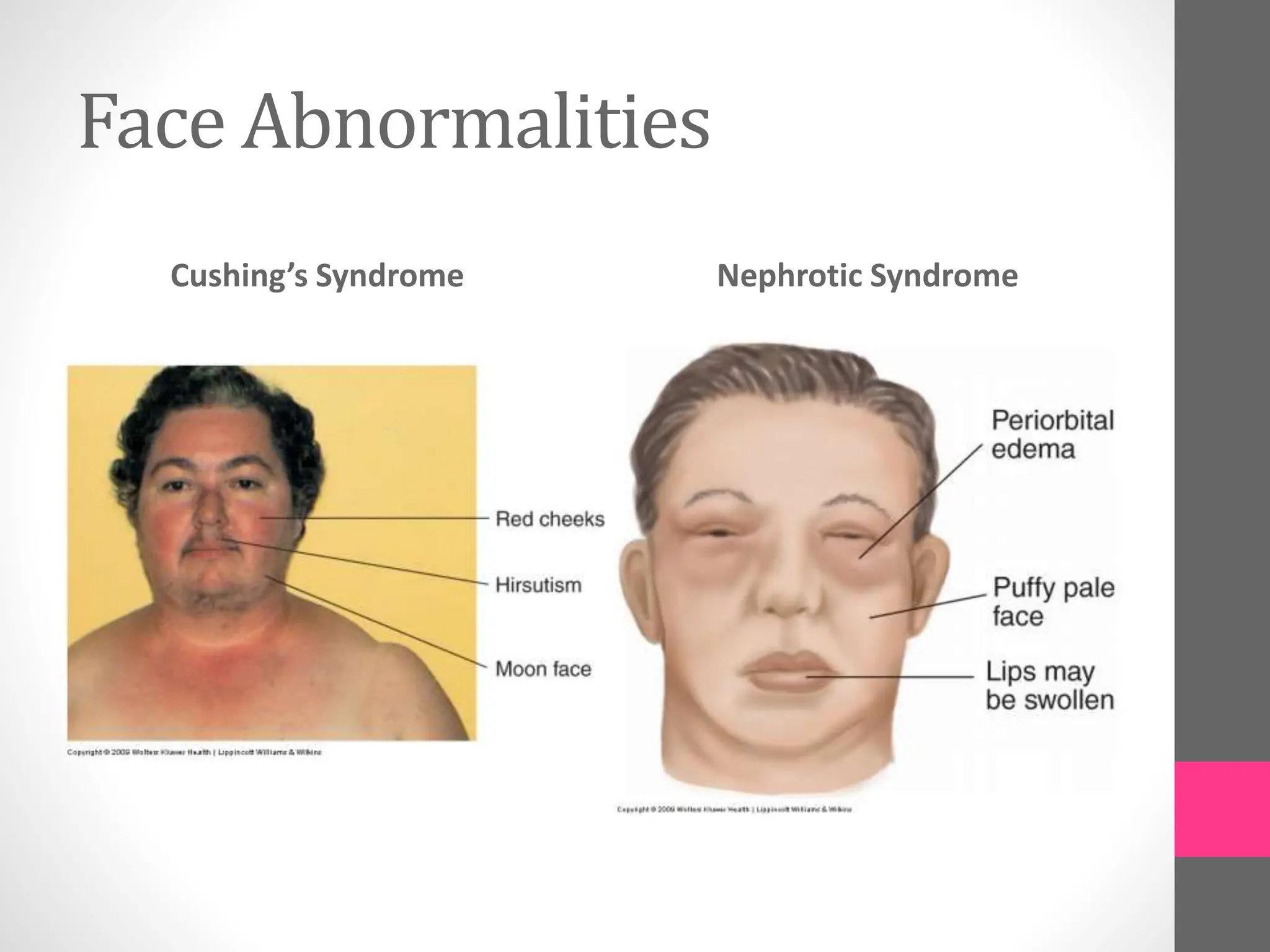
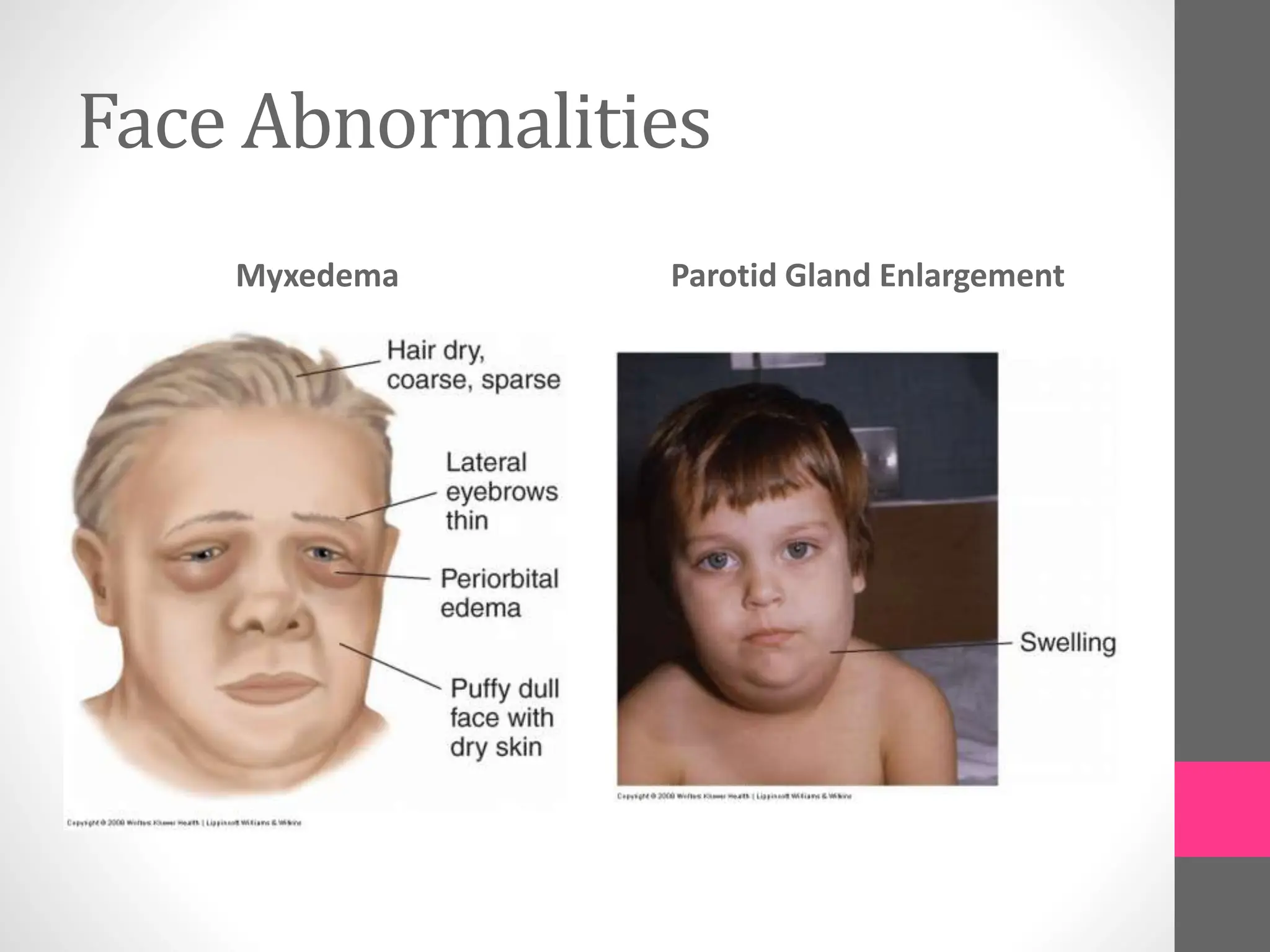
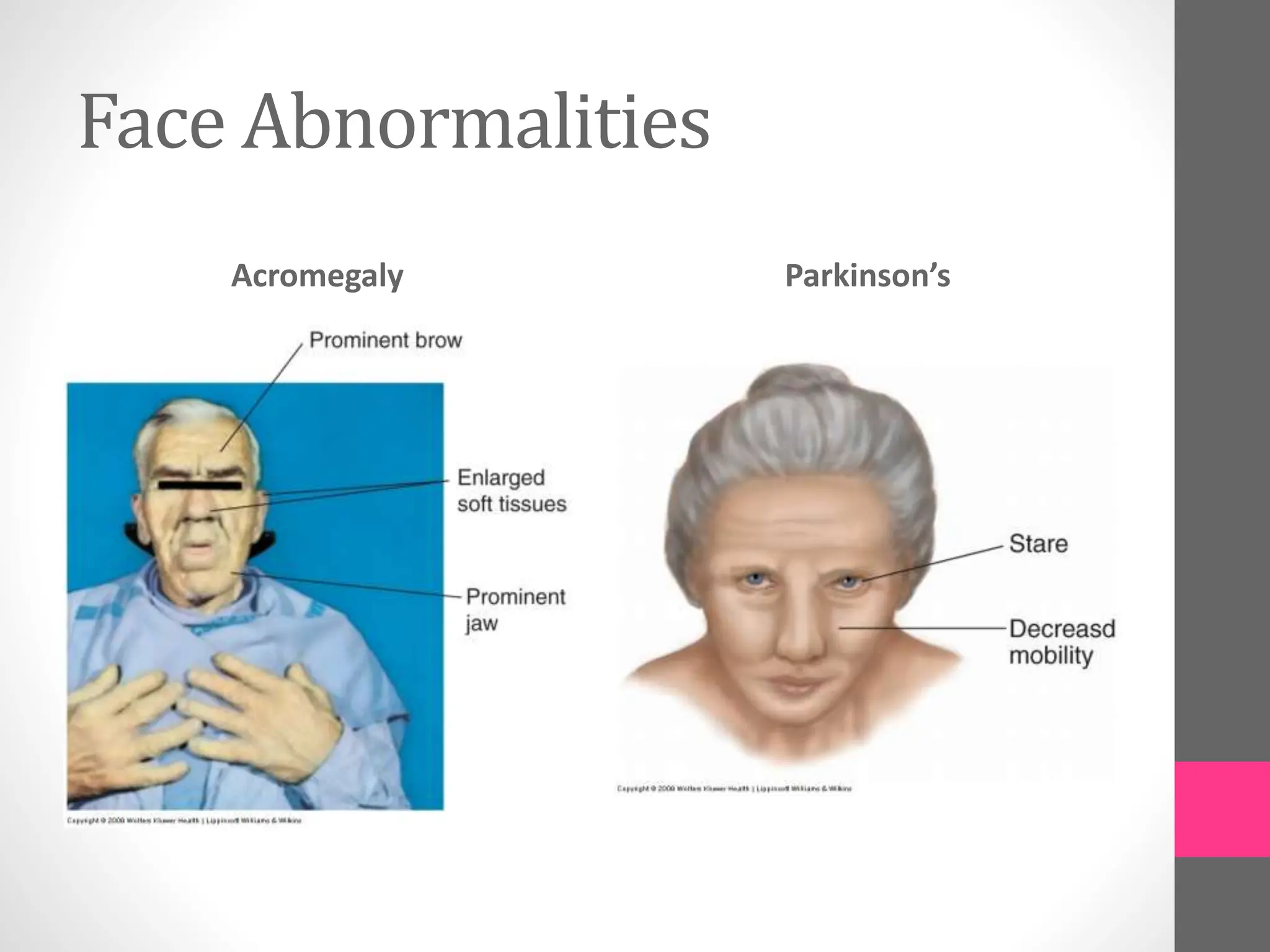
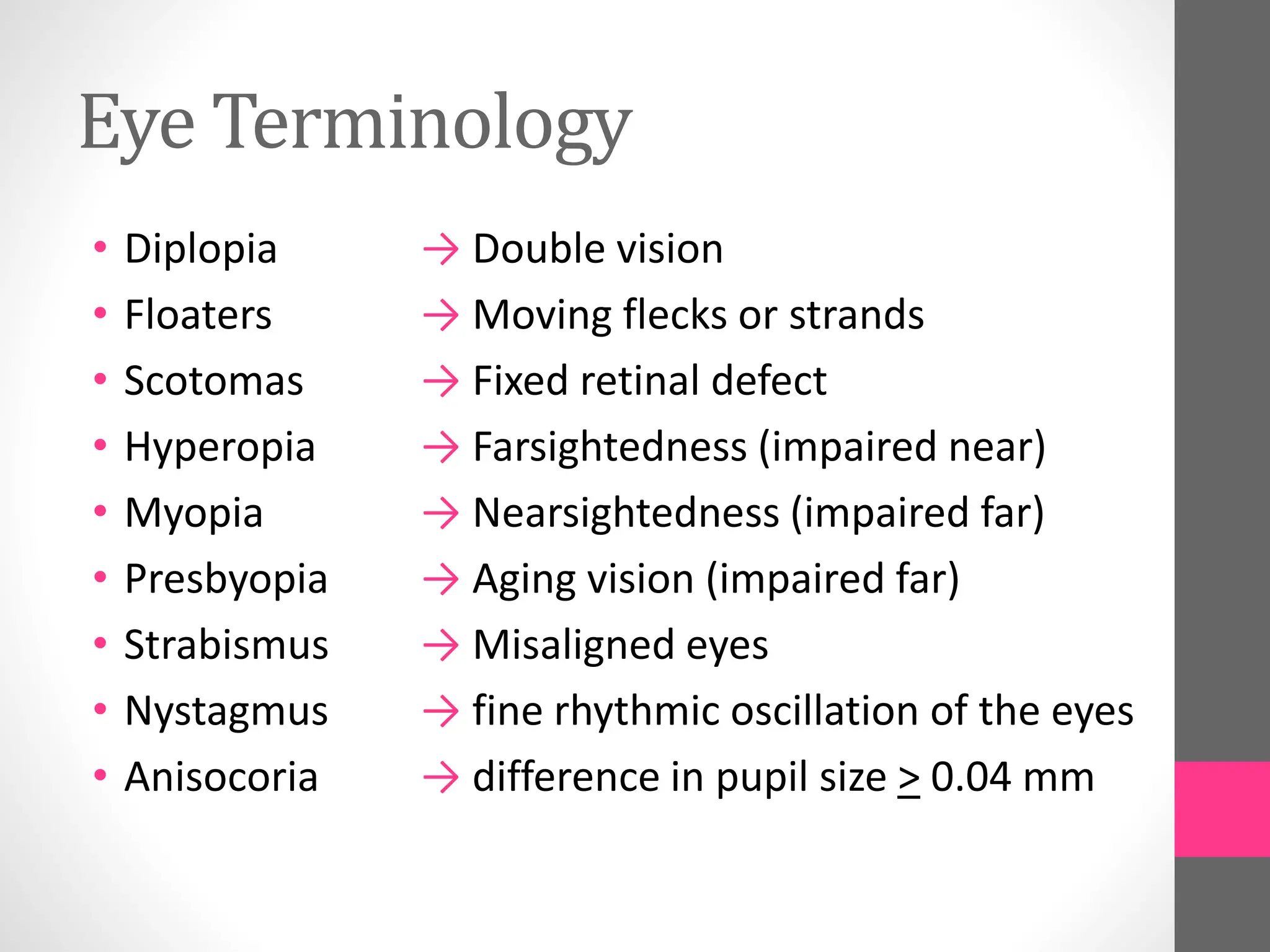
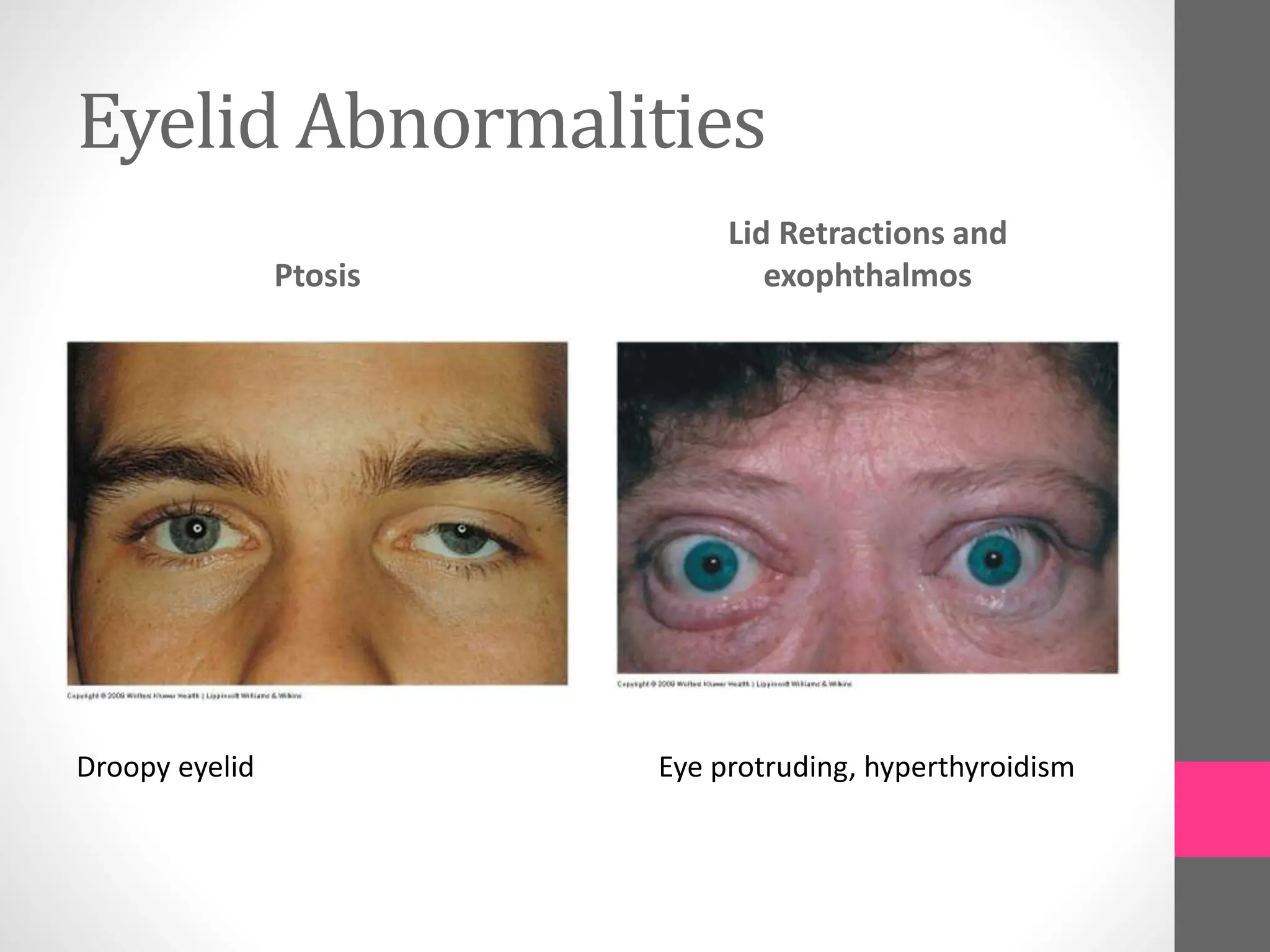
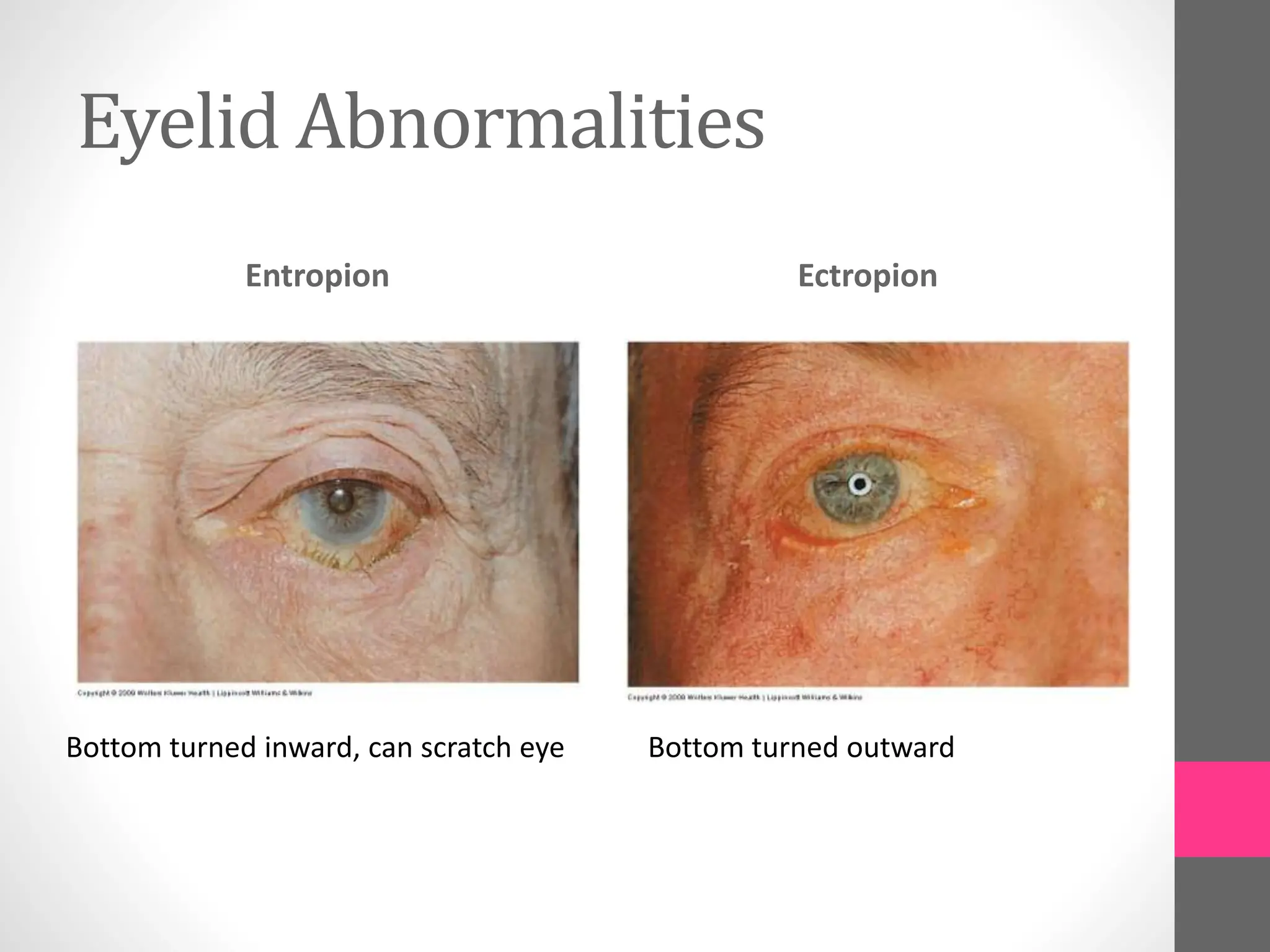
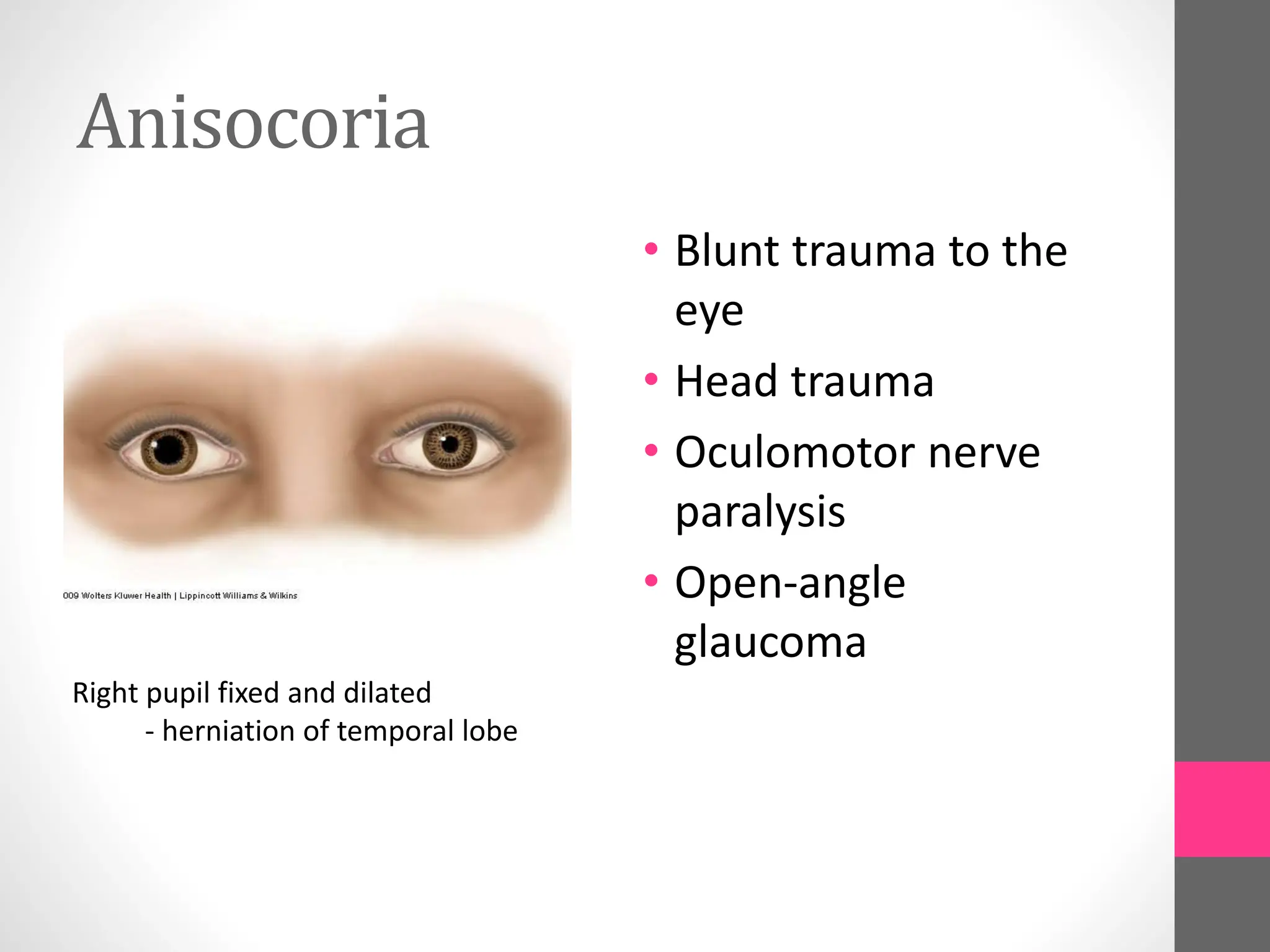
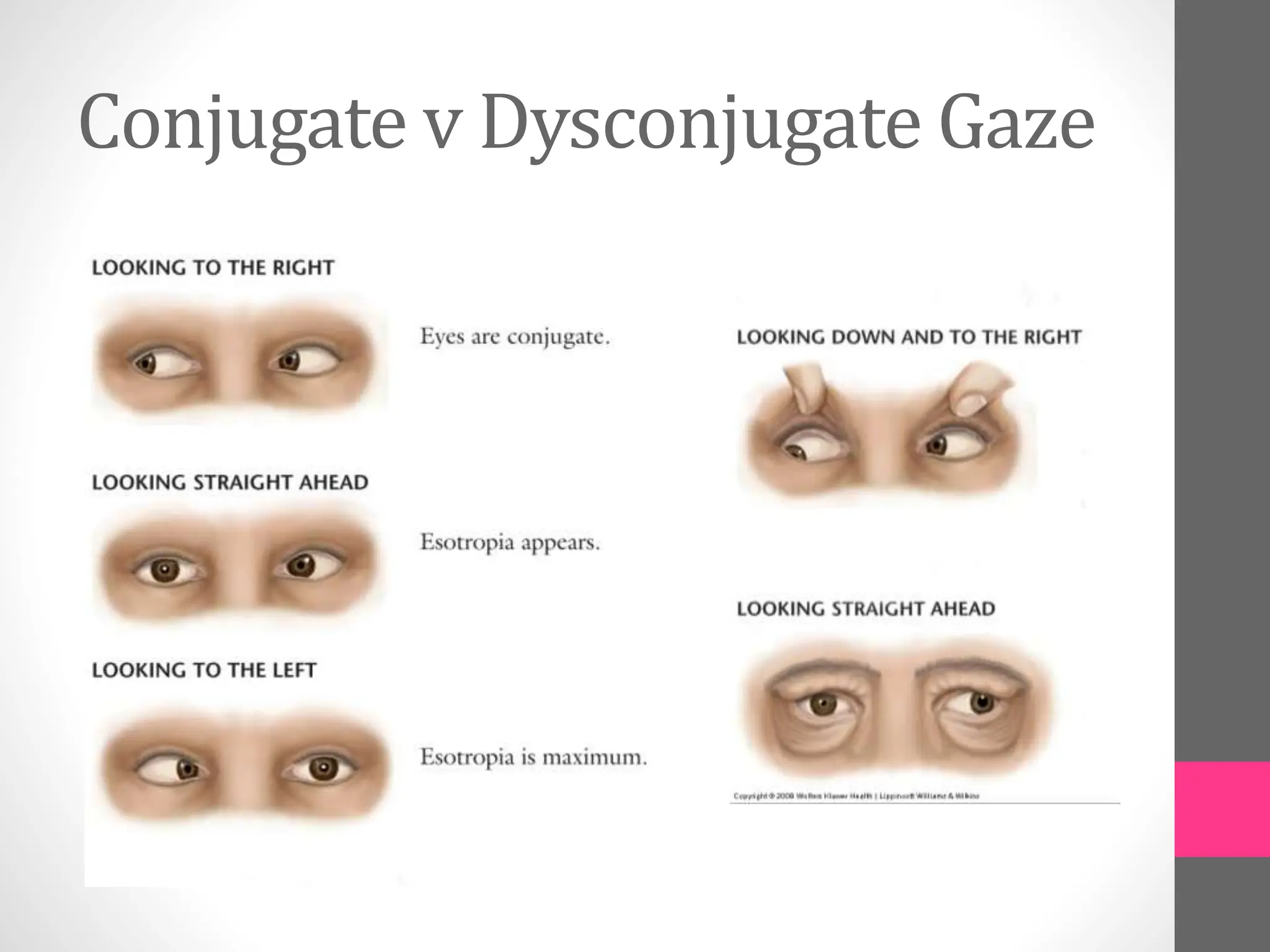
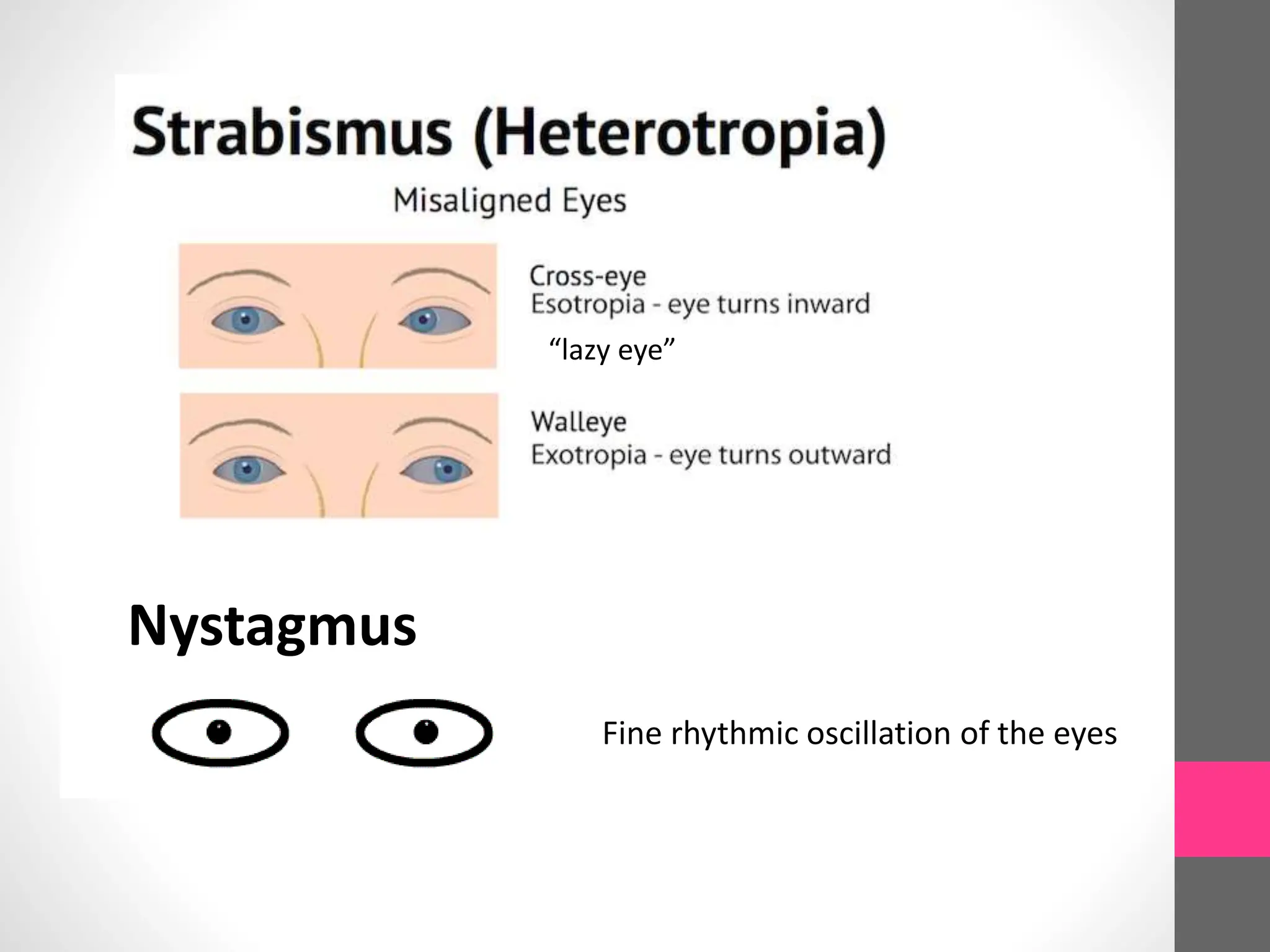
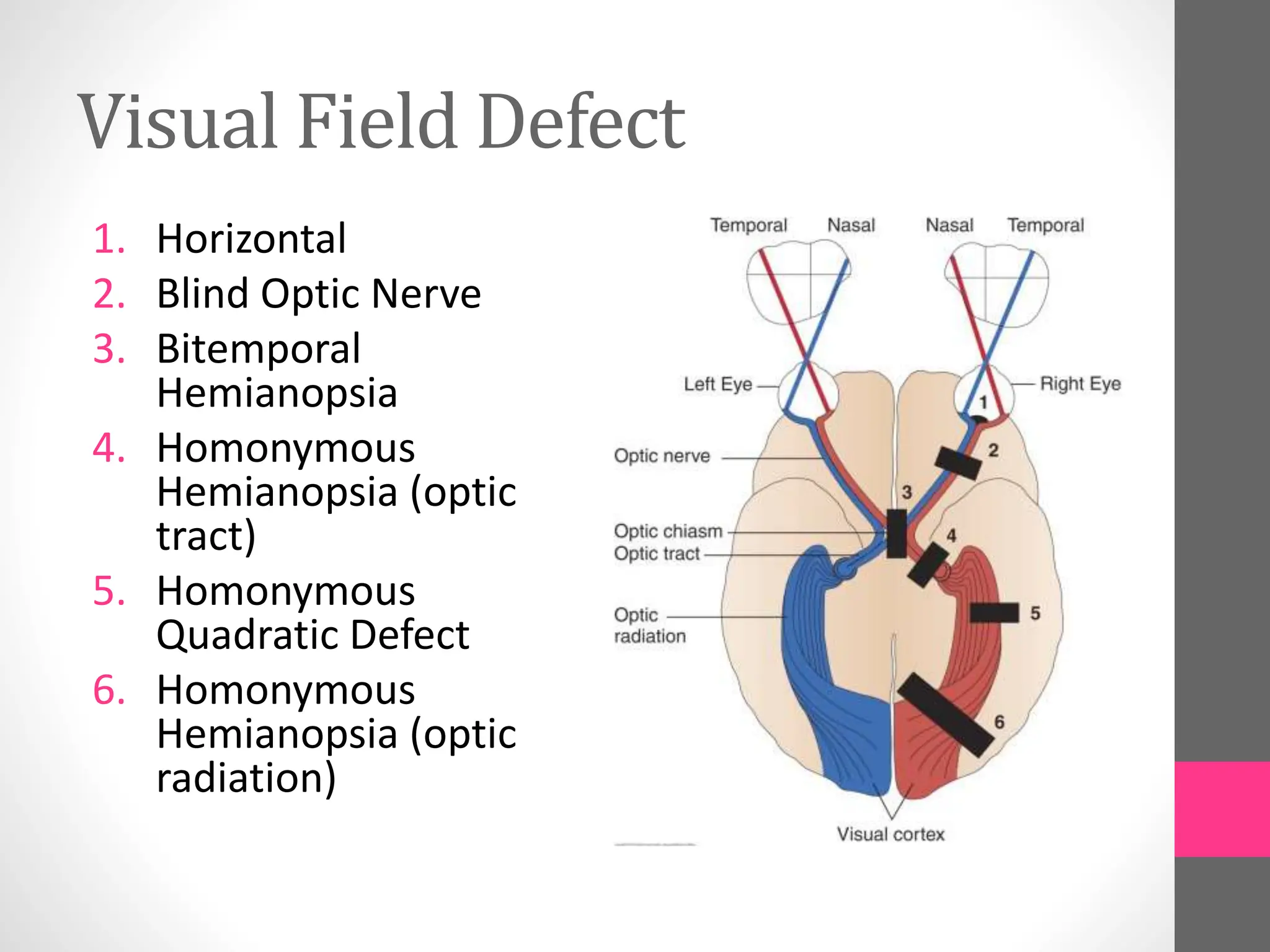
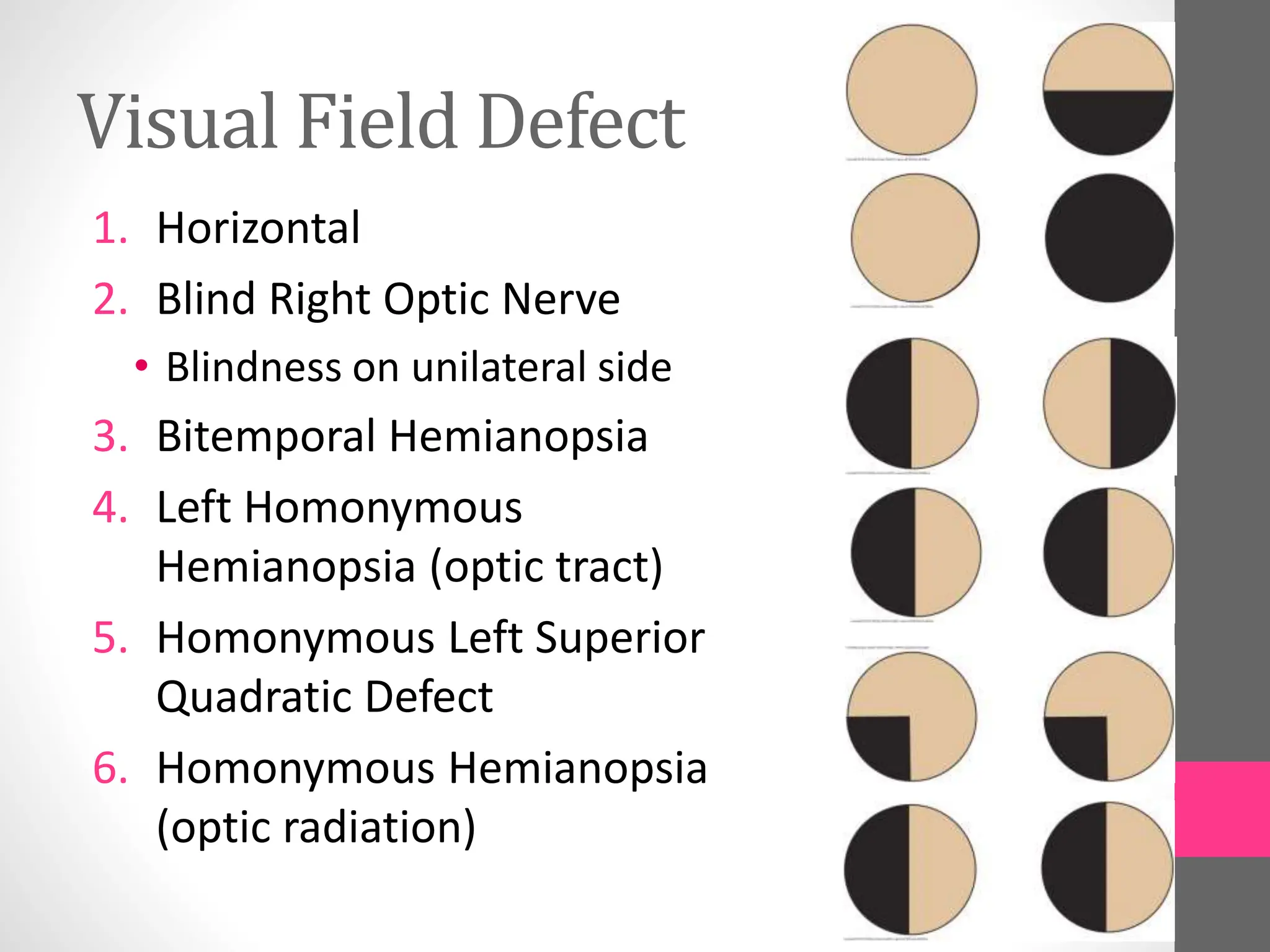
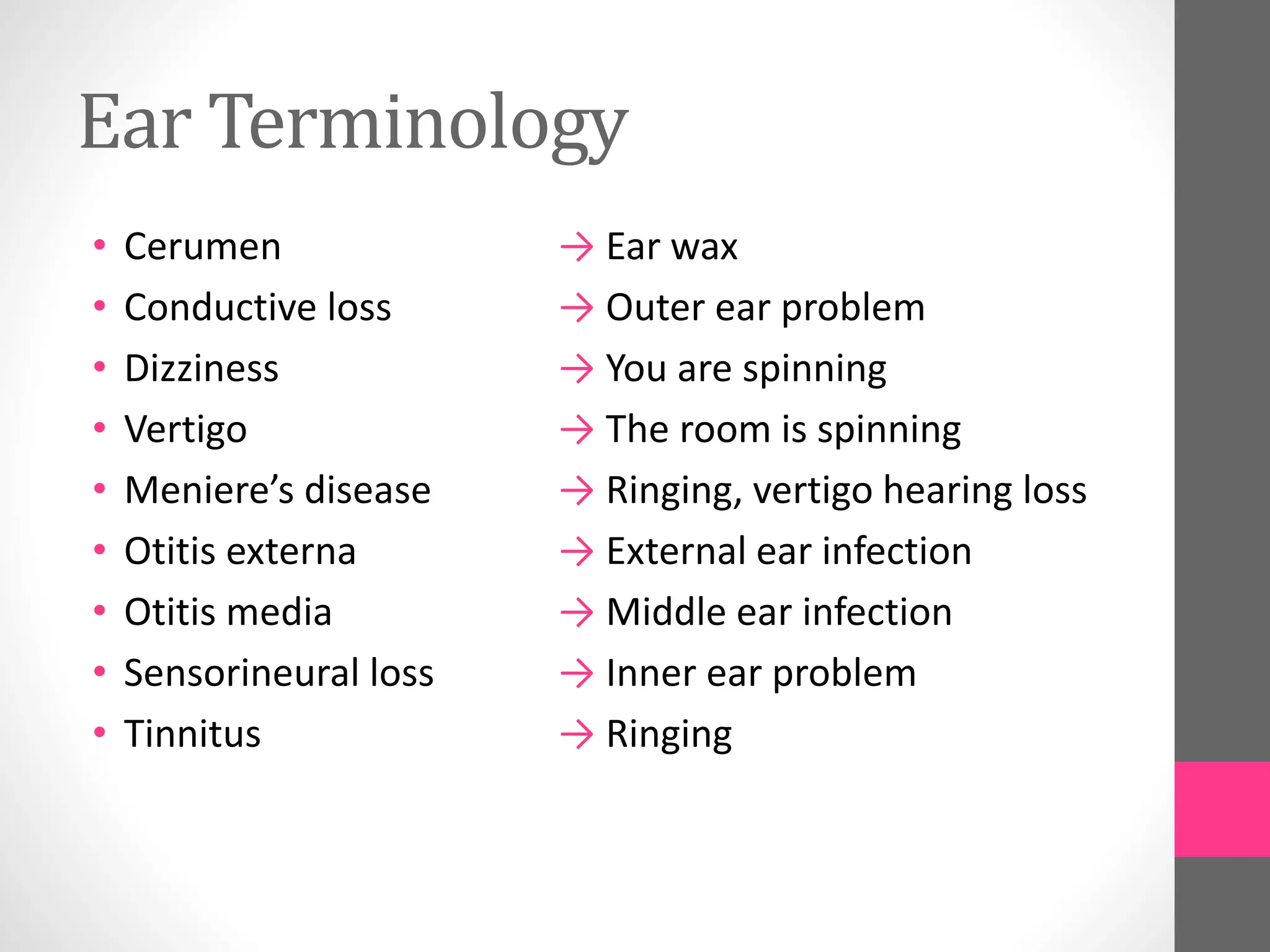
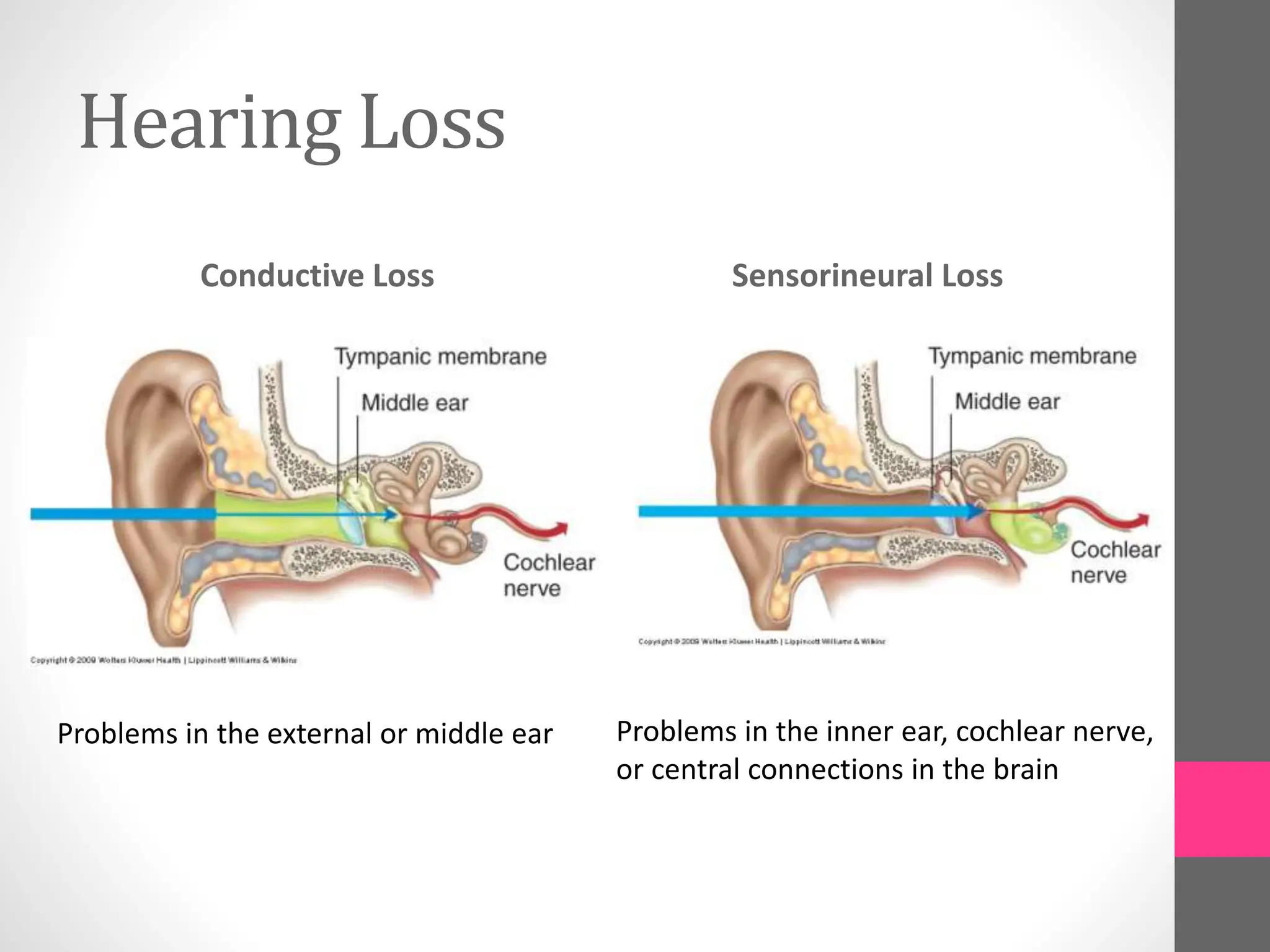
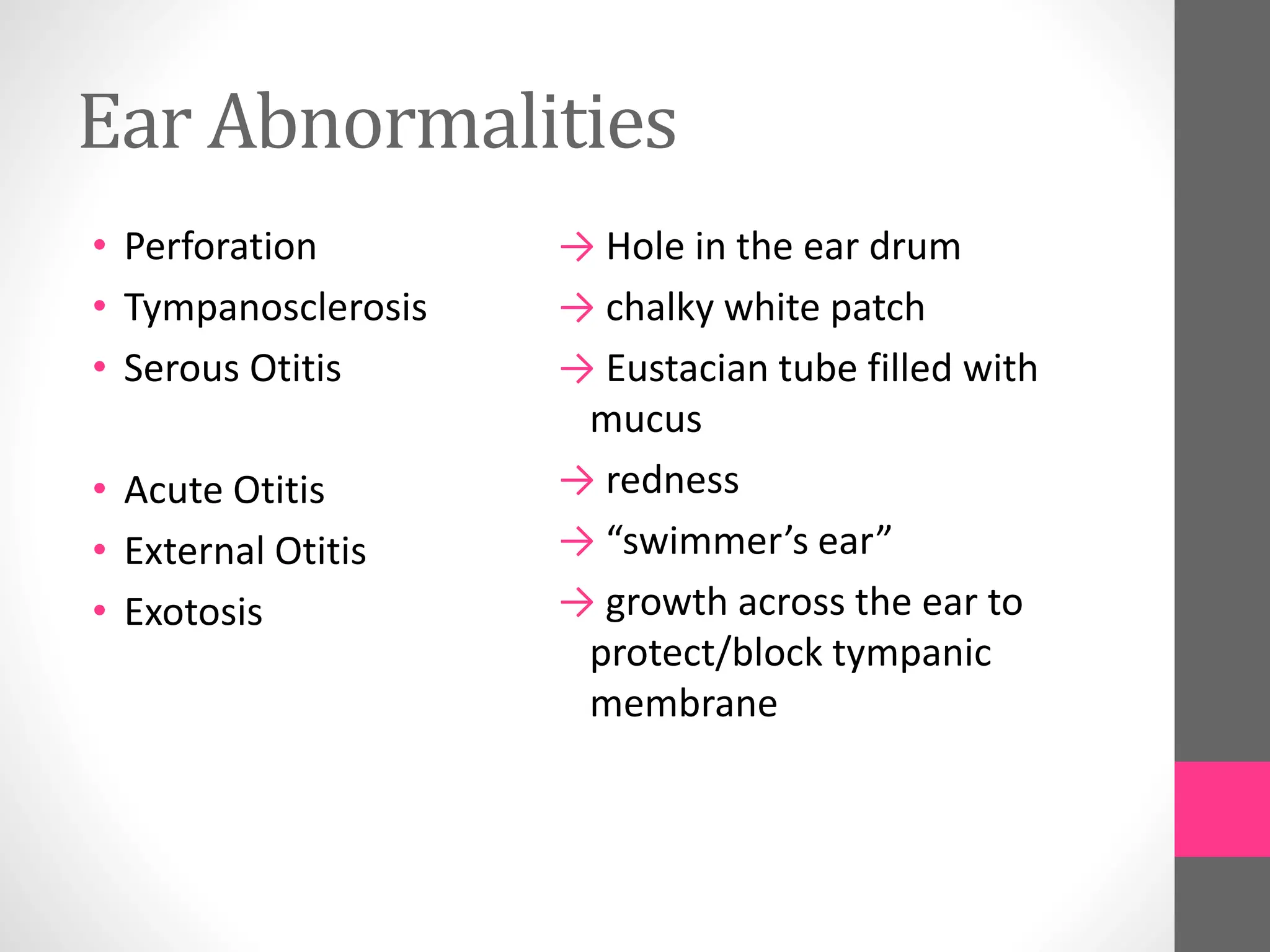
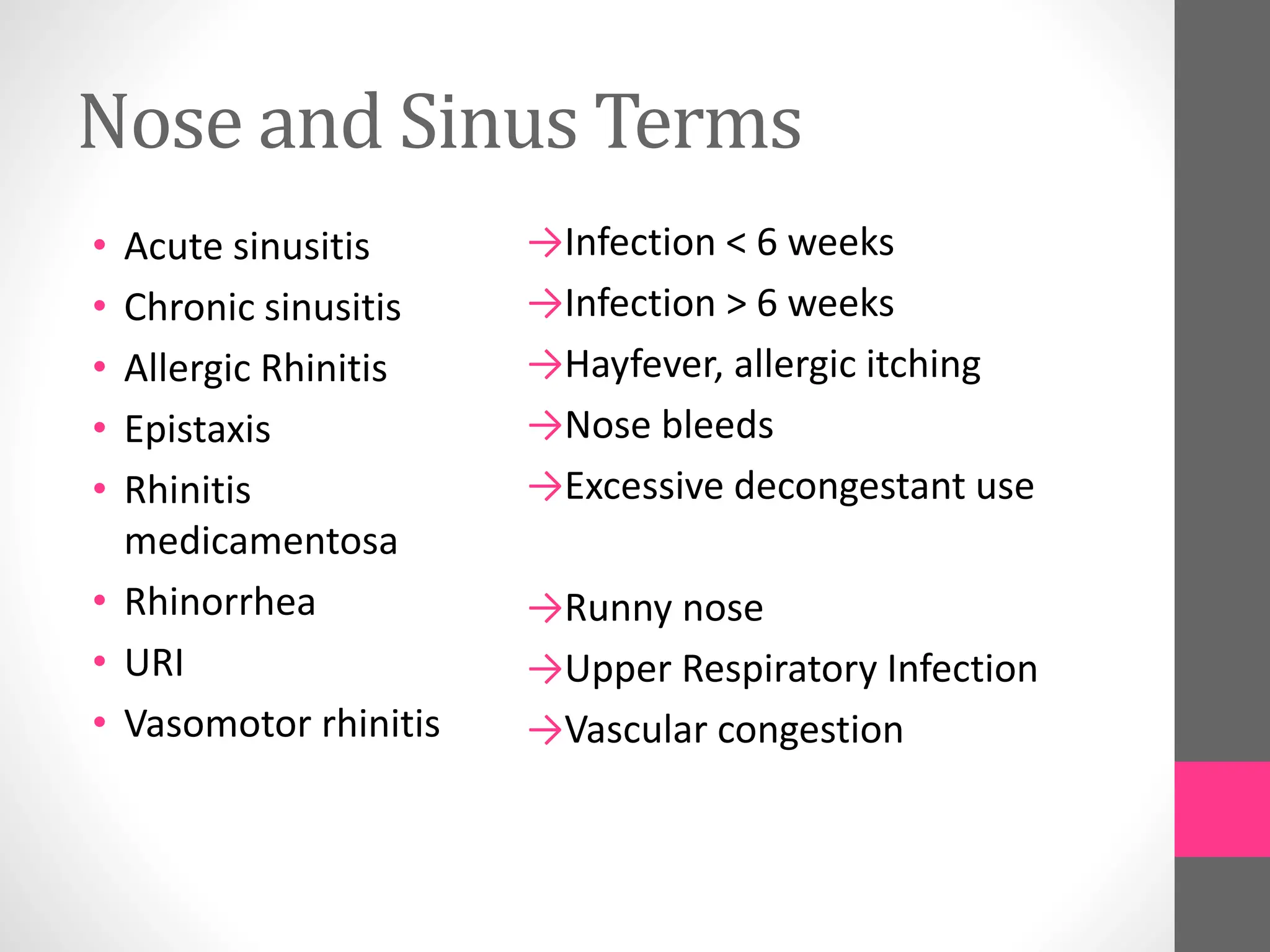
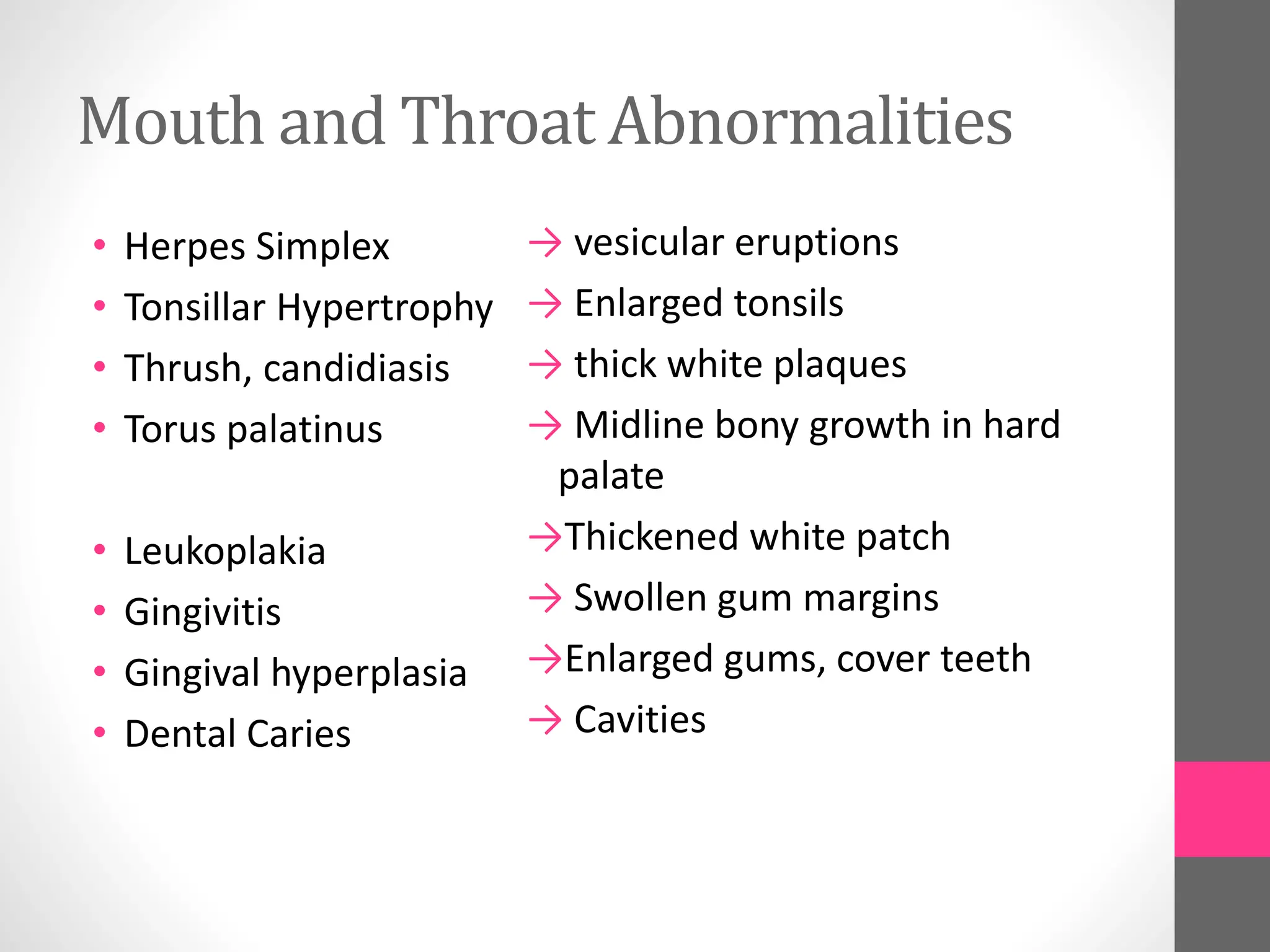
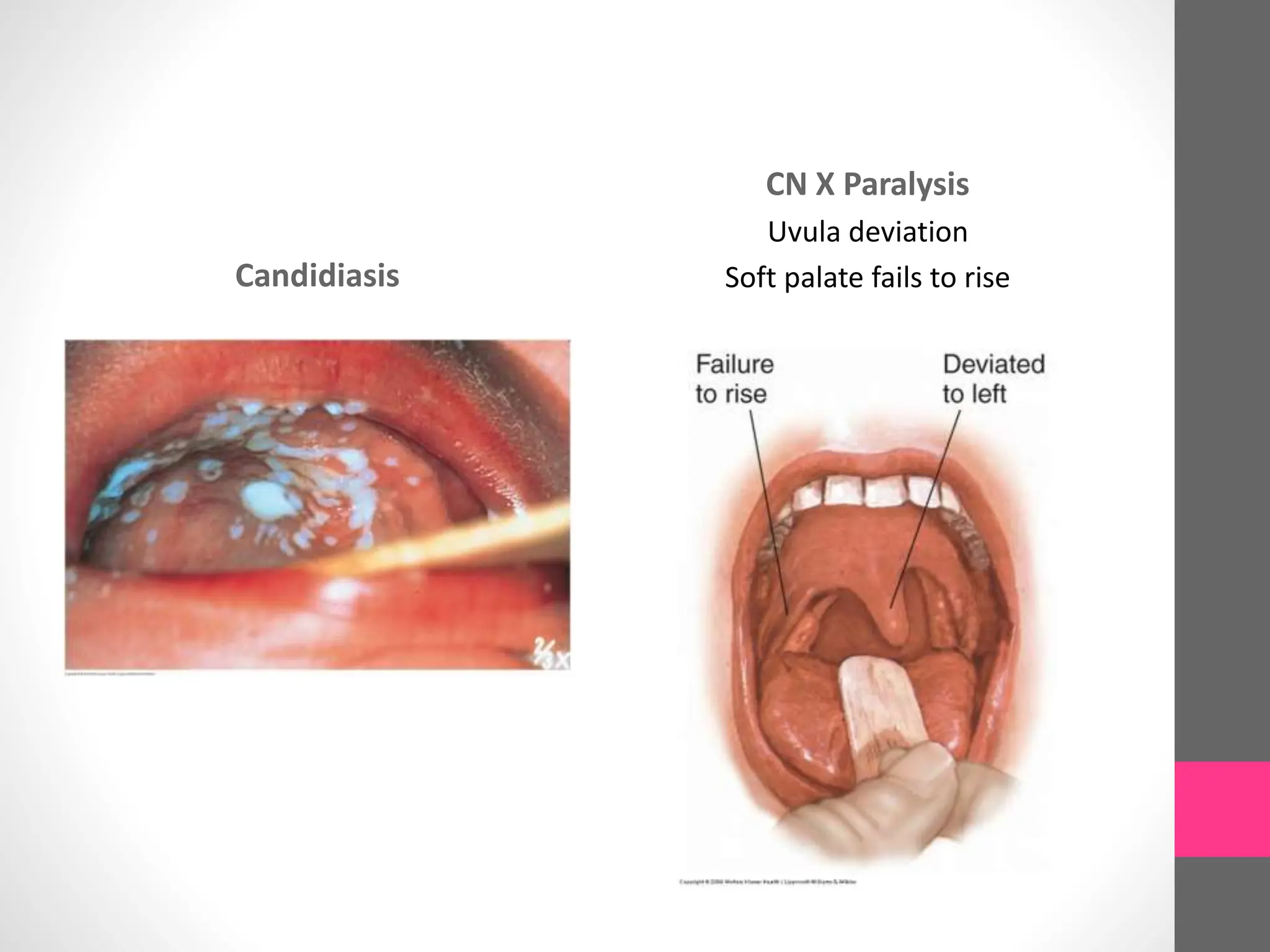
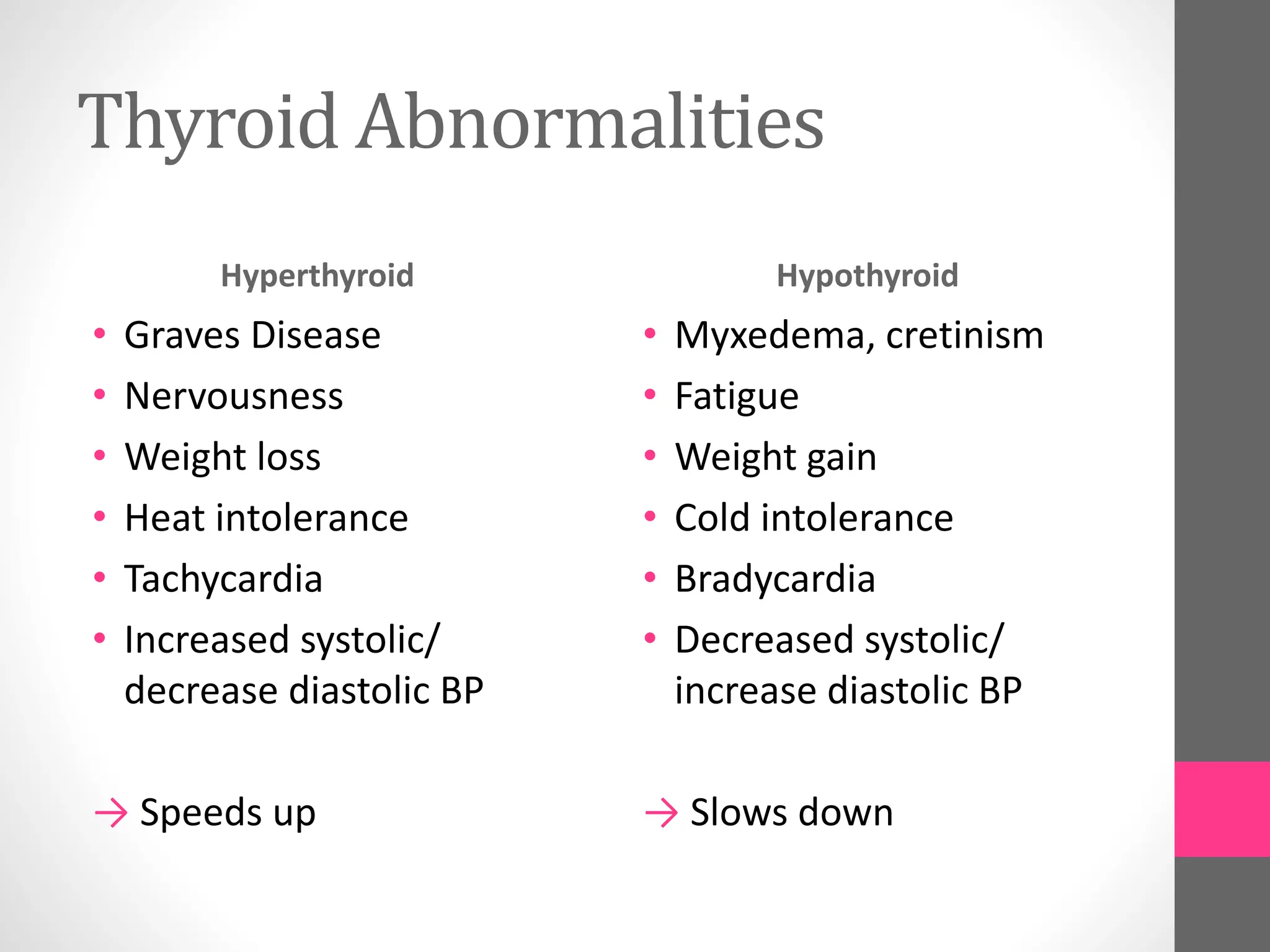
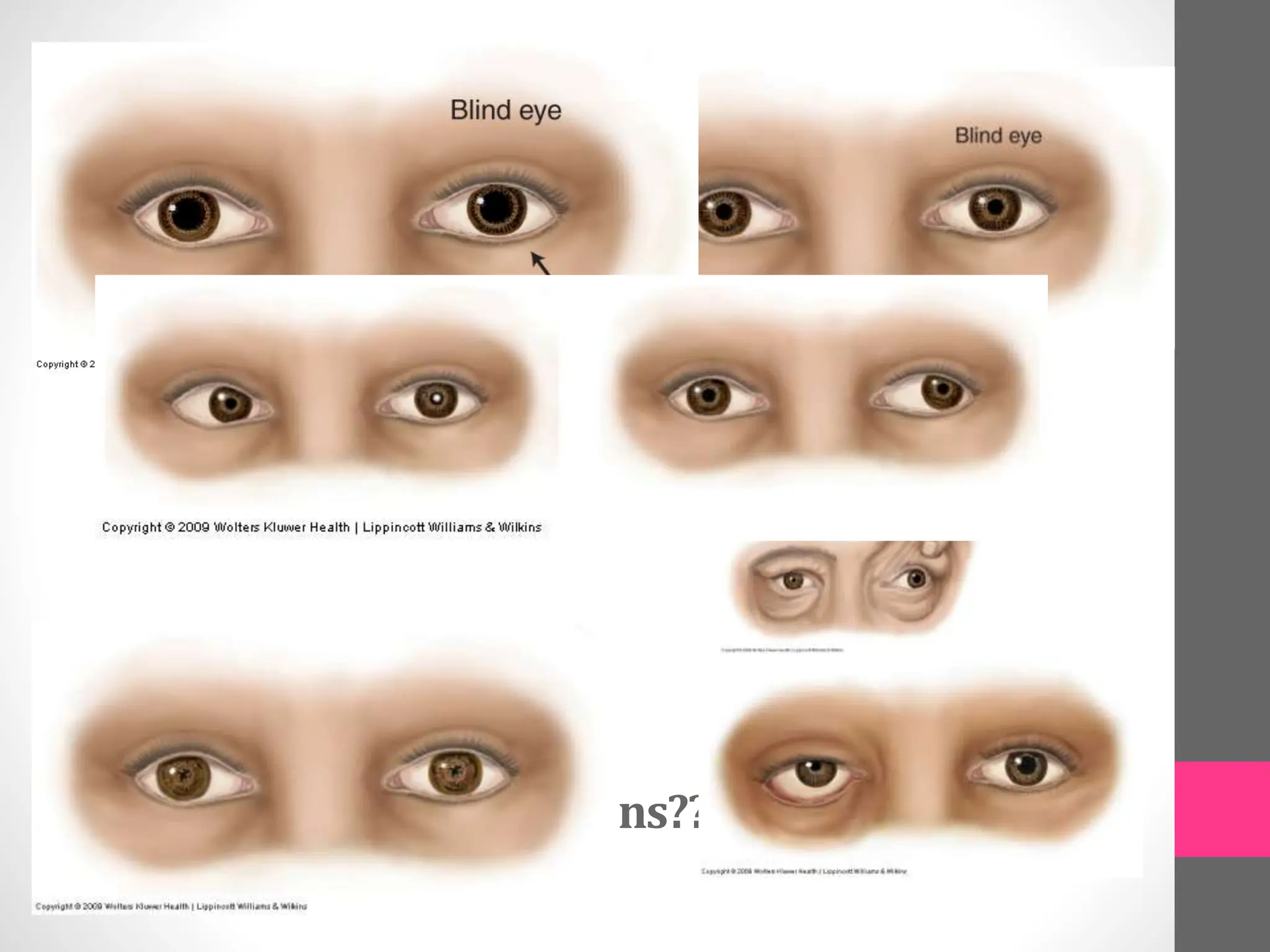
2. Common abnormalities are defined, such as nystagmus, ptosis, visual field defects, perforated eardrum, sinusitis and rhinitis.
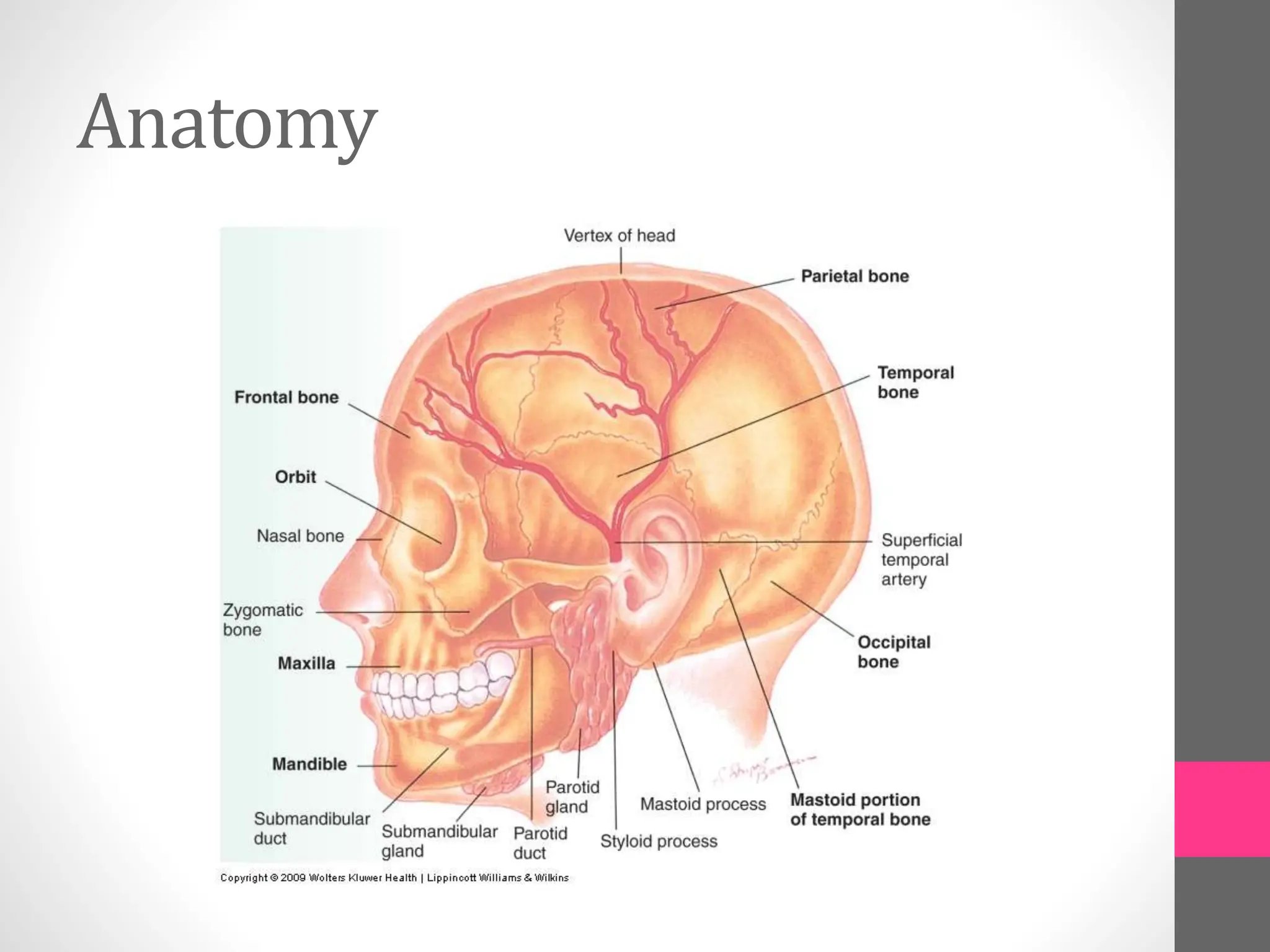
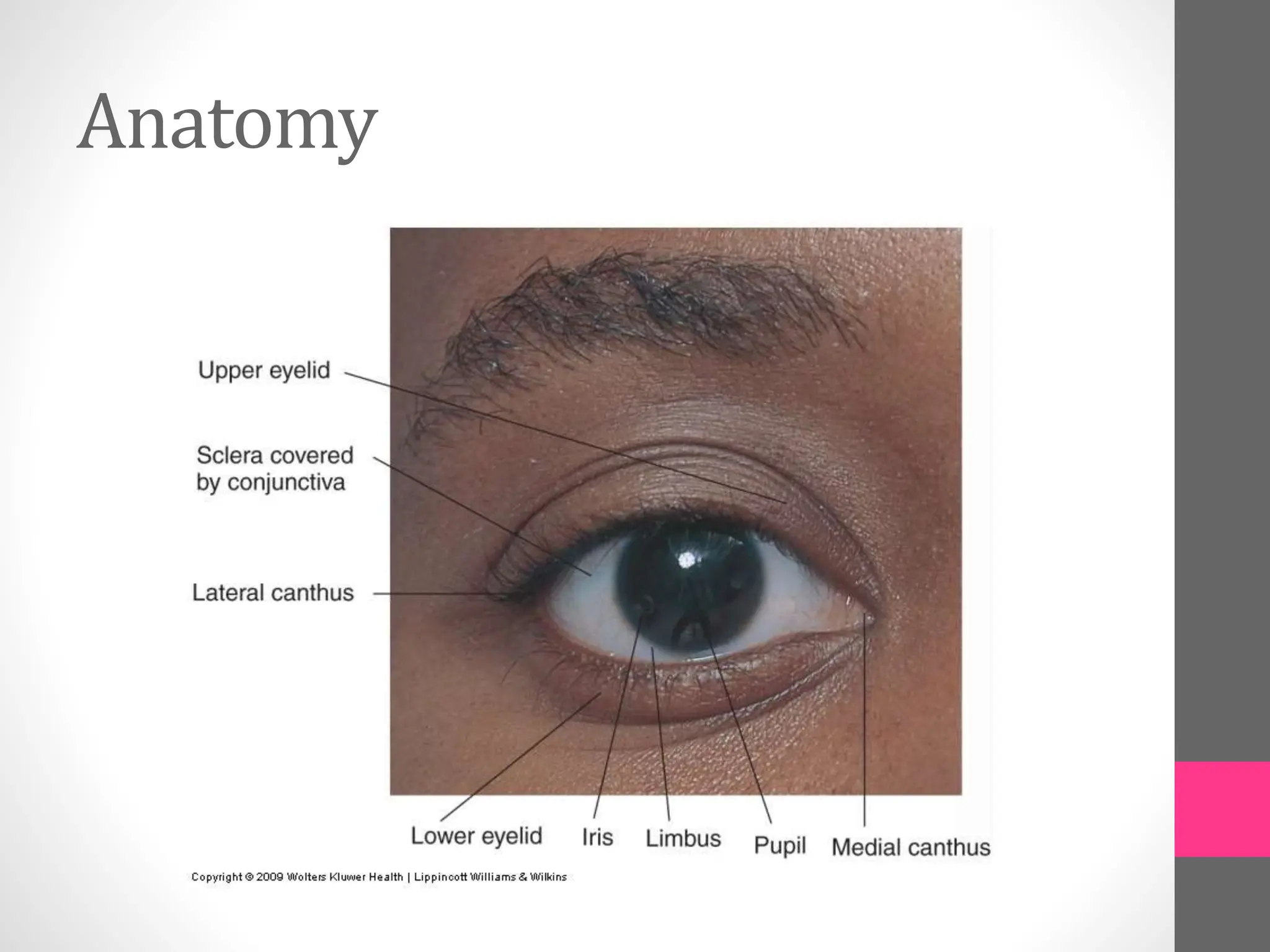
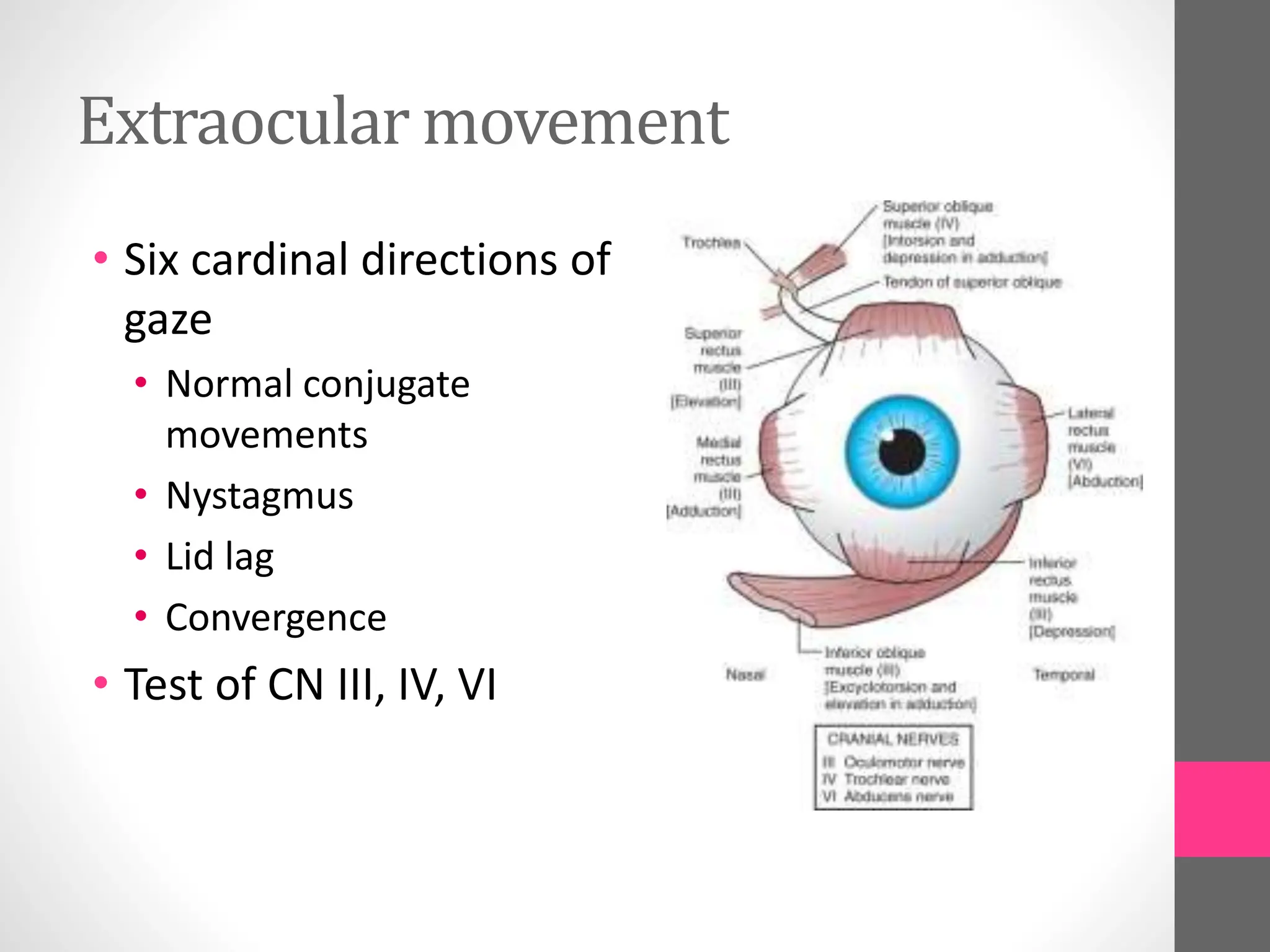
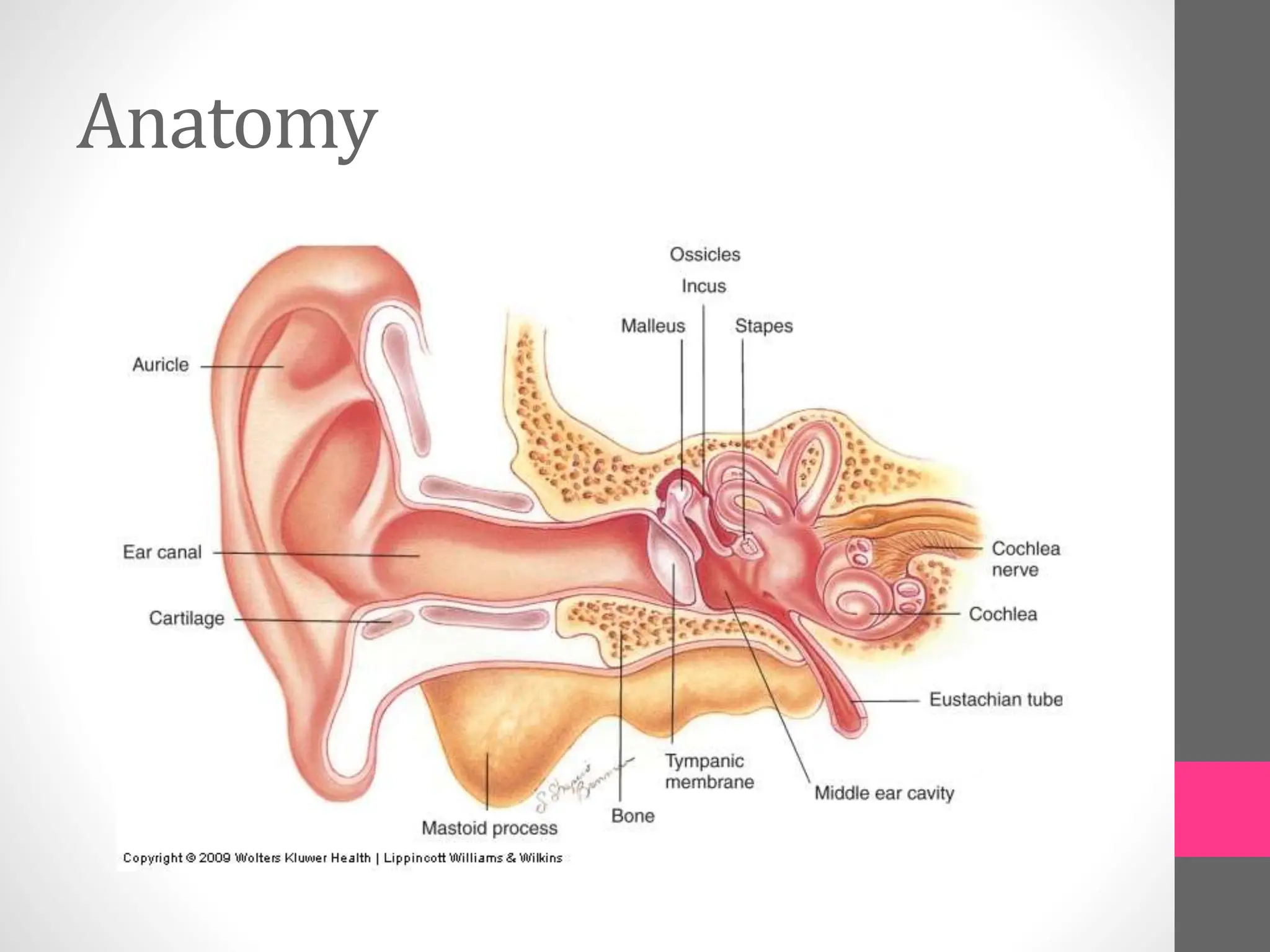
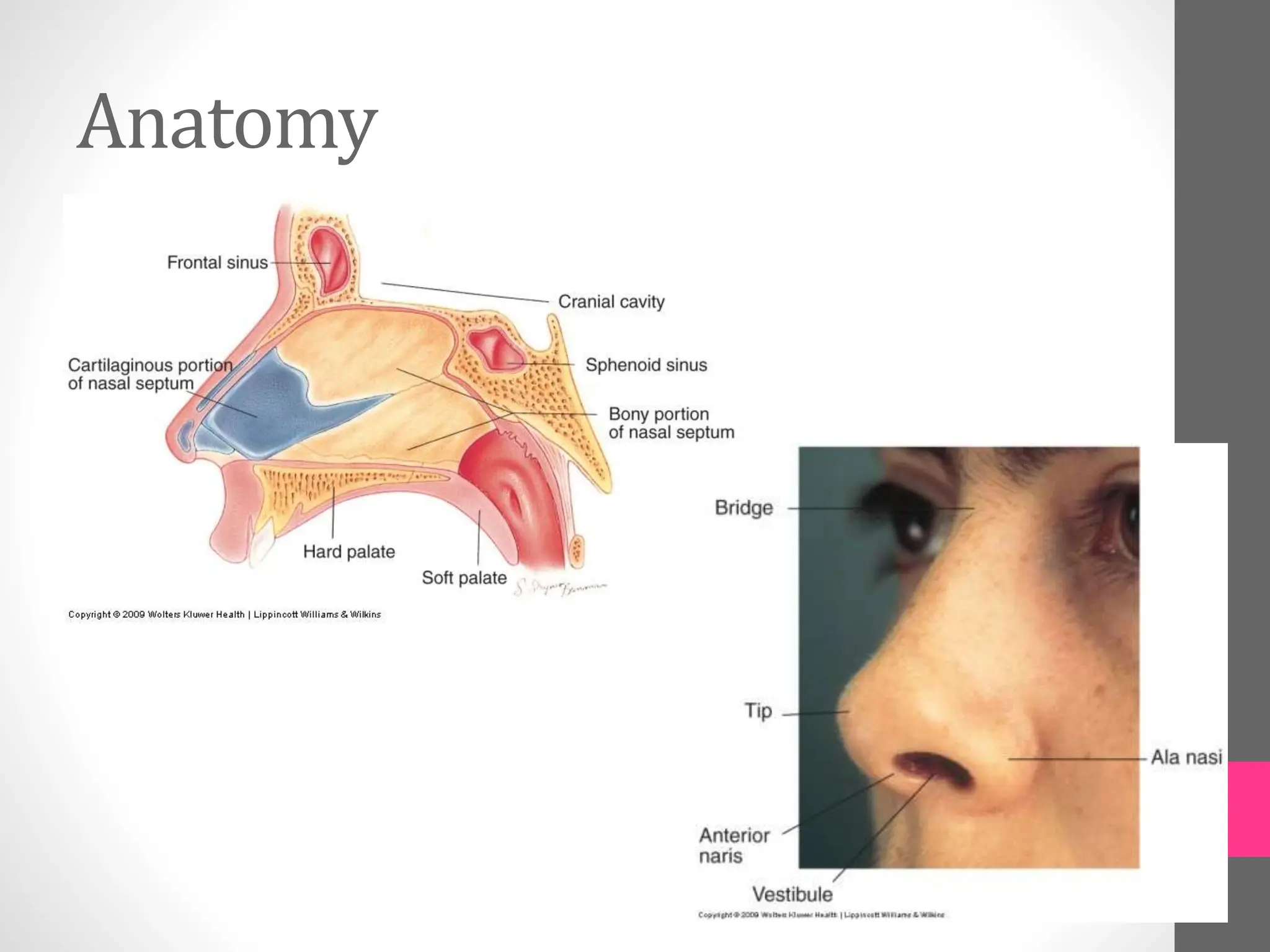
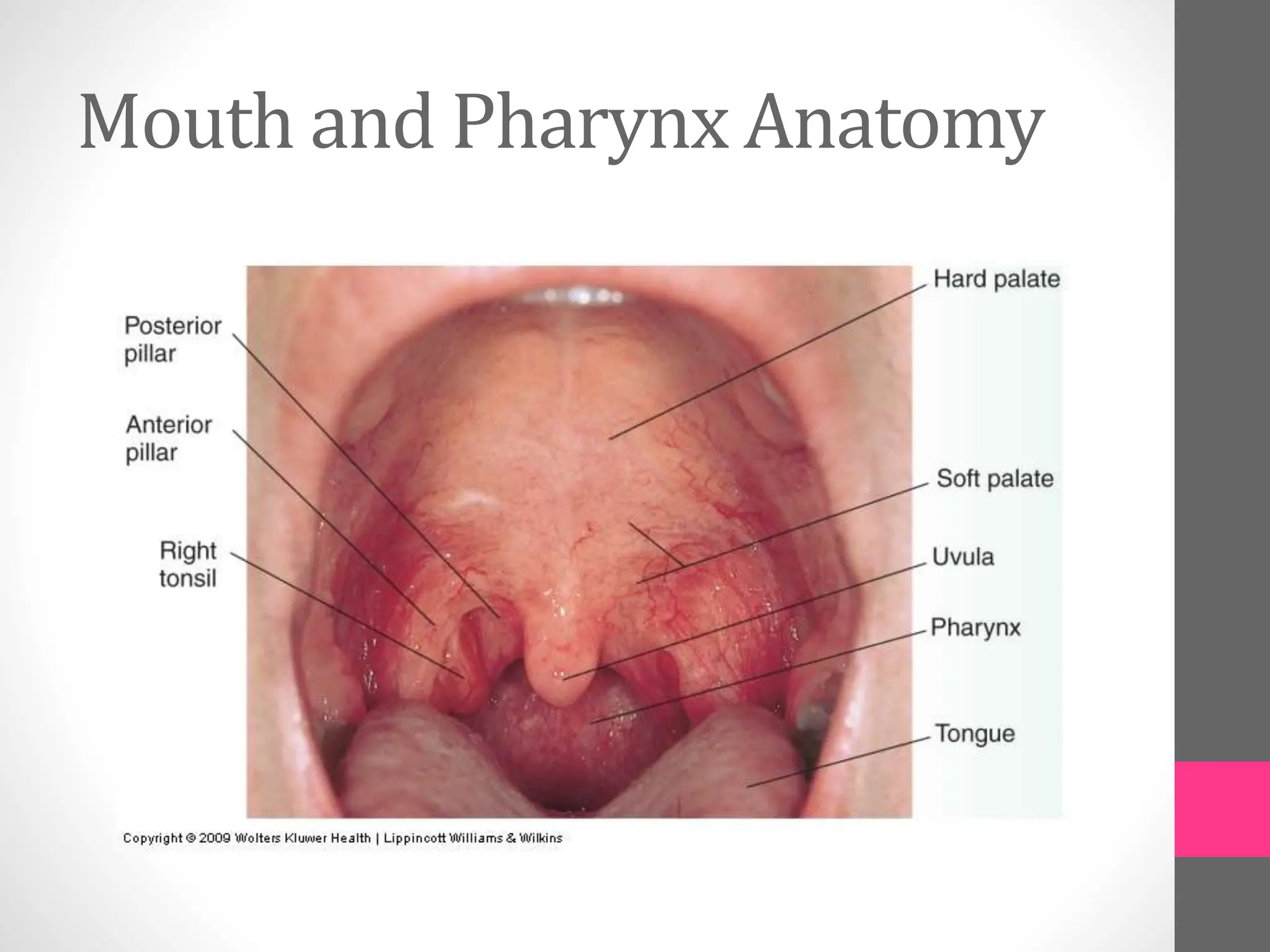
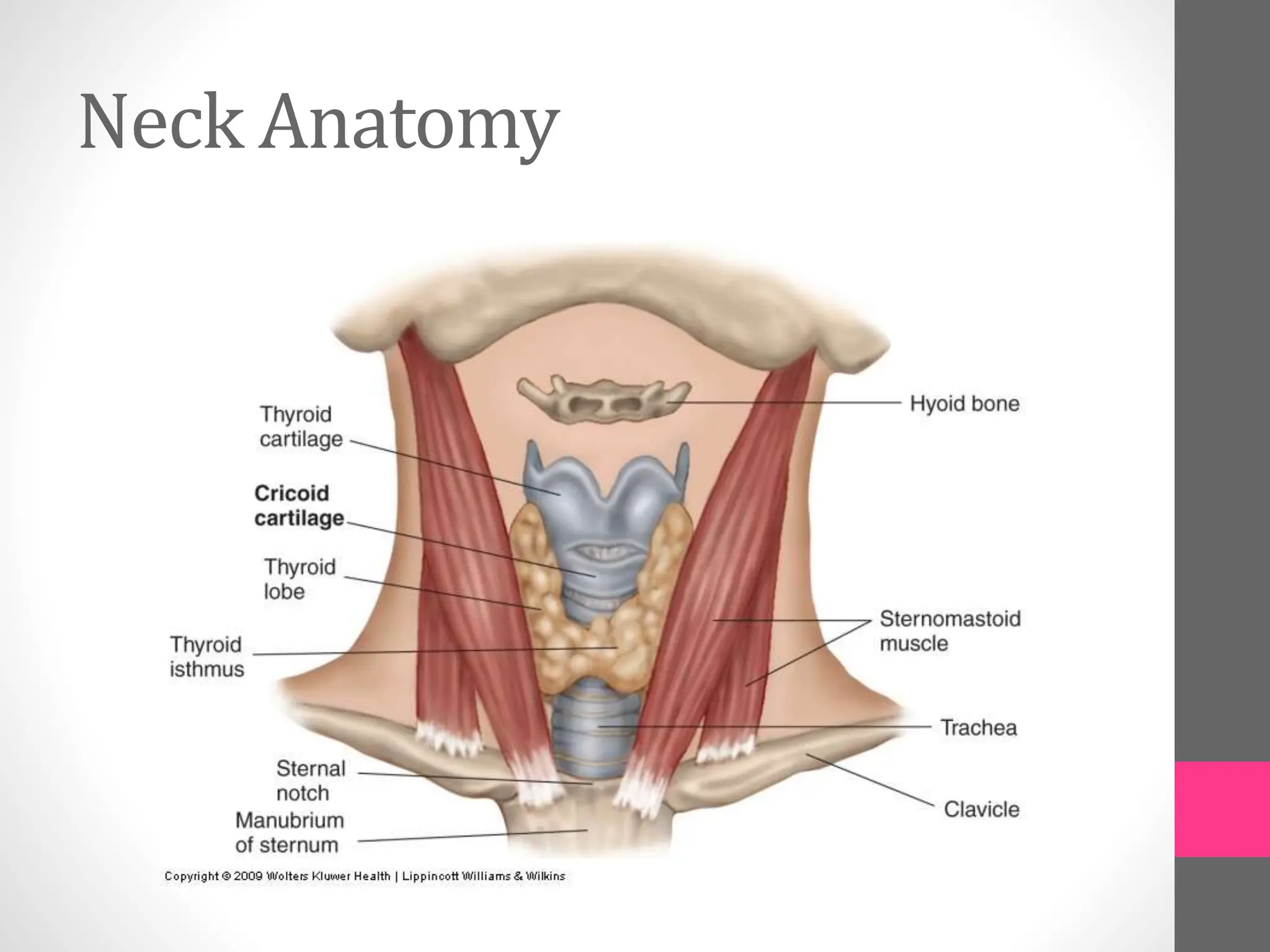
3. The anatomy of each area is briefly outlined to provide context for the examination. Descriptions of pupils, extraocular movements and other exam findings are included.