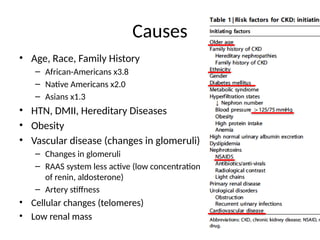
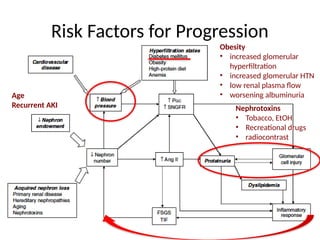
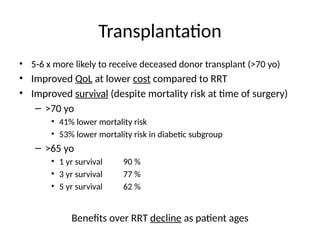
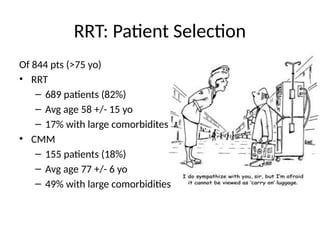
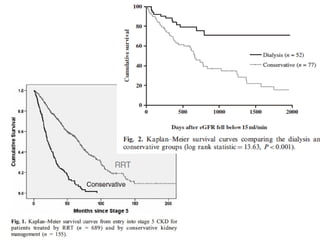
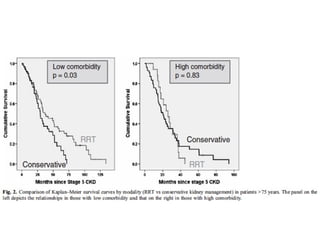
The document discusses chronic kidney disease (CKD) and end-stage renal disease (ESRD) in the geriatric population, highlighting definitions, measurements, risk factors, and management goals. It notes a rising prevalence of CKD with age, particularly among diverse racial groups and those with comorbidities such as diabetes and hypertension. The document emphasizes the importance of nephrology referral, management of complications, and trends in renal replacement therapy (RRT) outcomes, especially in older adults.