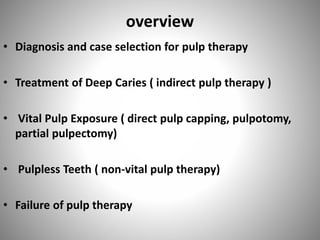
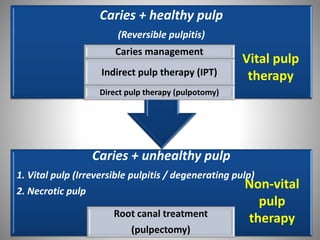
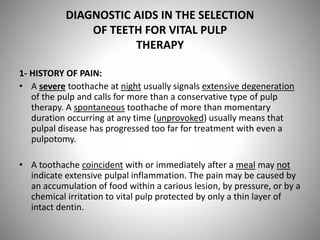
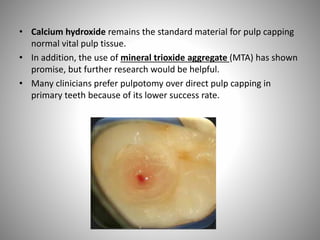
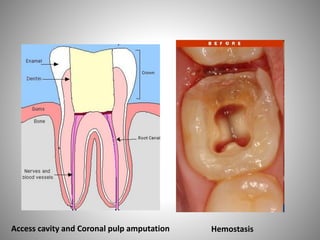
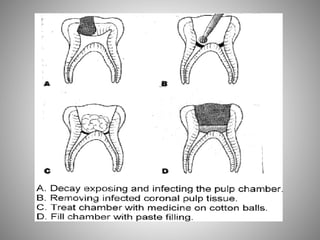
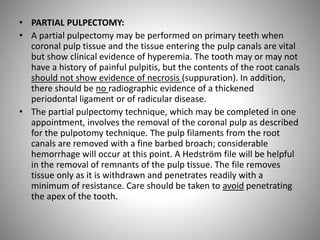
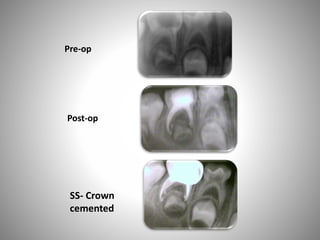
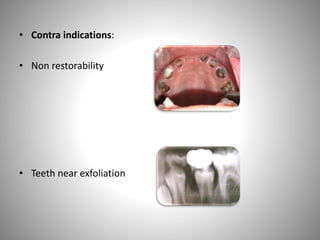
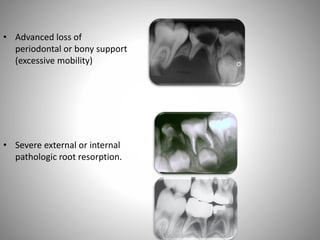
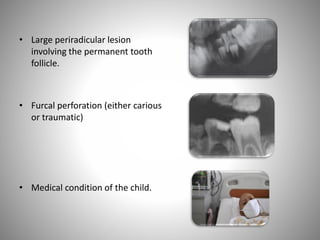
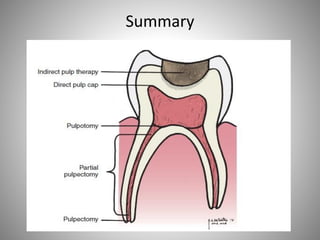
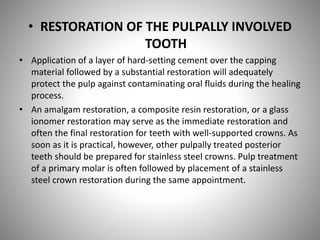
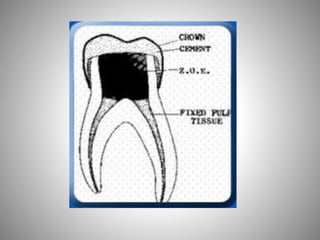
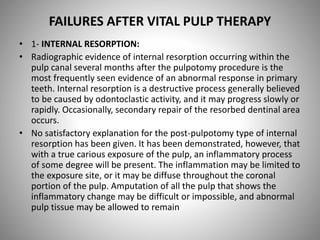
The document provides a comprehensive overview of endodontics for primary teeth, detailing diagnostic approaches, treatment options, and management of pulp therapy including vital and non-vital interventions. It emphasizes the importance of patient history, clinical signs, and radiographic evaluation in case selection, as well as the various techniques like pulpotomy and direct pulp capping based on the condition of the pulp. Additionally, it highlights post-treatment complications and the importance of follow-up in managing pulpally treated teeth.