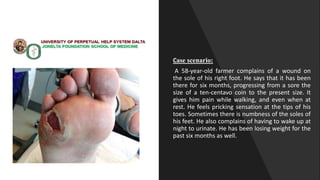
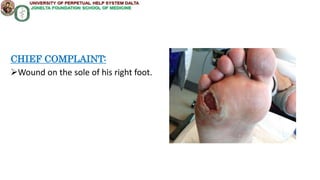
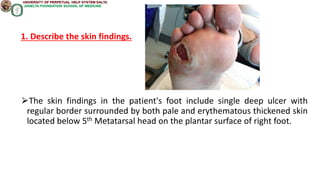
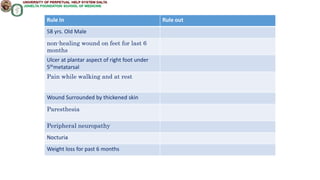
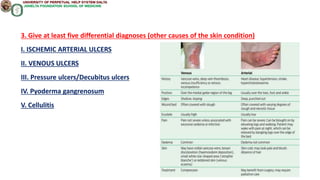
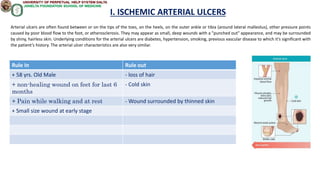
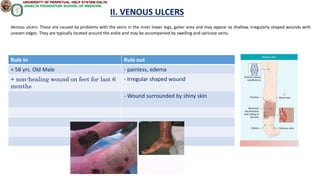
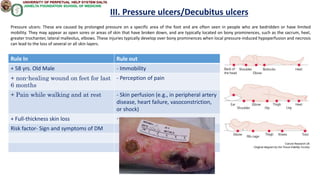
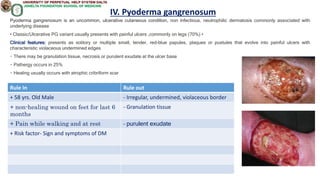
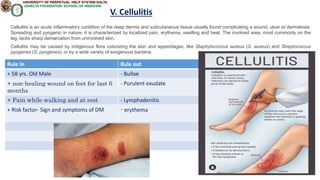
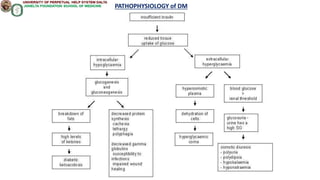
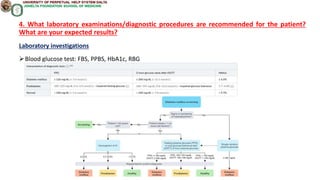
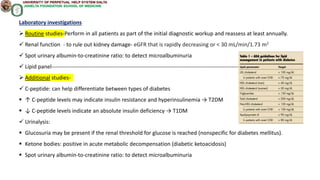
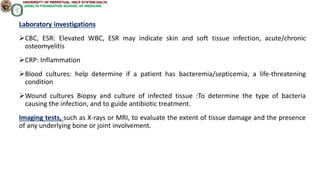
A 58-year-old male farmer presents with a non-healing wound on the sole of his right foot that has been present for six months. He complains of pain in the wound area when walking or at rest, as well as numbness and tingling in his toes and feet. He also reports nocturia and unintentional weight loss over the past six months. Laboratory tests, imaging, and biopsy are recommended to evaluate blood sugar levels, infection, and tissue damage. Treatment options include optimizing diabetes management through lifestyle changes and medications to improve blood glucose control and healing of the foot ulcer.