The document discusses emerging blood glucose monitoring technologies. It notes that the growing diabetes epidemic poses diagnostic and management challenges. There is an immediate need for new approaches to support patient self-management and treatment adherence. The document summarizes various emerging monitoring technologies like continuous glucose monitors, closed loop insulin delivery systems, mobile apps, and alternatives to glucose monitoring. It emphasizes that technology must be tailored to individual patient needs and that self-monitoring of blood glucose remains an important management tool when used properly.

![Bailey TS et al.. Diabetes Technol Ther. 2018
Reddy N, Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279046/
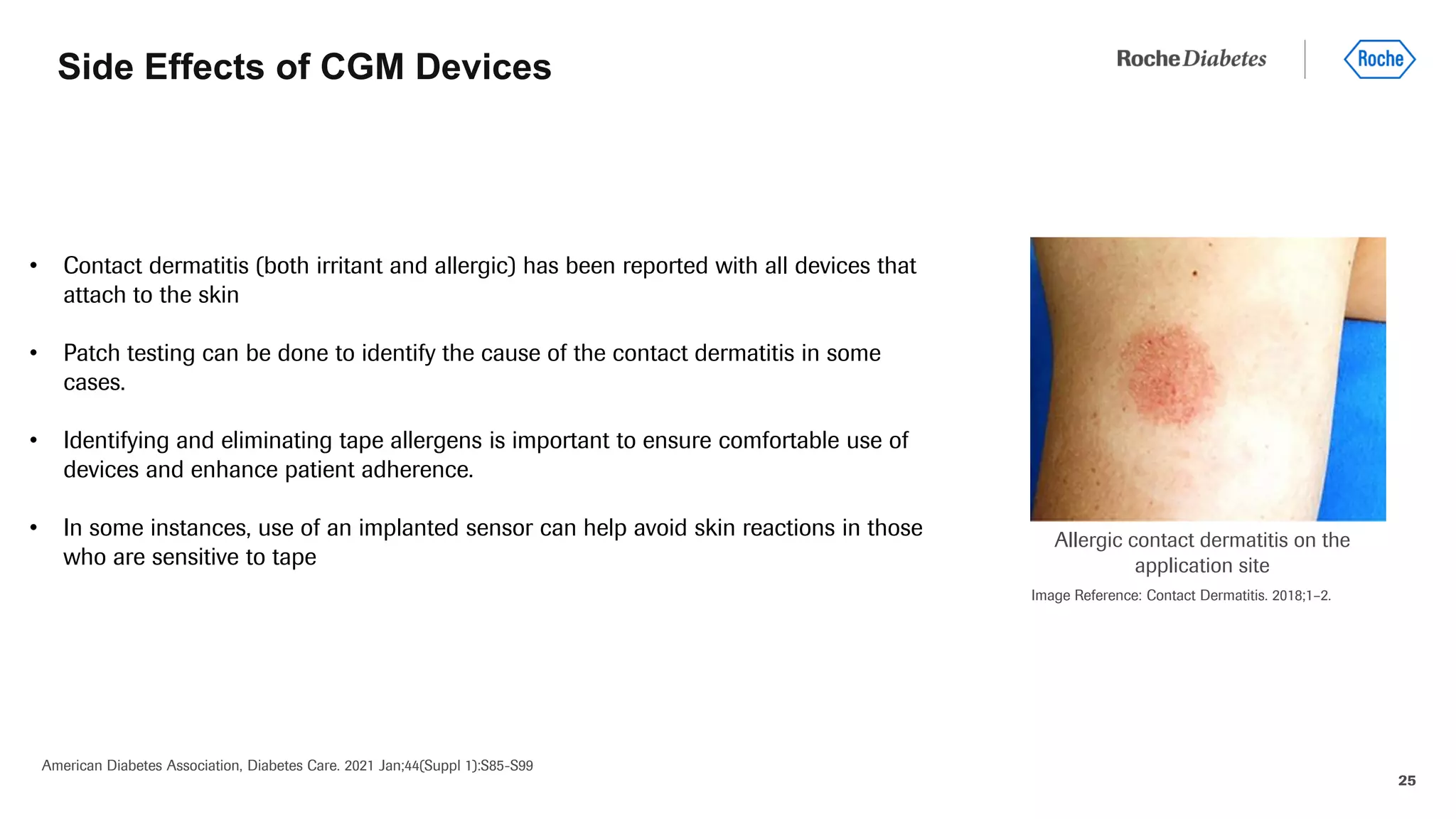
American Diabetes Association, Diabetes Care. 2021 Jan;44(Suppl 1):S85-S99. 4
Overview of diabetes technologies
New and
smarter insulins
and delivery
systems are in
development that
seek to mitigate
both
hyperglycemia and
hypoglycemia and
increase time in
range.
Blood glucose
monitoring as
assessed by meter
or continuous
glucose monitor
Hybrid devices that
both monitor glucose
and deliver insulin
Software that
serves as a
medical device,
providing
diabetes self-
management
support
Information systems
now exist that may be
leveraged to merge
data from previously
discrete systems into
new models of
connected care
1 2 3 4 5](https://image.slidesharecdn.com/sigma-topic5-221006193643-f9ed18d3/75/Emerging-blood-glucose-monitoring-techniques-4-2048.jpg)
![6
The landscape of glucose monitoring technologies is
expanding and rapidly changing
Continuous glucose
monitoring (CGM)
Permit significantly more fine-
tuned adjustments in insulin
dosing and other therapies.
CGM technologies for automatic
collection of data have spurred
interest in noninvasive glucose
monitoring as an additional tool
for obtaining information about
glucose levels.
Closed loop control
(CLC)
Also known as an
“artificial” or “bionic”
pancreas, this technology
links CGM with
automatically controlled
insulin delivery.
Mobile Technology
and Decision Support
Increasing connectivity
between glucose
monitoring technologies
and mobile devices has
facilitated ongoing
improvements in self-
care and
communication of data.
Alternate
Markers of
Glucose Control
Use of additional
analytes besides
glucose is being
established.
Reddy N, Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279046/](https://image.slidesharecdn.com/sigma-topic5-221006193643-f9ed18d3/75/Emerging-blood-glucose-monitoring-techniques-6-2048.jpg)
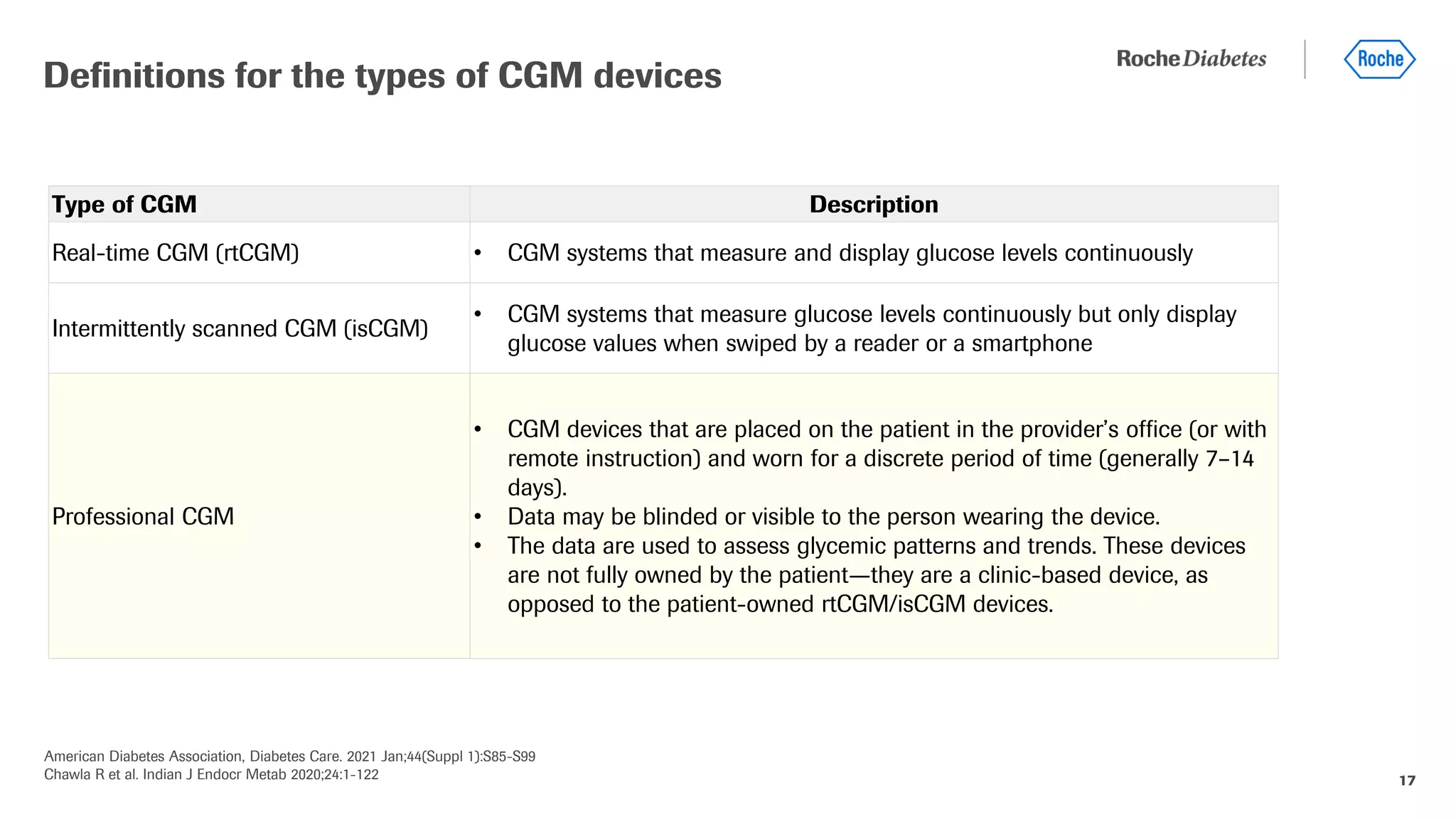
![American Diabetes Association, Diabetes Care. 2021 Jan;44(Suppl 1):S85-S99
Chawla R et al. Indian J Endocr Metab 2020;24:1-122 14
Most commonly followed accuracy standards for
glucometers
•BG, blood glucose; FDA, U.S. Food and Drug Administration; ISO, International Organization for Standardization.
•↵† The range of blood glucose values for which the meter has been proven accurate and will provide readings (other than low, high, or error).
•↵‡ Values outside of the “clinically acceptable” A and B regions are considered “outlier” readings and may be dangerous to use for therapeutic
decisions
• International Organization for Standardization (ISO
15197:2013)[740]
• U. S. Food and Drug Administration (USFDA)
Comparison of ISO 15197:2013 and FDA blood glucose meter accuracy standards](https://image.slidesharecdn.com/sigma-topic5-221006193643-f9ed18d3/75/Emerging-blood-glucose-monitoring-techniques-14-2048.jpg)
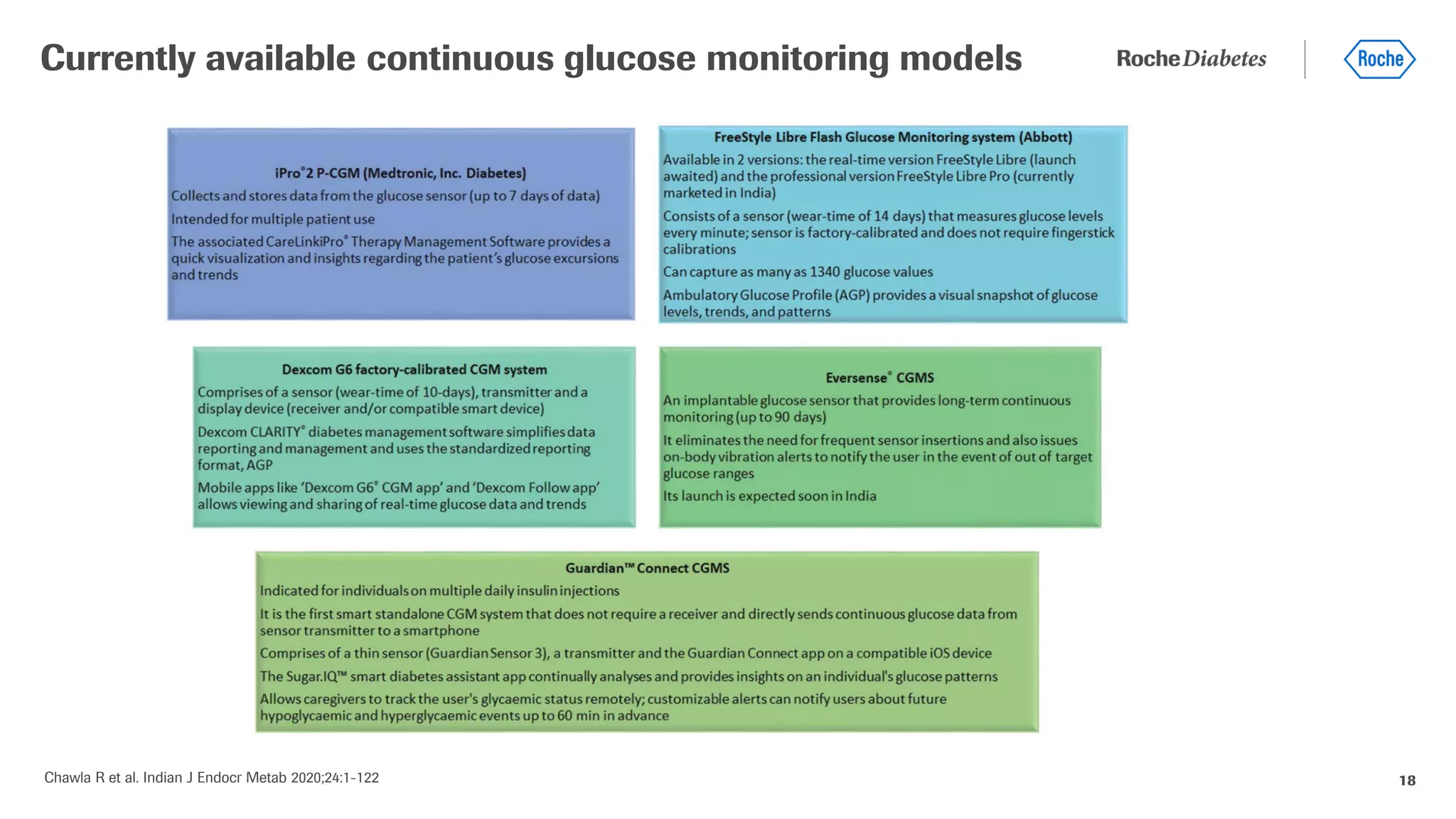
![16
• CGM measures glucose levels (typically interstitial glucose) continuously and
updates the glucose level display every 1 to 5 minutes.
• Most CGMs consist of
1) a monitor to display the information (in some cases, this is the patient’s
mobile device)
2) a sensor that is usually inserted into the subcutaneous tissue, and
3) a transmitter that transmits the sensor data to the monitor.
• Most CGM devices were approved for adjunctive use only due to limitations in
accuracy; in this case patients must still perform fingerstick glucose monitoring in
order to guide therapy and perform calibrations.
Continuous glucose monitoring (CGM): a complementary
method for assessment of glycemic control
Reddy N, Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-.
Available from: https://www.ncbi.nlm.nih.gov/books/NBK279046/
Kesavadev J et al. J Diabetol 2017;8:61-7
Chawla R et al. Indian J Endocr Metab 2020;24:1-122
Continuous Glucose Monitoring System (iPro2)
Image from: Kesavadev J et al. J Diabetol 2017;8:61-7](https://image.slidesharecdn.com/sigma-topic5-221006193643-f9ed18d3/75/Emerging-blood-glucose-monitoring-techniques-16-2048.jpg)
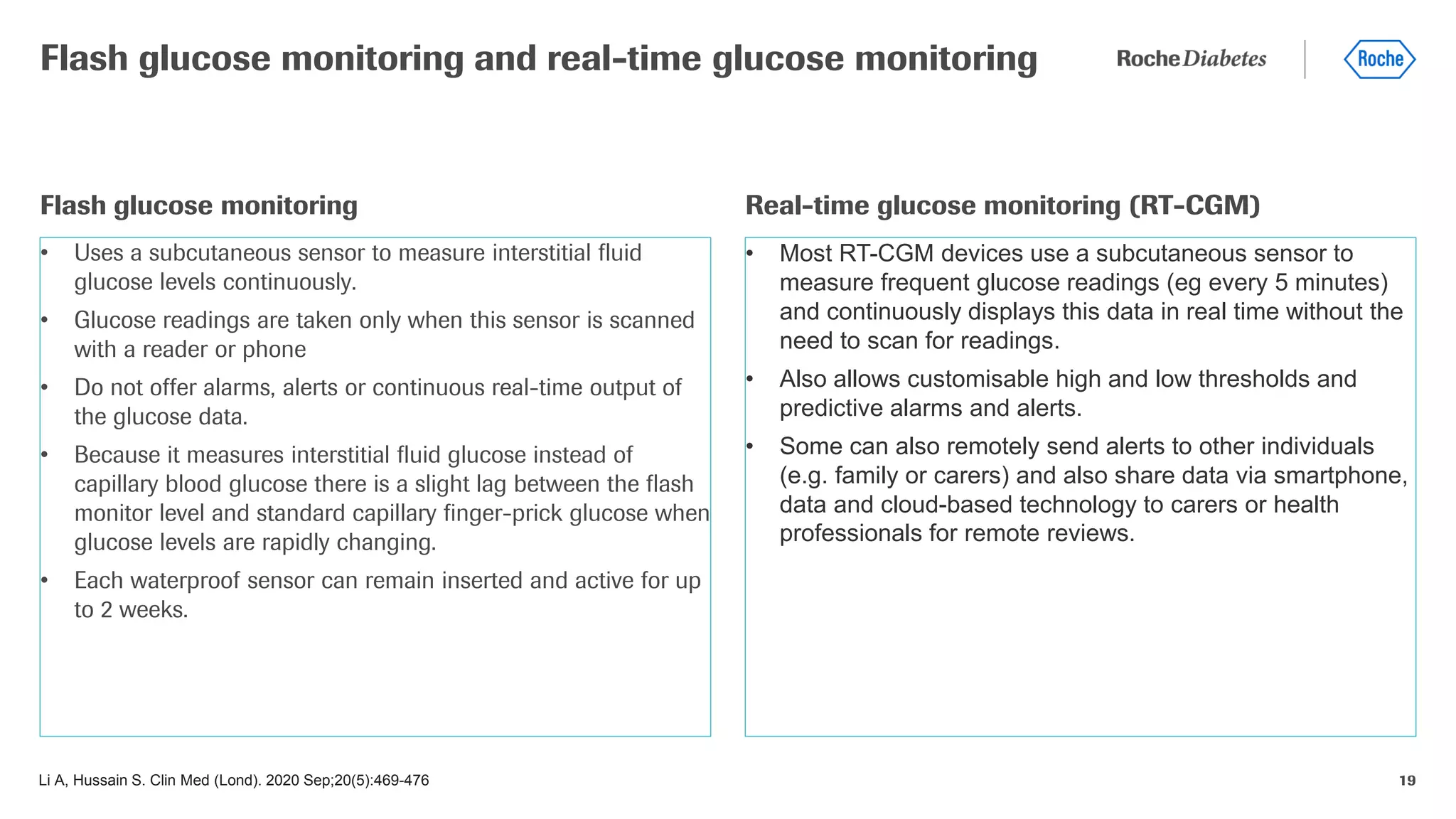
![27
AGP is a standardized reporting format for glucose data that was developed by an expert panel of diabetes
specialists and is customized for insulin pumps or injection therapy.
AGP averages daily glucose records, presenting the median glucose and its 25–75th and 10–90th
percentiles across a standard ‘modal’ day.
AGP is currently employed by many reporting systems and consists of 3 components:
1. Statistical Summary, which utilizes standard metrics and terminology to summarize the number of
values, percentage of values and time in target, above target, and below target, as well as an
assessment of glucose variability.
2. Modal day report which collapses data from days or weeks to a single day in order to identify patterns
by time of day. Data are presented graphically as 5 distribution curves, representing the median,
interquartile range, and 10th to 90th percentiles, on the backdrop of target range.
3. Daily View, which facilitates review of within day events.
Ambulatory Glucose Profile (AGP)
Reddy N, Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-.
Available from: https://www.ncbi.nlm.nih.gov/books/NBK279046/](https://image.slidesharecdn.com/sigma-topic5-221006193643-f9ed18d3/75/Emerging-blood-glucose-monitoring-techniques-27-2048.jpg)
![28
• Glucose Statistics: Metrics include mean glucose,
estimated A1C, glucose ranges, coefficient of variation and
standard deviation.
• Glucose Profile: Daily glucose profiles are combined to
make a one-day (24-hour) picture. Ideally, lines would stay
within grey shaded area (target range)
• Orange: median (middle) glucose line
• Blue: area between blue lines shows 50% of the
glucose values
• Green: 10% of values are above (90% top line) and
10% are below (10% bottom line)
• Insulin Profile Graph: Shows basal insulin pump settings
over a 24-hour period
• Bolus Insulin Graph: Combines all bolus insulin doses
into one graph to make a one day (24-hour) picture. Each
box on the graph covers 60 minutes of doses.
• Orange: median (middle) dot
• Blue: shaded box shows 50% of the bolus dosages in
the hour
• Green: lines above and below the shaded box
(whiskers) show how many of the bolus dosages per
hour were between 75 - 90% and between 10 - 25%
Ambulatory Glucose Profile (AGP)
Reddy N, Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-.
Available from: https://www.ncbi.nlm.nih.gov/books/NBK279046/](https://image.slidesharecdn.com/sigma-topic5-221006193643-f9ed18d3/75/Emerging-blood-glucose-monitoring-techniques-28-2048.jpg)