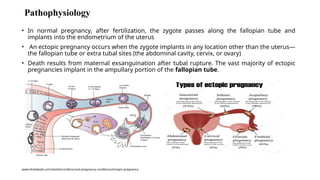
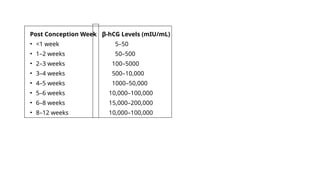
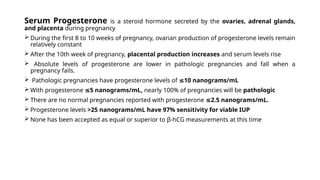
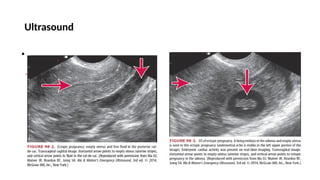
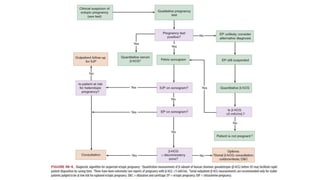
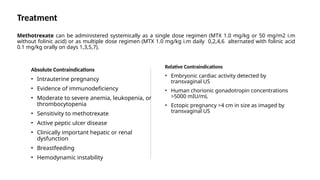
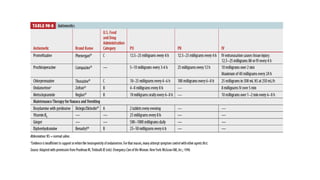
The document provides a comprehensive overview of ectopic pregnancy and other related emergencies within the first 20 weeks of pregnancy, detailing assessment procedures, diagnostic evaluations, management strategies, and risk factors. Key points include the importance of hemodynamic stability, the utilization of serum hCG testing and ultrasound for diagnosis, and treatment options ranging from medical management with methotrexate to surgical interventions. Additionally, it covers conditions such as spontaneous abortion, septic abortion, and gestational trophoblastic disease, emphasizing their diagnosis and treatment approaches.