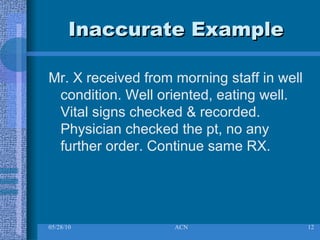
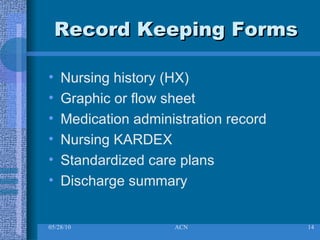
Nursing documentation (ND) involves recording a patient's care and is important for communication, facilitating good care, and meeting legal standards. Accurate ND describes assessments, interventions, and outcomes; and information reported to physicians. Benefits include providing a record of critical thinking, reflecting care quality, and demonstrating nursing's unique contributions. Principles include being comprehensive, reflecting standards, and having identifying information. Inaccurate examples lack details, while accurate examples fully describe a patient's condition and care.