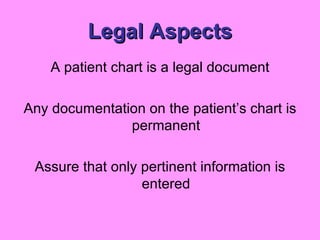
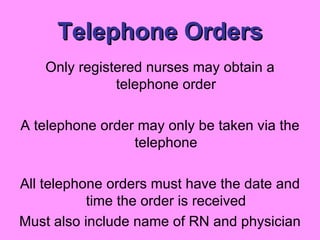
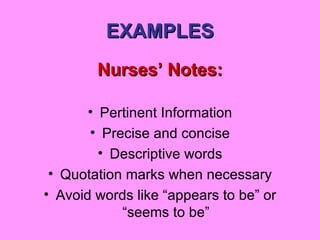
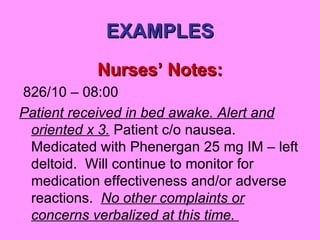
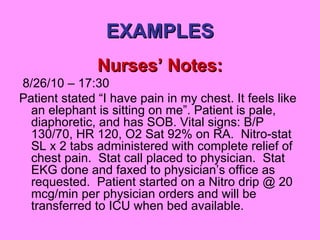
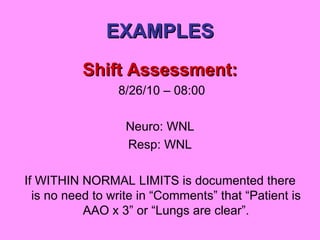
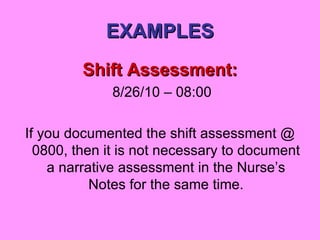
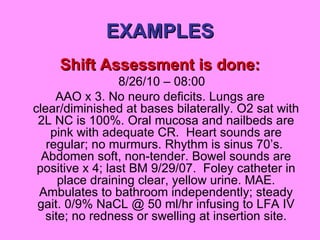
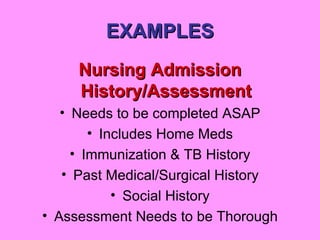
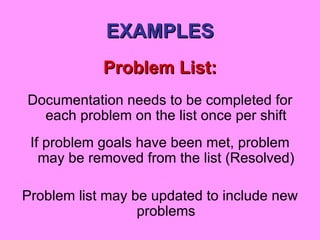
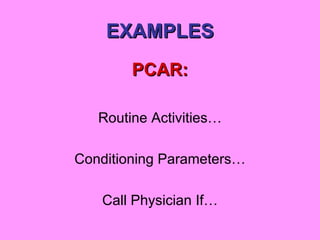
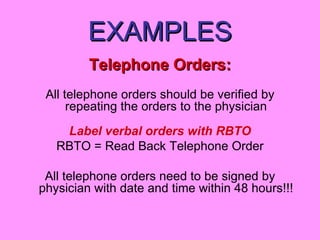
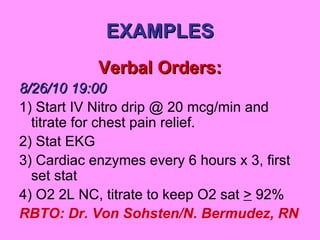
This document provides guidance on nursing documentation for novice and experienced nurses. It discusses the importance of documentation for continuity of care, quality management, and legal protection. It reviews different documentation systems and tools used at Bethesda Memorial Hospital, including shift assessments, nurses' notes, problem lists, and incident reports. Examples of proper documentation formats are also provided. The reference stresses that nursing documentation must be thorough yet concise to tell the patient's story factually without judgments.