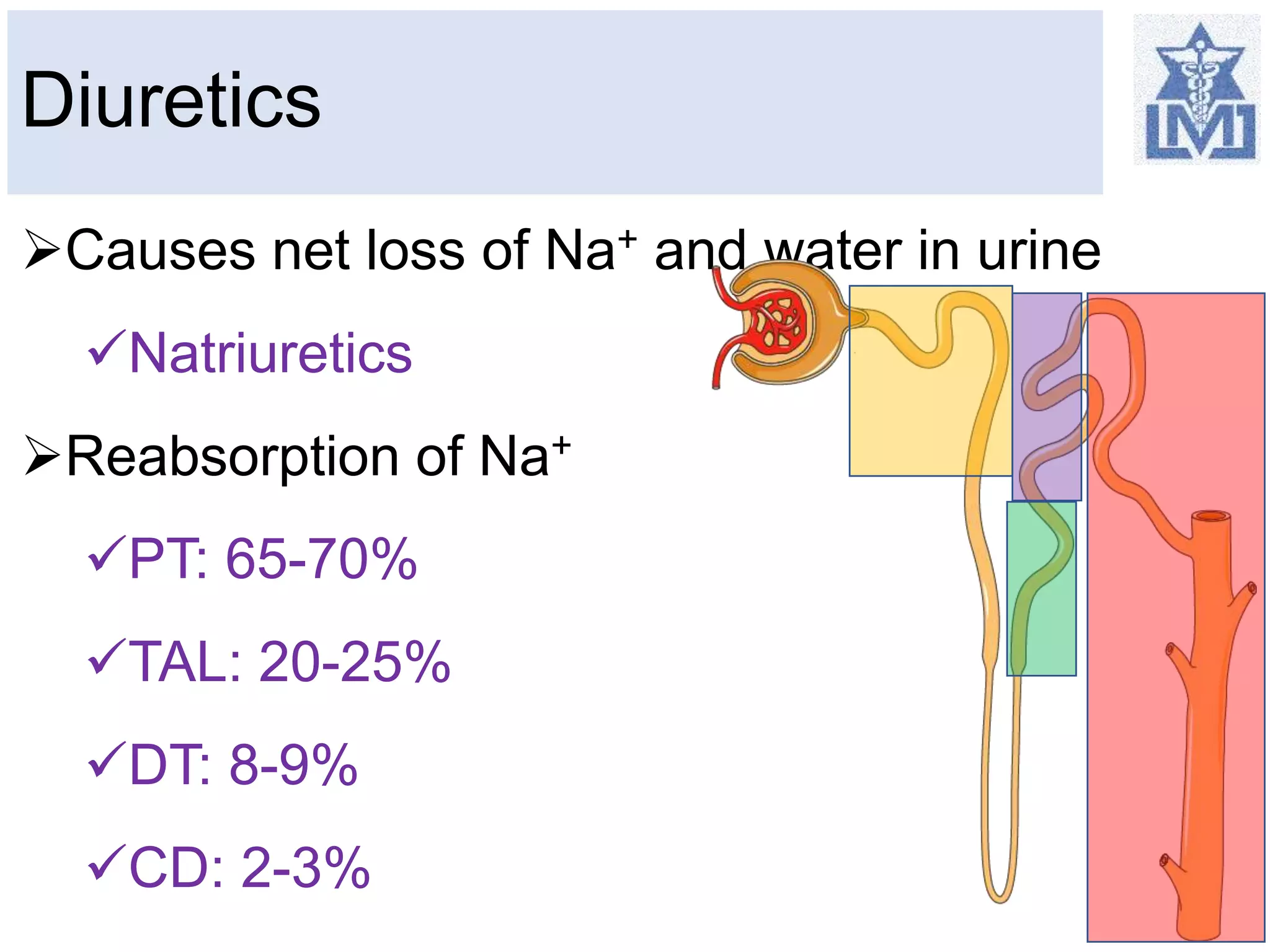
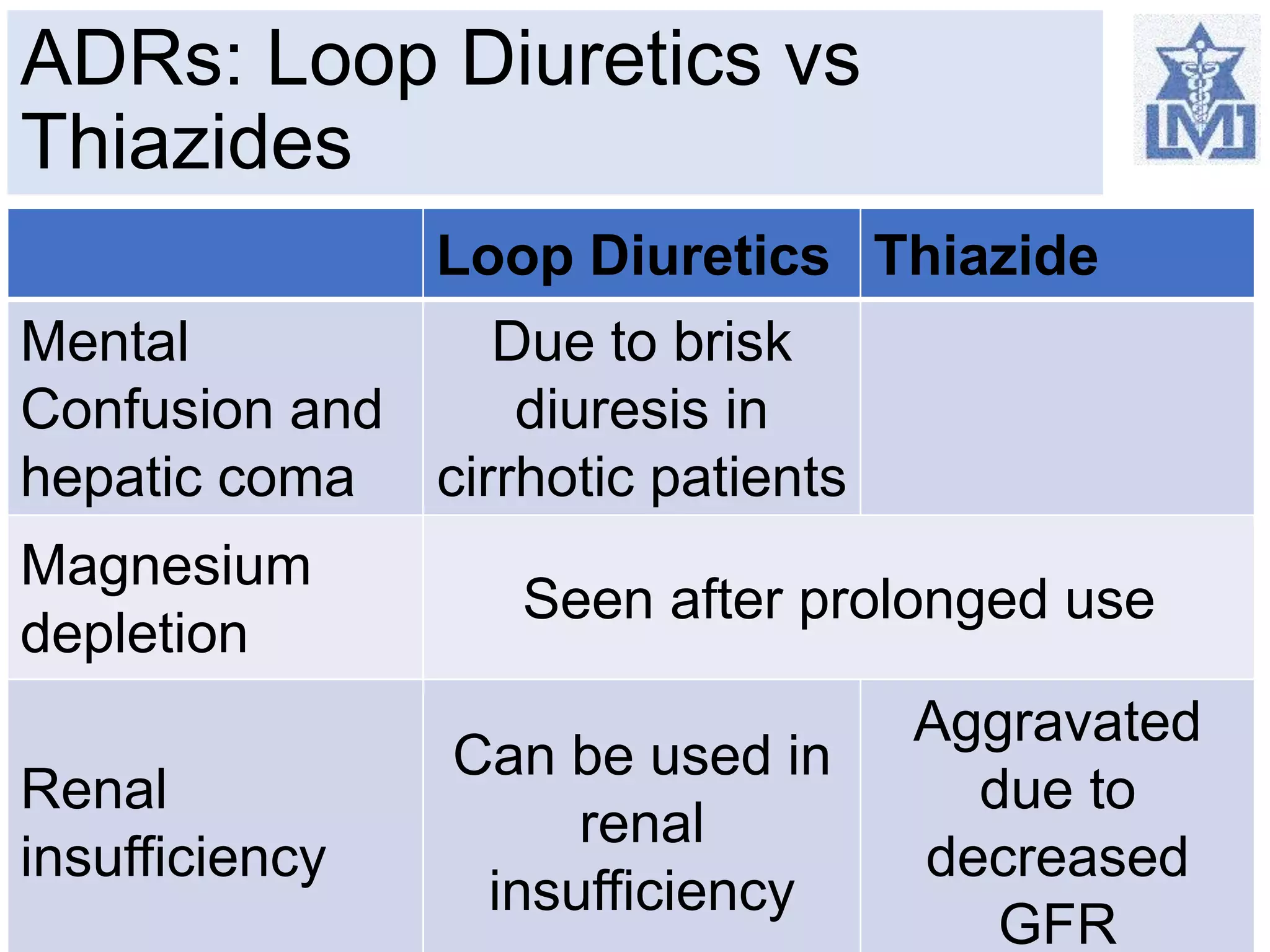
This document provides an overview of diuretics for medical students. It begins by classifying diuretics into high ceiling, medium efficacy, and weak categories. It then focuses on the mechanisms and effects of loop diuretics like furosemide and thiazide diuretics. Loop diuretics work by inhibiting sodium-potassium-chloride transport in the thick ascending limb, while thiazides inhibit sodium-chloride transport in the distal tubule. The document compares the adverse effects and drug interactions of these classes. It concludes by emphasizing how diuretics are commonly used to treat hypertension and edema and can interact with other drugs.