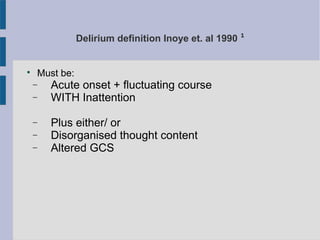
Delirium is a common condition affecting approximately 30% of older adult inpatients and anywhere from 10-50% of older patients who have had surgery. It is defined as an acute onset of fluctuating mental status changes, inattention, and either disorganized thinking or altered level of consciousness. Delirium can present as hyperactive, hypoactive, or mixed. The first steps in assessing delirium are to explore potential causes such as infection, pain, constipation through tests like bloodwork and imaging, and to treat the underlying cause. Non-pharmacological interventions like reassurance and redirection are preferred, with medication being a last resort option. It is important to involve nursing, occupational therapy, and other experienced colleagues for