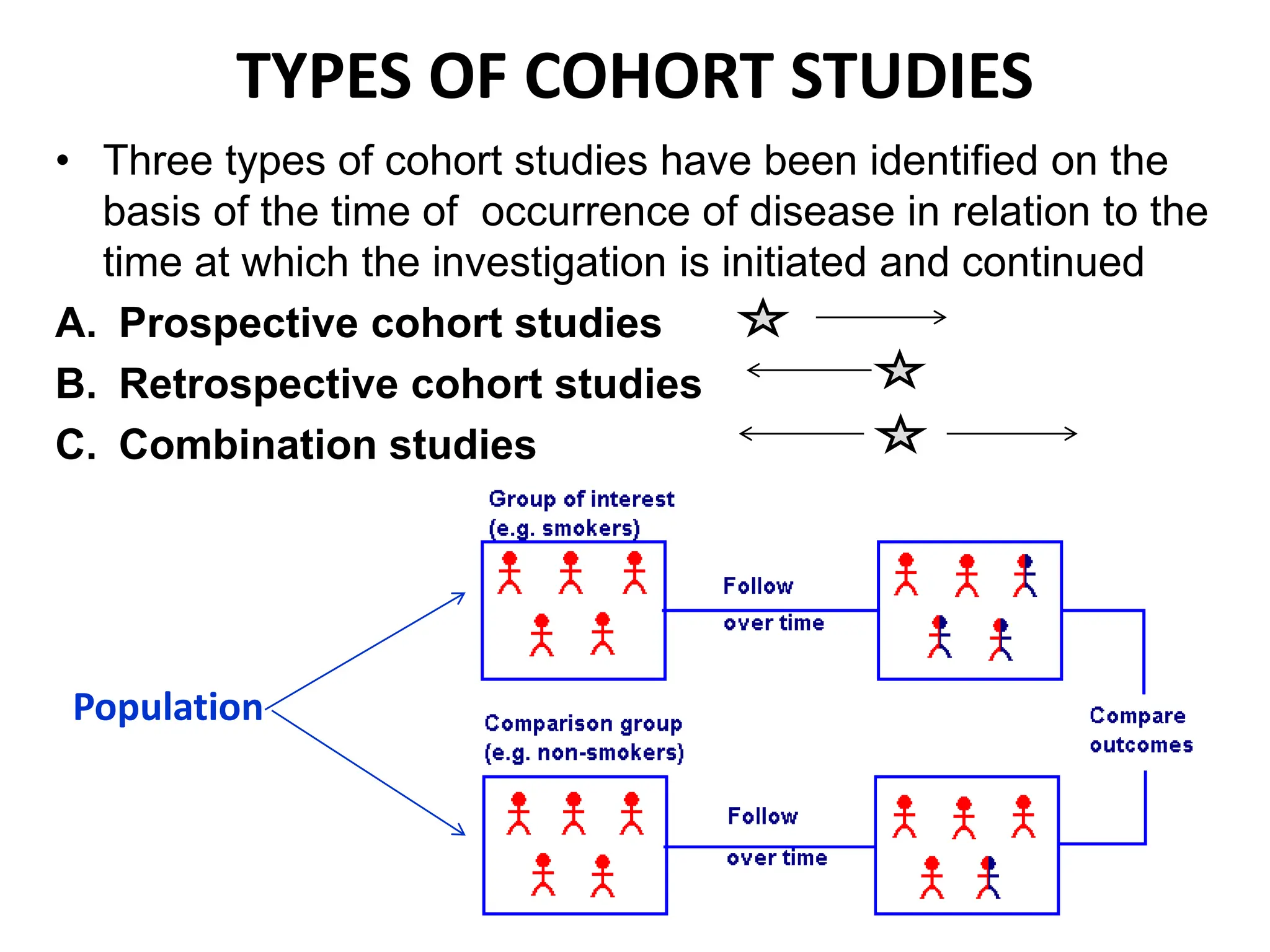
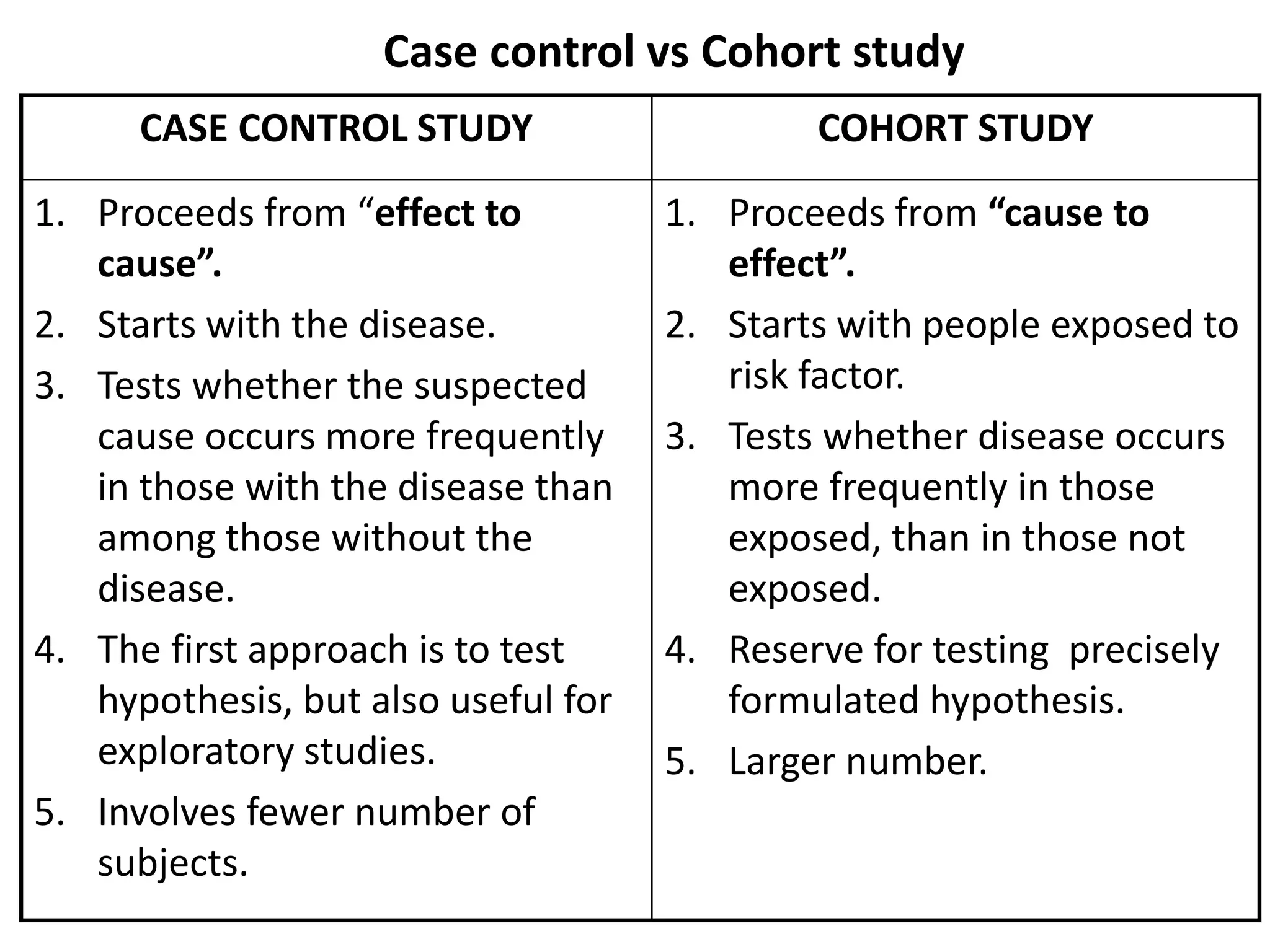
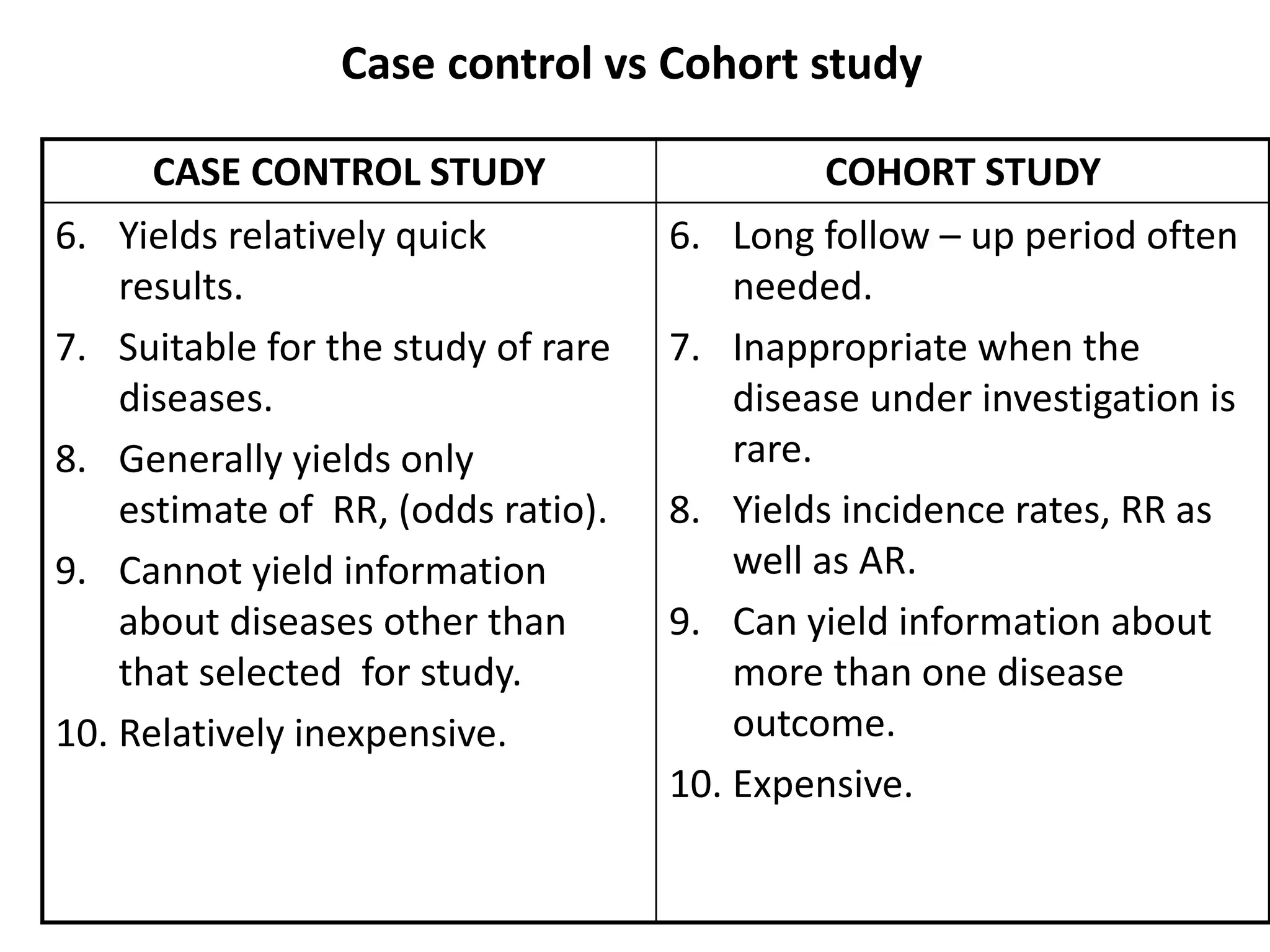
The document outlines the concept, types, and procedures of cohort studies, which investigate the relationship between a suspected cause and disease by observing groups sharing common characteristics over time. It highlights the importance of careful selection of study cohorts, data collection on exposures, and analysis of outcomes to determine risks associated with various exposures. The advantages and disadvantages of cohort studies are discussed, with emphasis on their capacity to calculate incidence rates and assess the strength of associations, while also noting challenges such as cost, attrition, and the need for substantial follow-up.