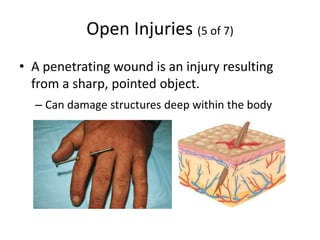
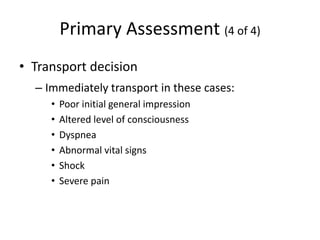
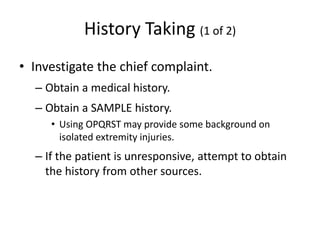
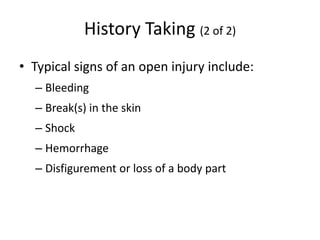
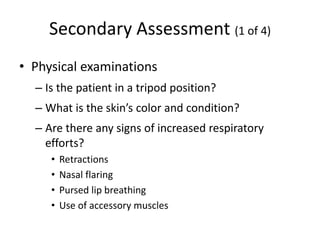
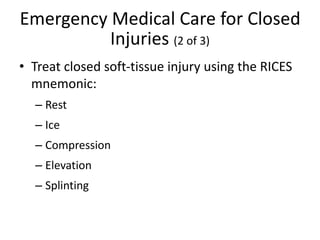
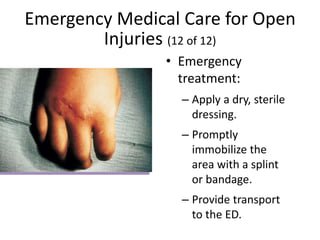
This document provides information on soft tissue injuries, including the skin, closed injuries, open injuries, and burns. It discusses the anatomy and physiology of the skin, mechanisms of injury, types of soft tissue trauma, patient assessment, and emergency medical treatment for these various injuries. Soft tissue injuries are common and range from minor abrasions and cuts to serious internal bleeding and life-threatening situations. Proper assessment and treatment is needed to control bleeding, prevent infection, treat for shock, and protect and dress wounds.