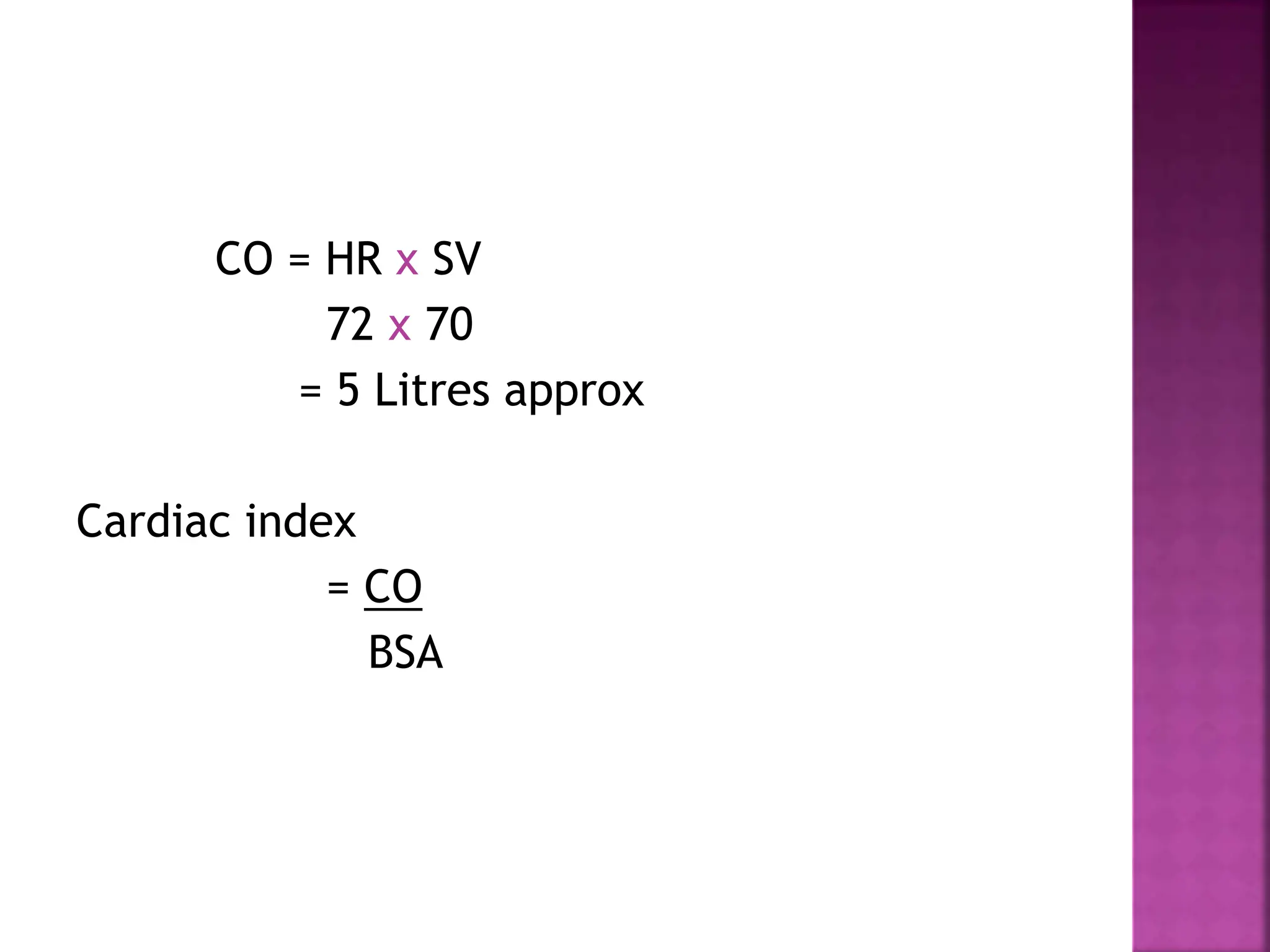
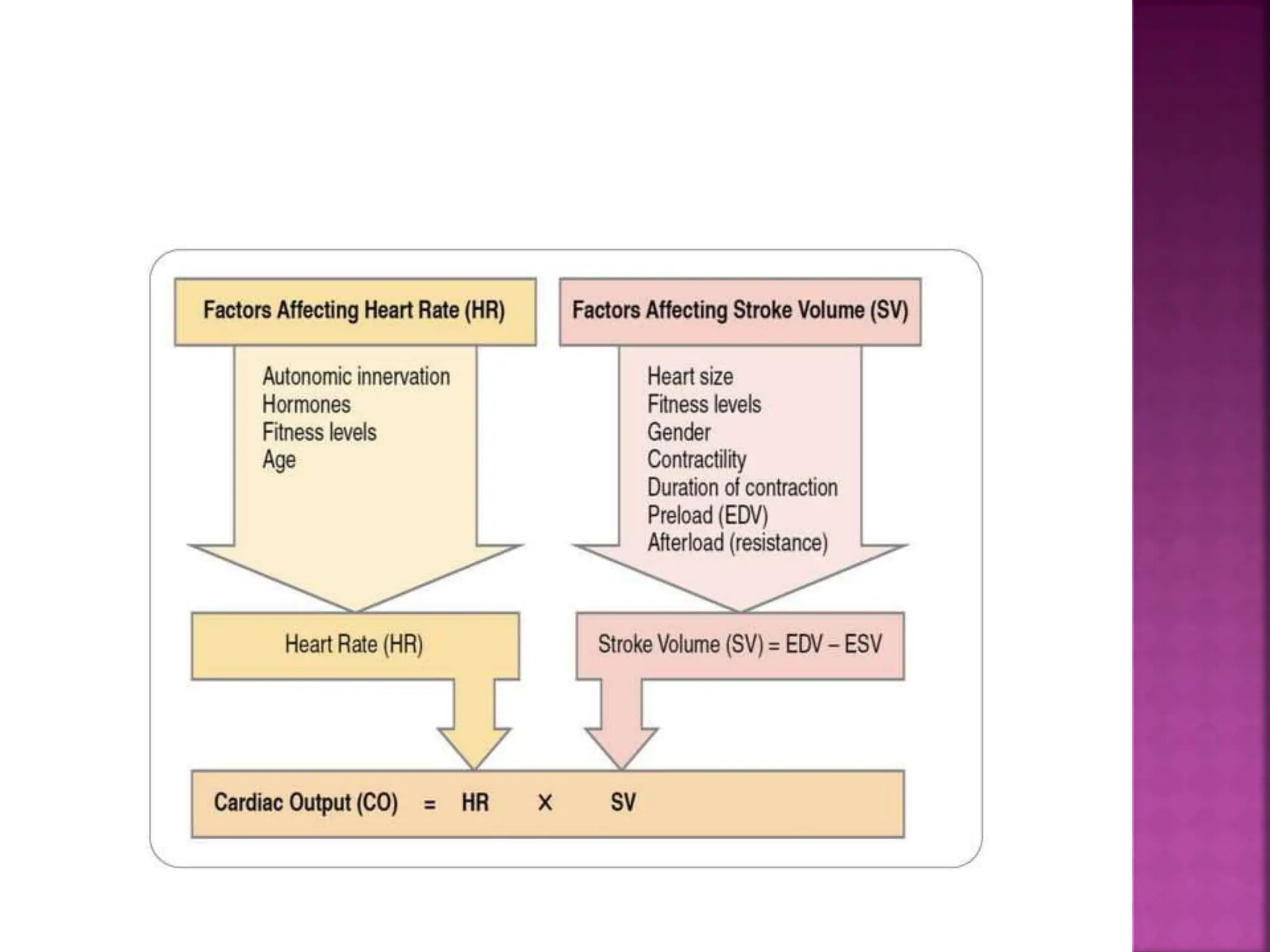
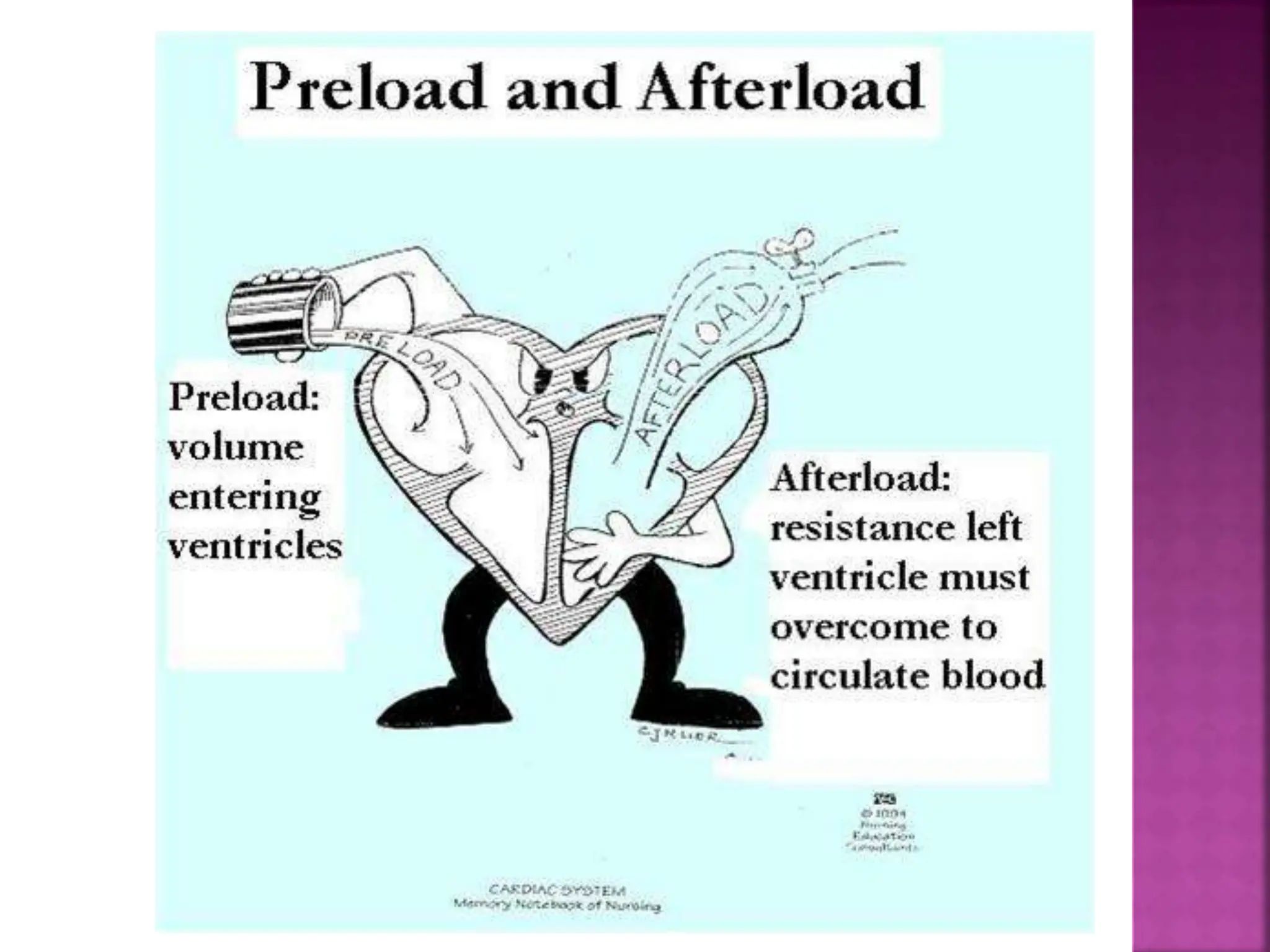
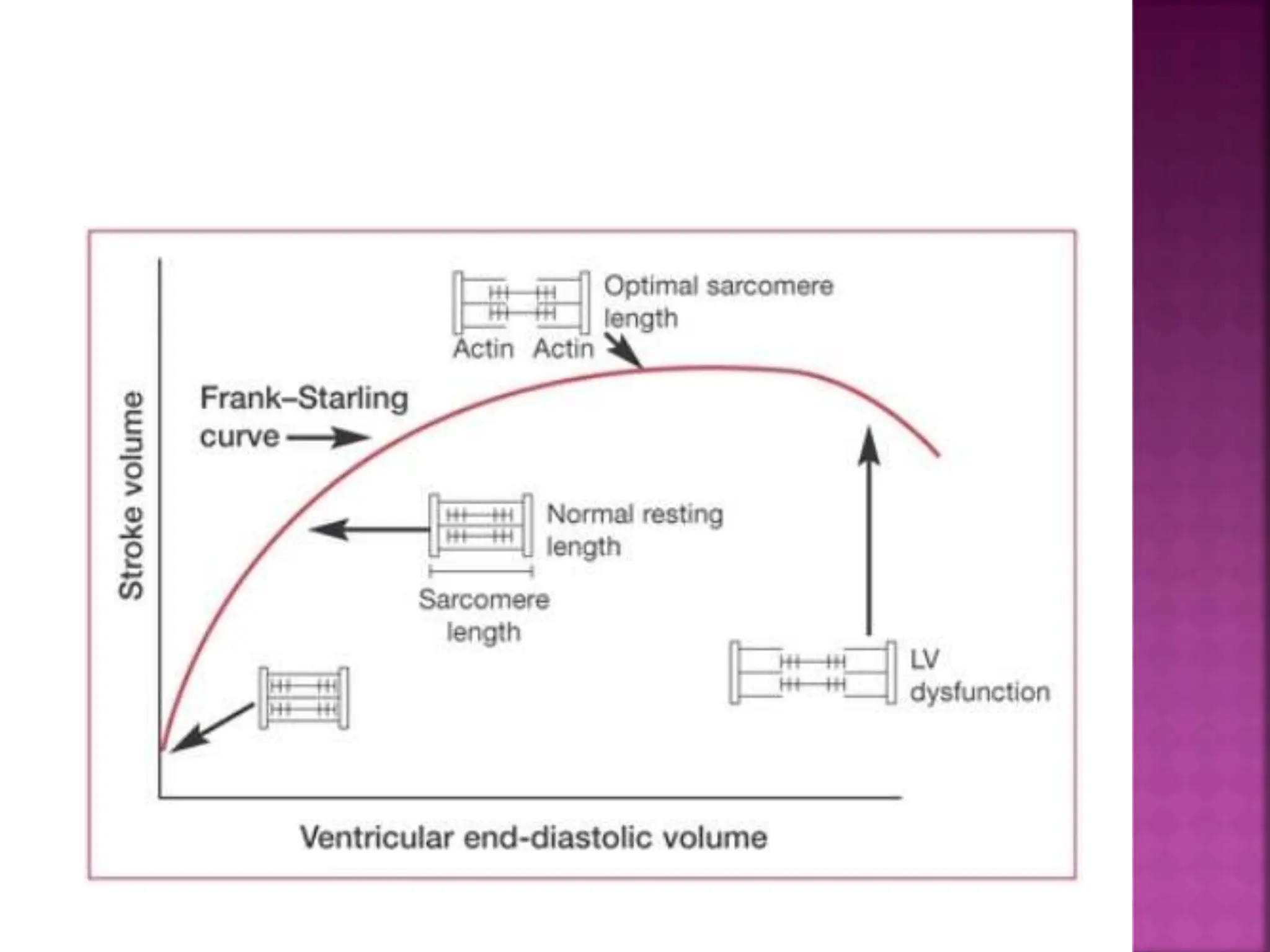
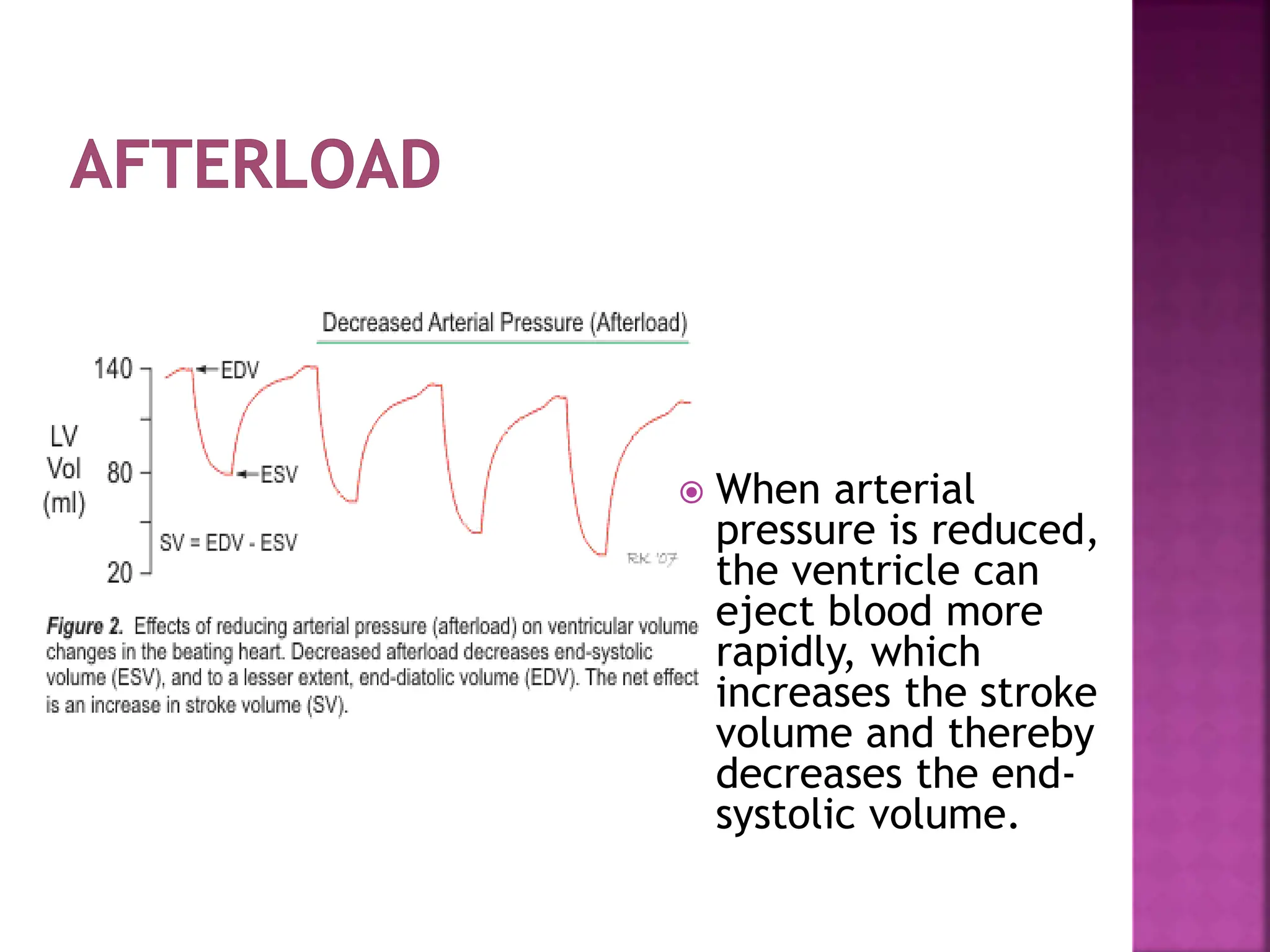
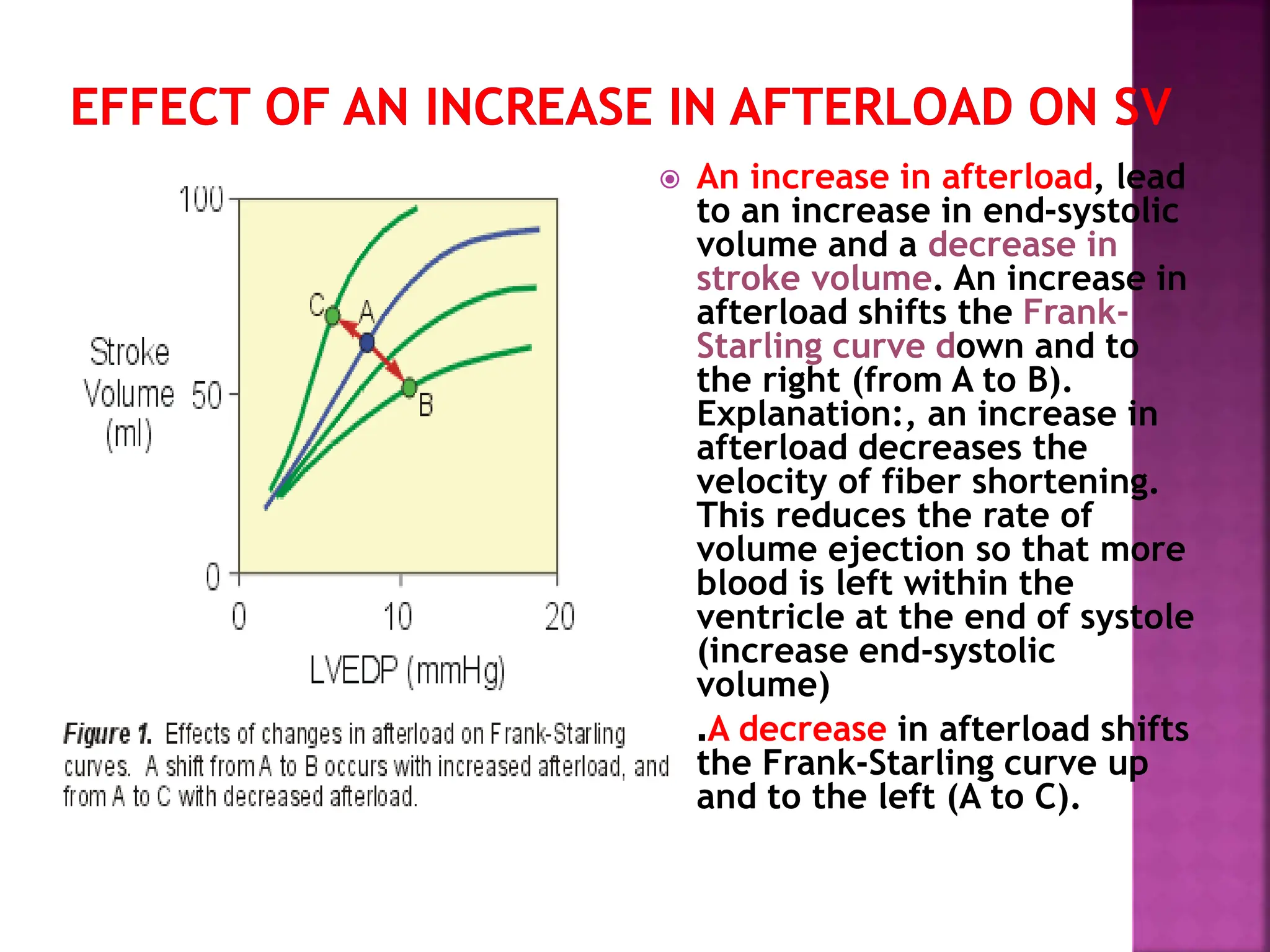
The document explains cardiac output as the volume of blood pumped by the heart each minute, influenced by heart rate and stroke volume. It discusses concepts such as preload, afterload, contractility, and factors affecting stroke volume, while also addressing the heart's response to changes in venous return. Additionally, it mentions the effects of anesthetic drugs on the cardiovascular system, including their vasodilatory actions and negative impact on contractility.