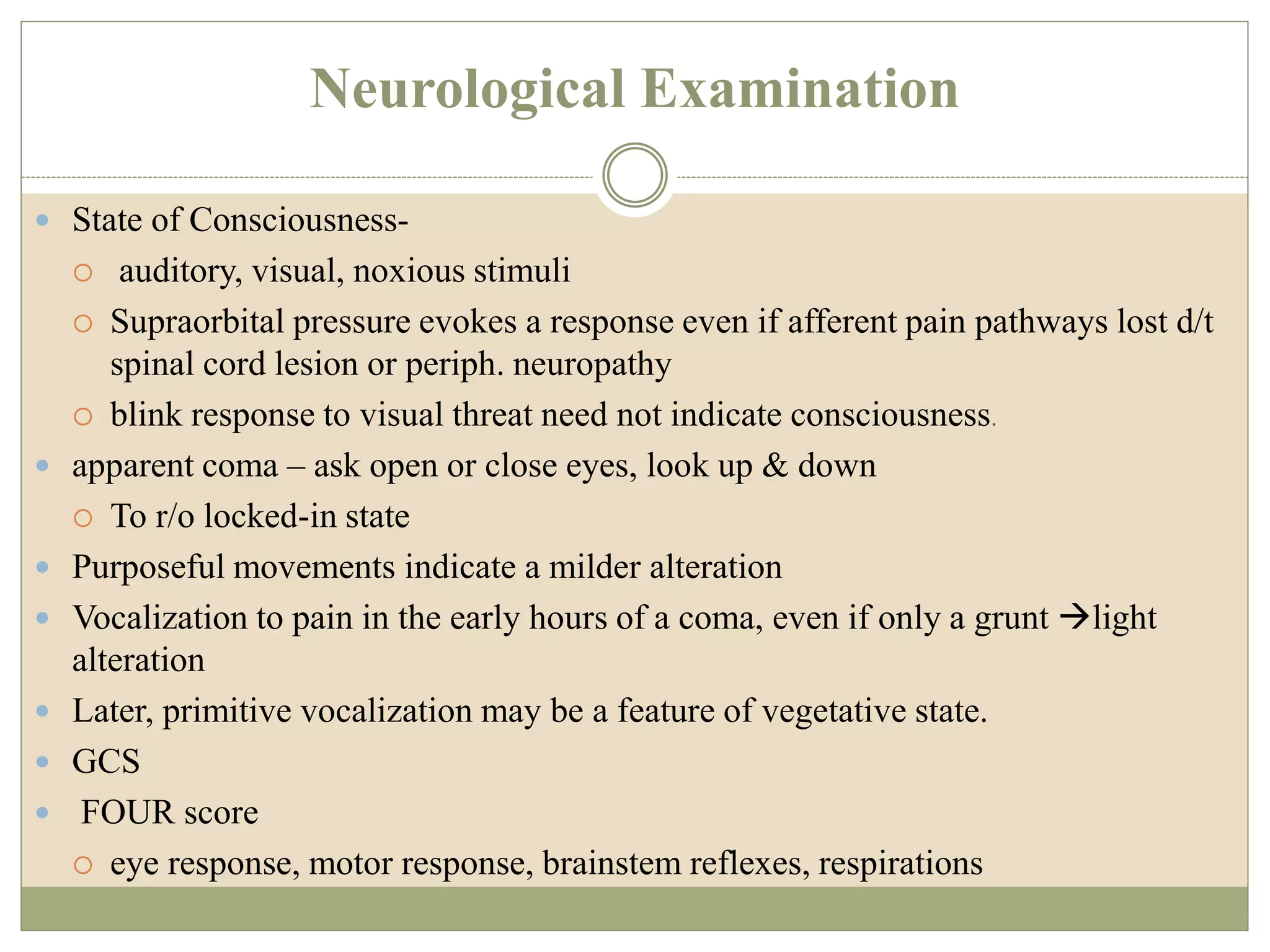
1) Stupor and coma are states of decreased or absent responsiveness that require evaluation to identify potentially reversible causes and provide emergency treatment.
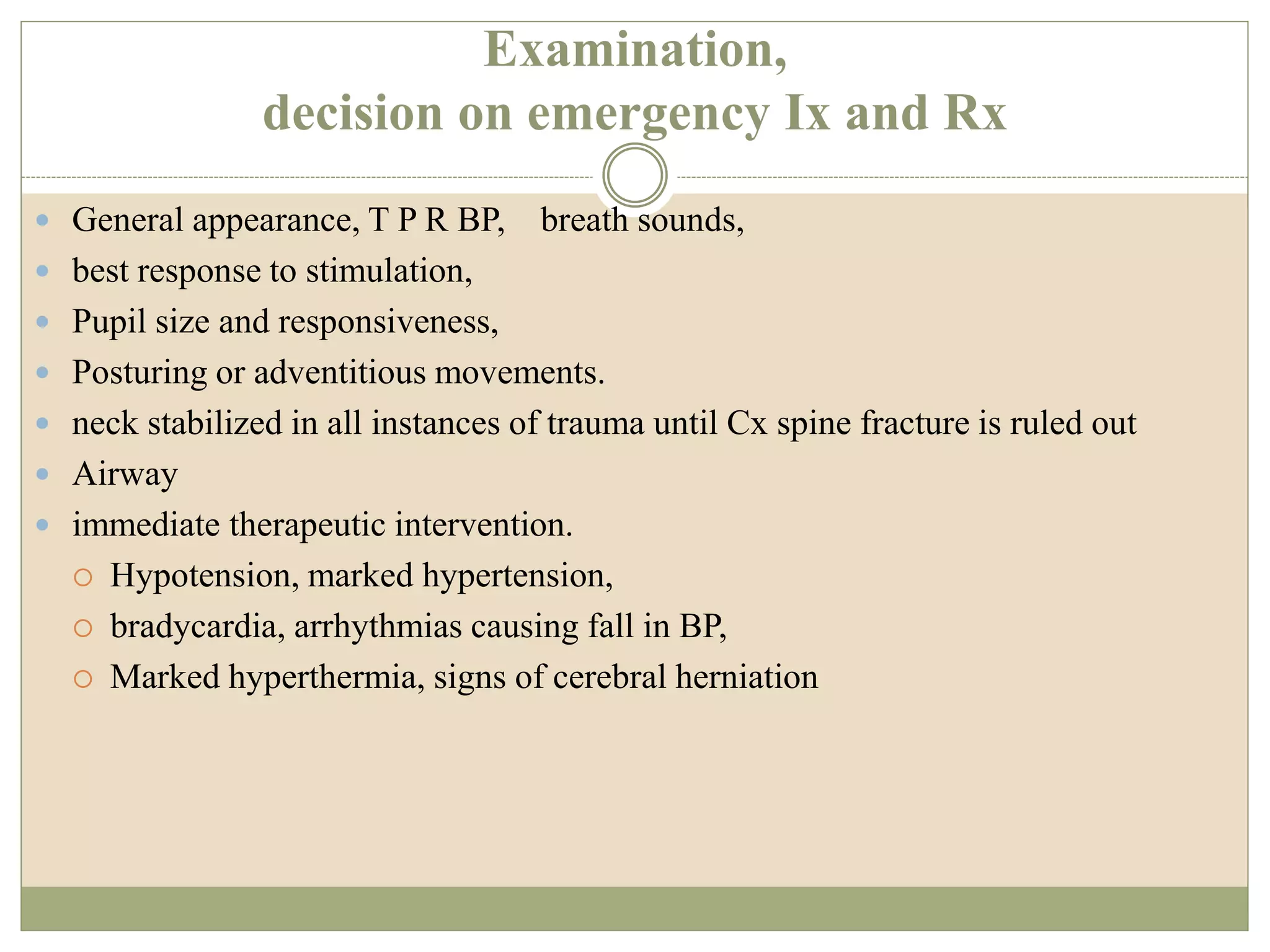
2) The initial approach involves stabilizing vital functions, treating potentially reversible causes, obtaining history, and performing a full neurological examination.
3) Emergency treatment may include supplemental oxygen, IV thiamine, glucose, and antibiotics depending on suspected causes identified from history and examination.