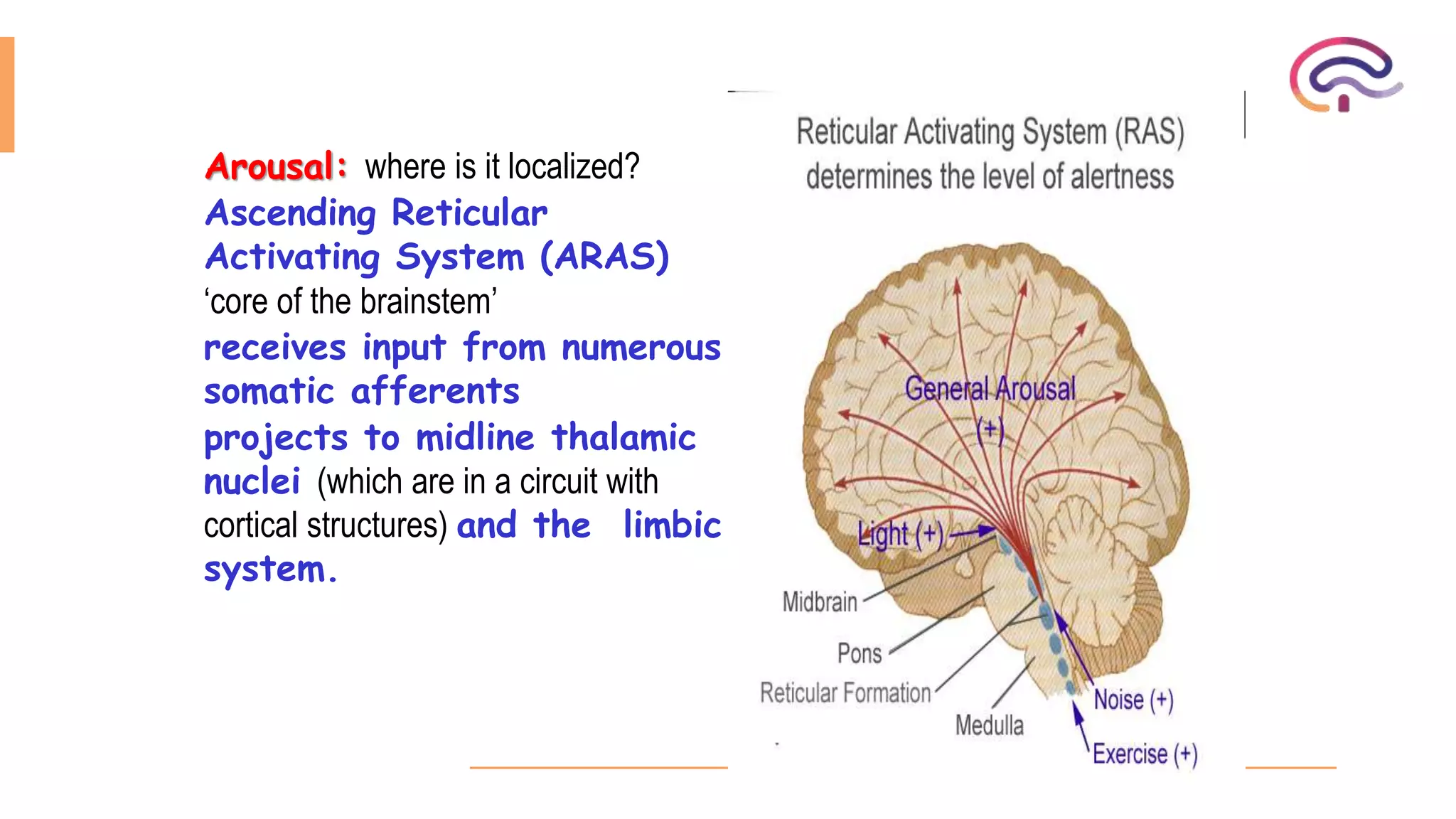
1. The document discusses the approach to evaluating and managing a comatose patient. It defines consciousness and the components of arousal and content of consciousness.
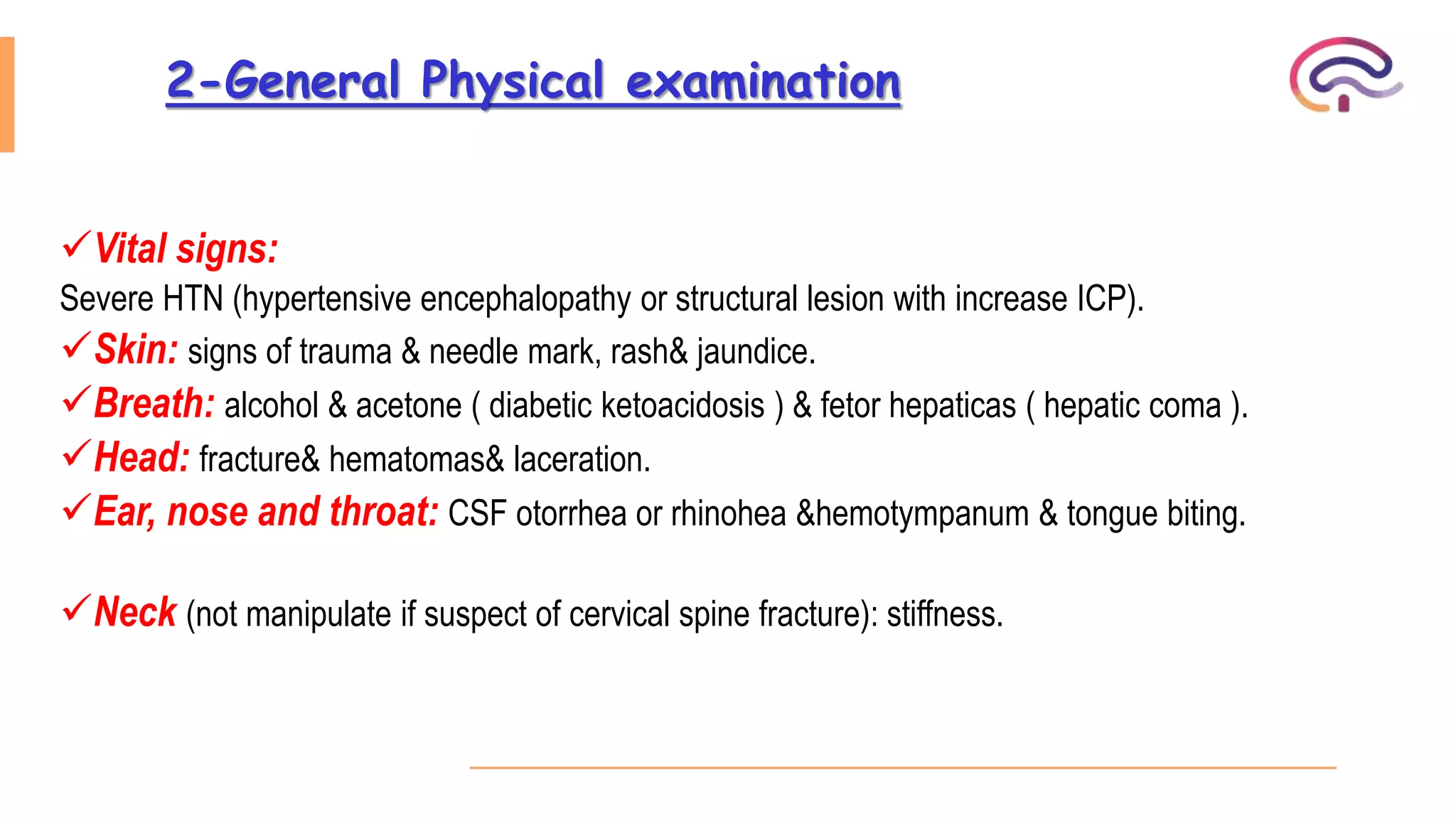
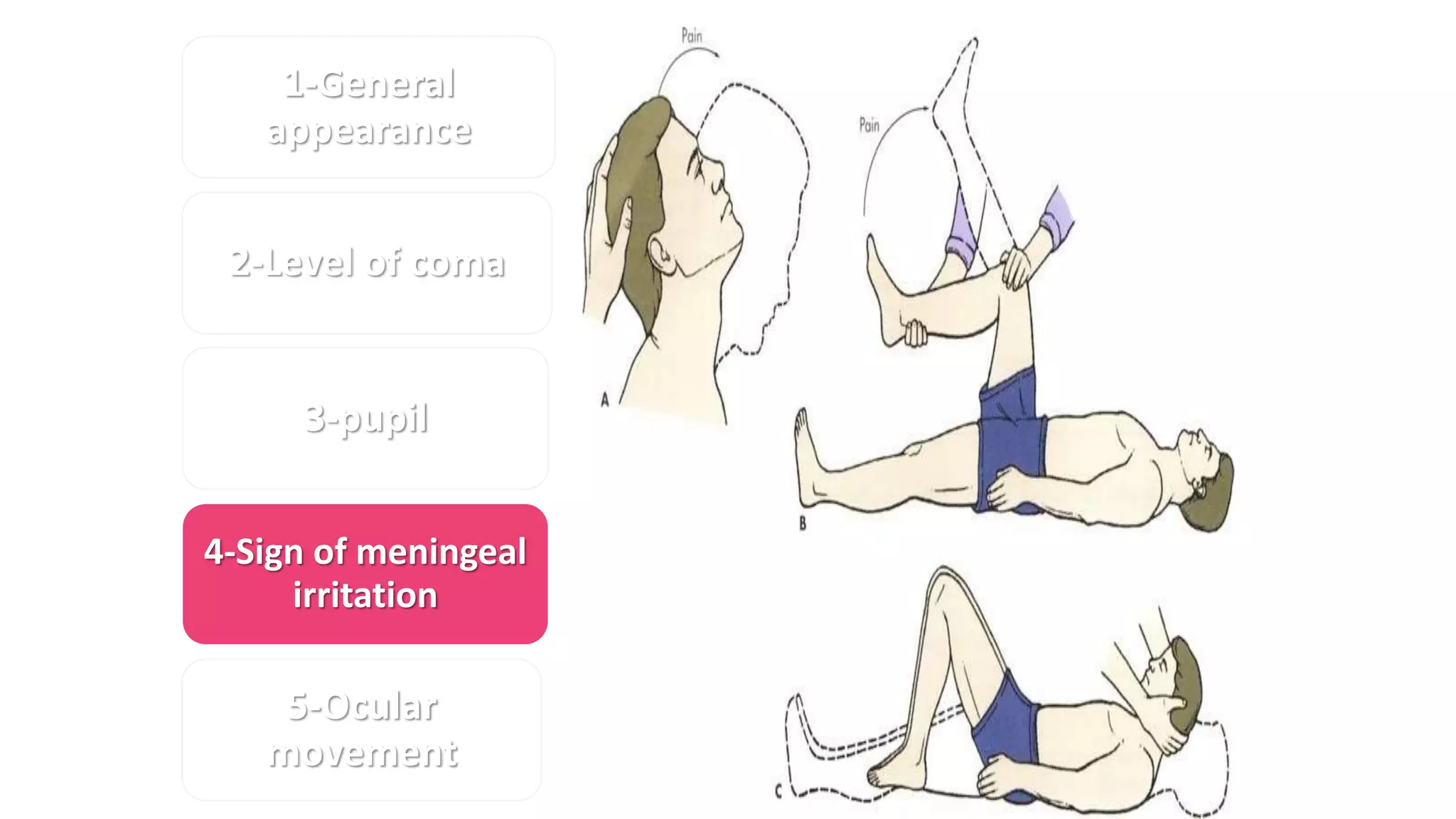
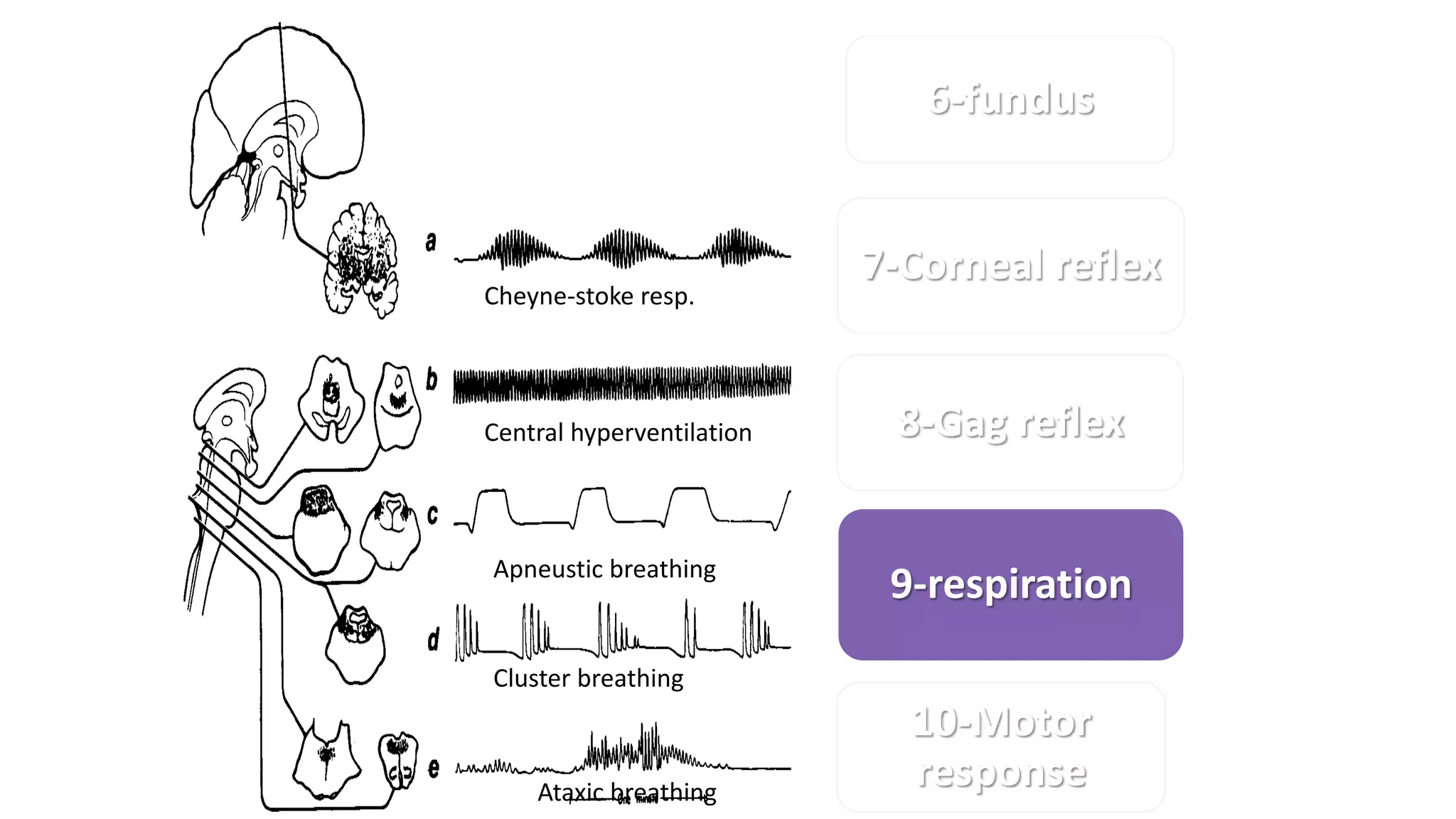
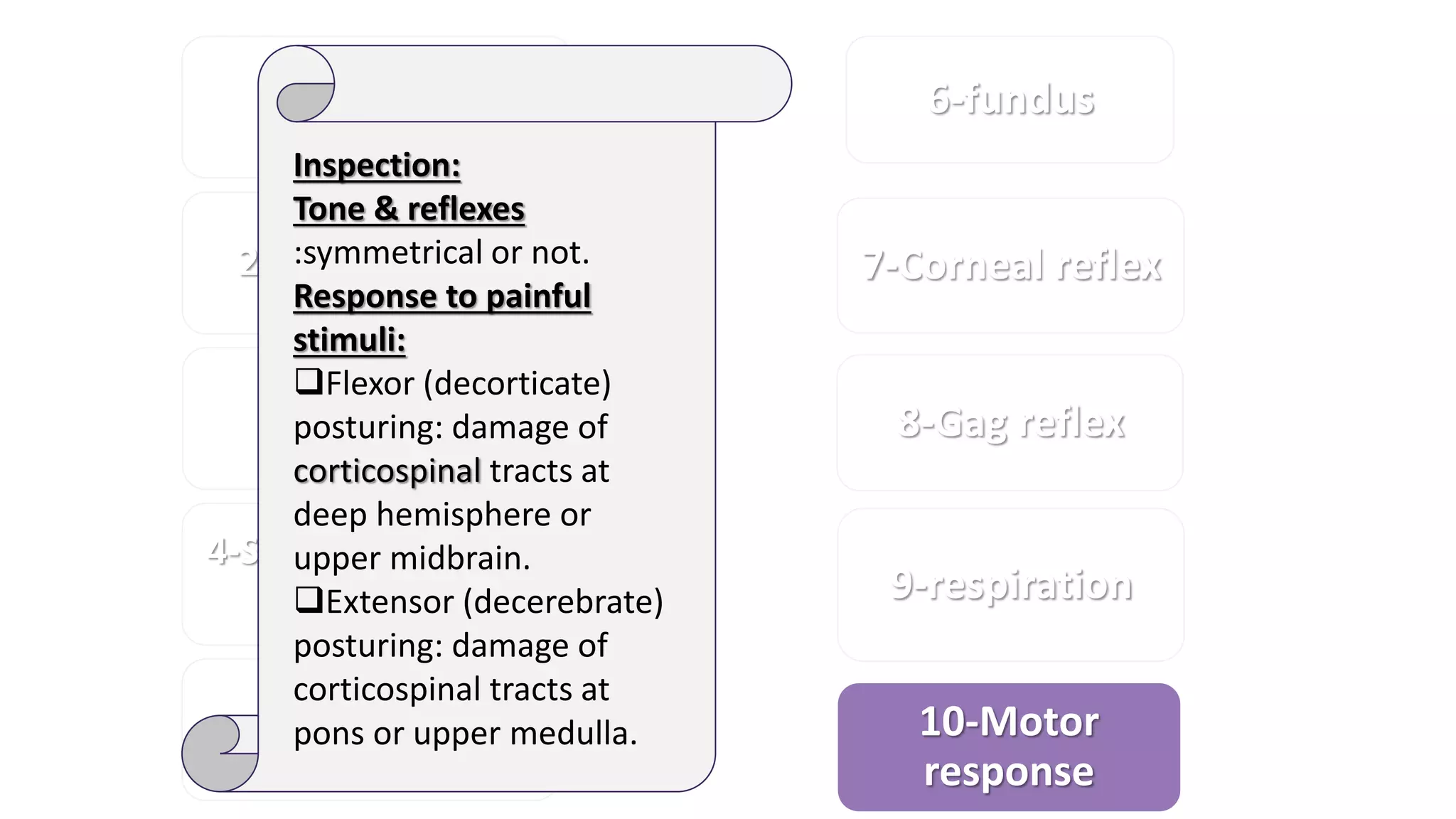
2. Evaluation of a comatose patient involves obtaining a detailed history, performing a physical exam including neurological assessment of pupil size and reactivity, eye and motor movements, and determining the level of coma.
3. Management begins with addressing airway, breathing, and circulation (ABCs), treating potentially life-threatening metabolic disorders, evaluating for increased intracranial pressure, and providing supportive care measures.