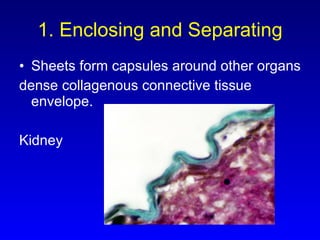
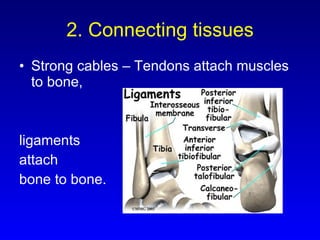
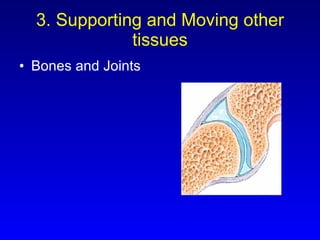
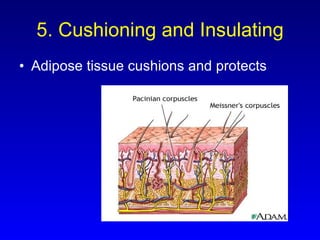
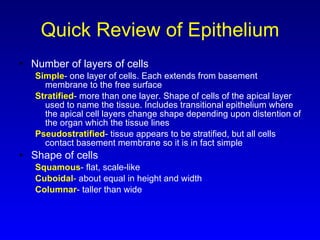
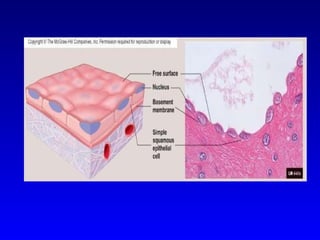
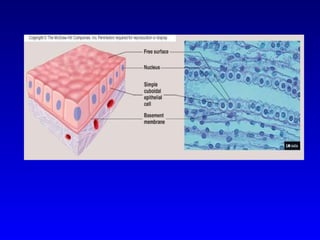
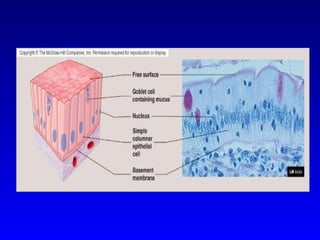
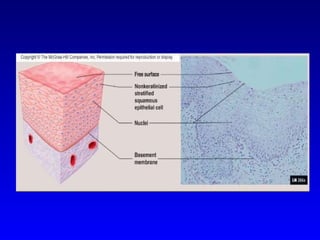
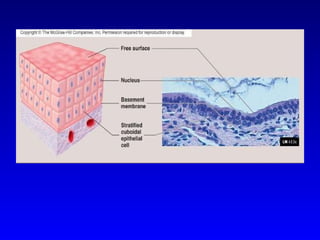
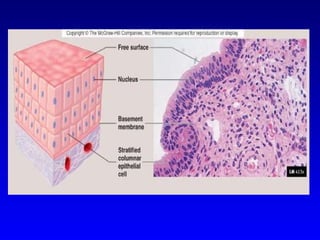
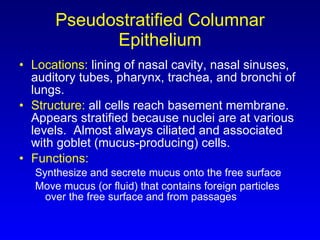
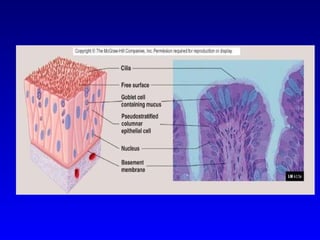
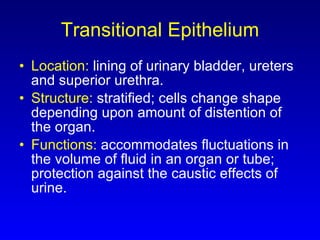
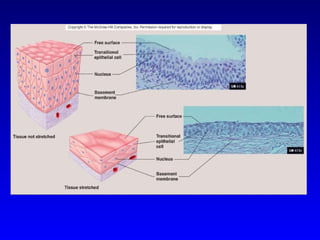
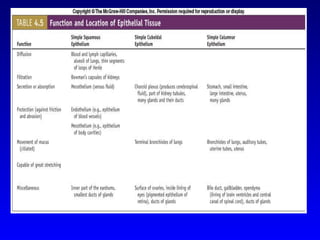
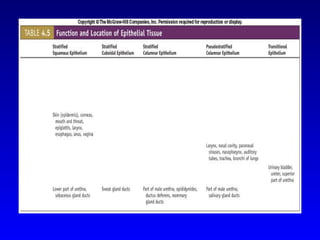
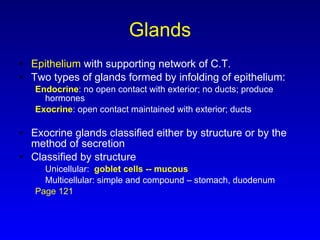
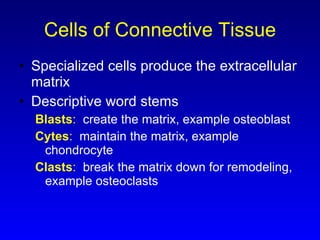
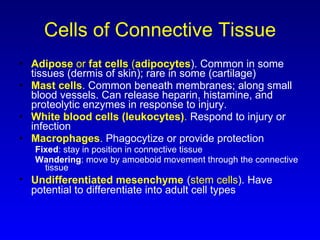
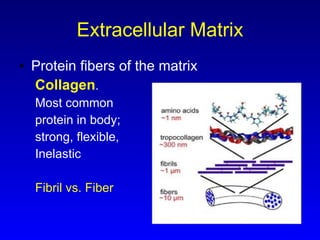
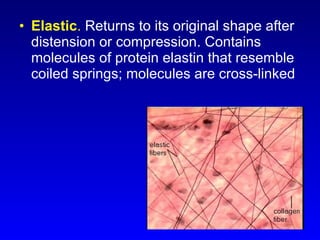
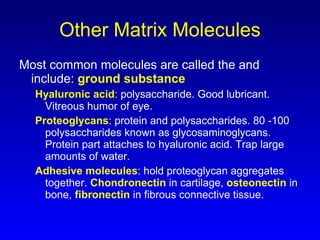
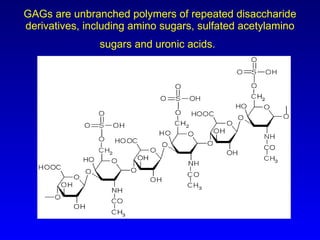
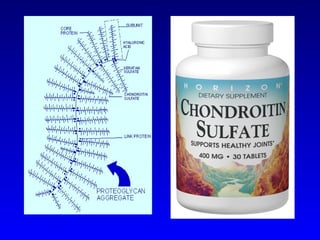
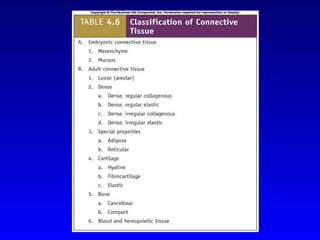
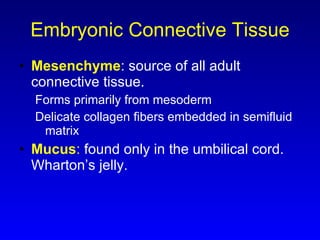
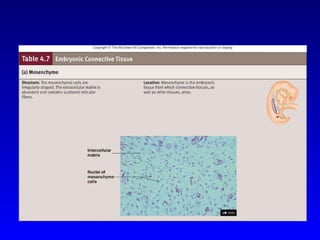
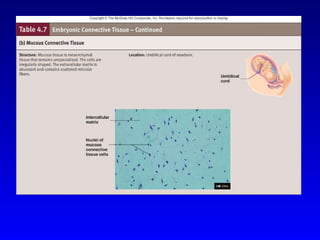
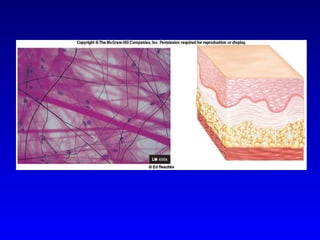
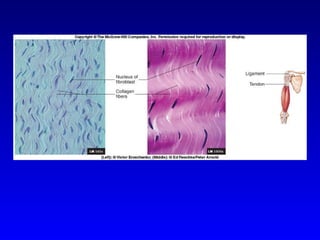
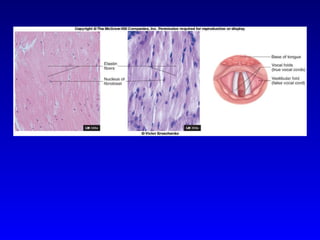
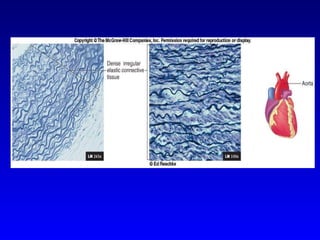
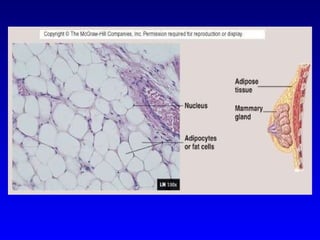
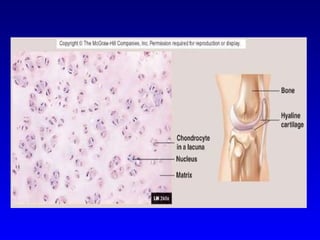
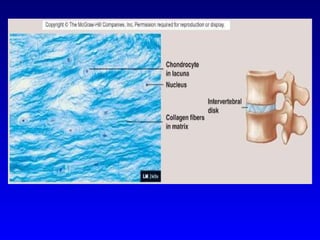
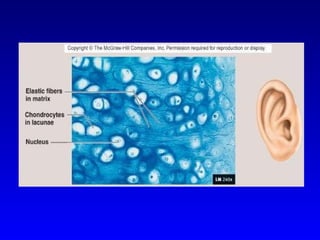
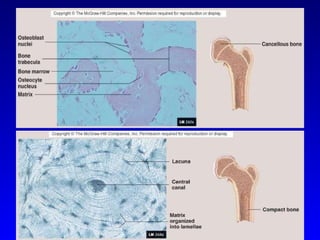
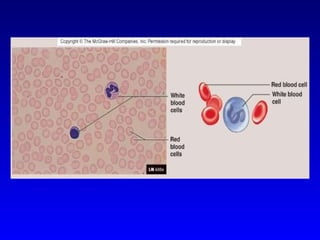
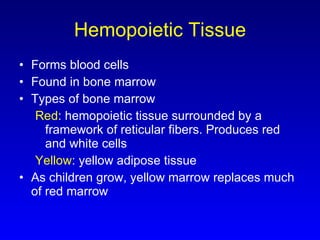
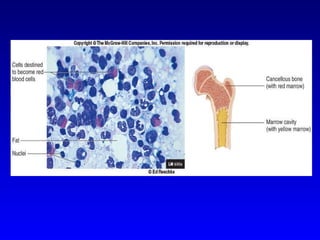
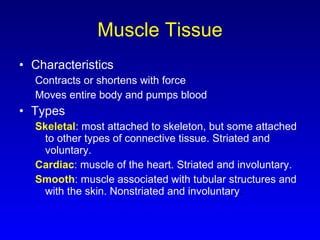
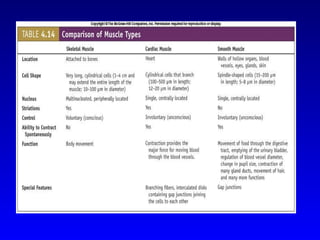
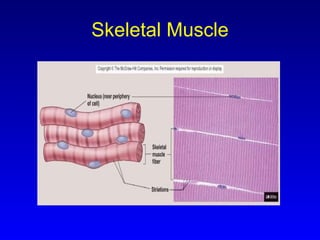
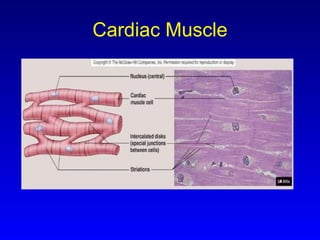
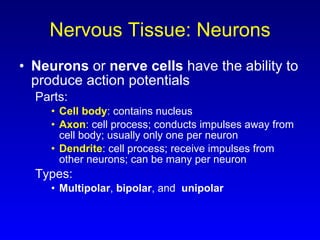
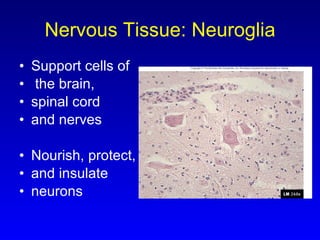
The document provides an overview of histology topics including the four primary tissue types, characteristics of epithelial and connective tissues, and an introduction to muscle and nervous tissues. It discusses the major characteristics and functions of epithelial tissues like simple squamous, simple cuboidal, stratified squamous, and pseudostratified columnar epithelium. It also summarizes the cells, extracellular matrix, and functions of the main types of connective tissues including loose connective tissue, cartilage, bone, and blood.