Adhesion in dentistry
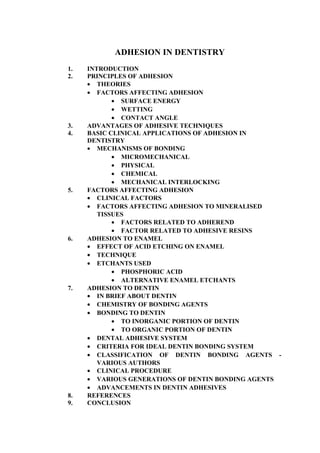
- 1. Sree Ganeshaya Namaha ADHESION IN DENTISTRY 1. INTRODUCTION 2. PRINCIPLES OF ADHESION • THEORIES • FACTORS AFFECTING ADHESION • SURFACE ENERGY • WETTING • CONTACT ANGLE 3. ADVANTAGES OF ADHESIVE TECHNIQUES 4. BASIC CLINICAL APPLICATIONS OF ADHESION IN DENTISTRY • MECHANISMS OF BONDING • MICROMECHANICAL • PHYSICAL • CHEMICAL • MECHANICAL INTERLOCKING 5. FACTORS AFFECTING ADHESION • CLINICAL FACTORS • FACTORS AFFECTING ADHESION TO MINERALISED TISSUES • FACTORS RELATED TO ADHEREND • FACTOR RELATED TO ADHESIVE RESINS 6. ADHESION TO ENAMEL • EFFECT OF ACID ETCHING ON ENAMEL • TECHNIQUE • ETCHANTS USED • PHOSPHORIC ACID • ALTERNATIVE ENAMEL ETCHANTS 7. ADHESION TO DENTIN • IN BRIEF ABOUT DENTIN • CHEMISTRY OF BONDING AGENTS • BONDING TO DENTIN • TO INORGANIC PORTION OF DENTIN • TO ORGANIC PORTION OF DENTIN • DENTAL ADHESIVE SYSTEM • CRITERIA FOR IDEAL DENTIN BONDING SYSTEM • CLASSIFICATION OF DENTIN BONDING AGENTS - VARIOUS AUTHORS • CLINICAL PROCEDURE • VARIOUS GENERATIONS OF DENTIN BONDING AGENTS • ADVANCEMENTS IN DENTIN ADHESIVES 8. REFERENCES 9. CONCLUSION
- 3. ADHESION IN DENTISTRY INTRODUCTION: After observing the industrial use of phosphoric acid to improve adhesion of paints and resin coatings to metal surfaces, Buonocore, in 1955, applied acid to teeth to “render the tooth surface more receptive to adhesion”. Buonocore’s pioneering work led to major changes in the practice of dentistry. Today we are in the age of the adhesive dentistry. Traditional mechanical methods of retaining restorative materials have been replaced, to a large extent, by tooth conserving adhesive methods. The concepts of large preparations and extension and prevention, proposed by Black in 1917, have gradually been replaced by smaller preparations and more conservative techniques. One major problem in restorative dentistry is the lack of proper union between the restorative material and the tooth surface. The process of inventions over a period of time have led to the development of arioso technique and modalities which help in adhesion and thereby reducing the tooth restoration gaps. Bonding / adhesion which was introduced into dentistry by the concept of acid etching by Buonocore in 1955 has changed the term to esthetic dentistry. Bonding in dentistry has improved stabilization and retention of restoration / excessive removal of sound tooth structure and the restorations are better able to transmit and distribute functional stresses across the bonding interface. ADVANTAGES OF ADHESIVE TECHNIQUES : Bonded restorations have a number of advantages over traditional, non adhesive methods. 1) Traditionally, retention and stabilization of restorations often required the removal of sound tooth structure. This is not necessary in many cases, when adhesive techniques are used. 2) Adhesion also reduces micro leakage at the restoration – tooth interface. So by preventing the micro leakage or the ingress of oral fluids and bacteria along the cavity wall – reduces the clinical problems such as post-operative sensitivity, marginal staining and recurrent caries - all of which may jeopardize the clinical longevity of restorative efforts. 3) Adhesive restorations better transmit and distribute functional stresses across the bonding interface to the tooth and have the potential to reinforce weakened tooth structure. 4) In contrast, a traditional metal intracoronal rest may act as a wedge between the buccal and lingual cusps and increase the risk of cuspal fracture. Adhesive techniques allow deteriorating restorations to be repaired and debonded restorations to be replaced with minimal or no additional loss of tooth material. 5) Last but not the least, these adhesive techniques have expanded the range of possibilities for esthetic restorative dentistry. As today’s patient
- 4. pays more attention to cosmetics than ever before, and teeth are a key consideration in personal appearance. Tooth colored materials are used to cosmetically restore and/or recountour teeth with little or no tooth preparation. Advances in dental adhesive technology have allowed the dentist to improve facial esthetics in a relatively simple and economic way. BASIC CLINICAL APPLICATIONS OF ADHESION IN DENTISTRY: To appreciate fully, the clinical application of adhesive techniques, the clinician must have a thorough (1) Understanding of adhesive mechanisms, (2) the materials to be bonded, the (3) dental adhesive systems available and (4) how these are applied to the clinical situation. An adhesive bond between two any two structures can be created by one or more of the following mechanisms (Van Naart 1994). 1) Micromechanical adhesion 2) Physical adhesion 3) Chemical adhesion 4) Molecular entanglement More usually, a combination of some or all of these is active in creating a adhesive bond. So the different bonding mechanisms with dental examples, are presented below. Along with that the adhesion promotes like primers and coupling agents is also given. a) Micro Mechanical Adhesion : Micromechanical adhesion results from the presence of surface irregularities, such as pits and fissure that give rise to microscopic undercuts. The liquid adhesive when applied can penetrate the pits and once set, is locked in the microscopic undercuts. A prerequisite for this form of adhesion is that the adhesive can readily adapt to the surface of the substrate the adaptation is determined by the wettability of the adhesive on the substrate, the ideal situation being that of perfect wetting when the adhesive spreads spontaneously over the surface. Any air / vapour in the pits must be able to escape infront of the advancing liquid. The degree of penetration ay also depend on the pressure used during the application of the adhesive, which helps to force the adhesive into the surface irregularities. In Micromechanical Retention Macro mechanical Retention - Here the adhesive is only able to disengage from substrate by fracturing. - Good wettability is of paramount importance. - Good wettability for macroretention is not a requisite. PRIMERS: Most materials do not normally have surface irregularities ideal for micromechanical bonding. However, the surface may be modified to make it more micromechanically retentive. This can be done either mechanically, for example by grit blasting ceramic and metal surfaces with small aluminum
- 5. oxide particles or chemically, with a primer. Primers are defined as substances which alter the surface morphology of the substrate but do not themselves play a part in bonding process – Wake 1976. These primers are applied to the surface before the adhesive. Eg. Of dental primers H3PO4 acidic primers are also employed – by many of recent DBA’s. Eg. Resin to Enamel bonding. Methacrylate – based resins, such as BisGMA, do not band to enamel, however the surface of enamel can be modified by the application of acidic primes. Here H3PO4 is used it helps by modifying the surface characteristics in enamel in two ways. a) Increases the surface roughness of enamel at the microscopic level, making it possible to bond to this surface by the process of micro mechanical bonding. b) This acid also raises the surface surgery of the enamel – which improves the ability of the resin to adapt closely to the etched enamel surface but only if the surface is thoroughly dried after etching (Baier 1992). Thus, the resin – to enamel bond is essentially micromechanical. 2) Other Forms of Micromechanical Bonding : The resin ceramic bond for veneers and inlays and the resin metal bond for resin bonded fixed partial dentures also relay on primers to modify the surfaces of the restorative material. PHYSICAL ADHESION: When two surfaces come in close proximity to one another, secondary forces of attraction can be generated through dipole-dipole interactions. The molecules must be polar so that they become oriented in a specific way at the interface. This bond polarity is a consequence of asymmetric electronic distribution in the bond. Polar reactions occur as a result of attractive forces between the positive and negative charges on the molecules. The magnitude of the interaction energy is dependent on the mutual alignment of the dipoles, but is usually less than 0.2 eV. This is considerably less than the bond energy of the primary bonds, such a ionic or covalent bonds, which is typically 2.0 to 6.0 eV. This type of bonding is a rapid and reversible process, because the molecules remain chemically intact on the surfaces. Therefore, this weak physical adsorption is also easily overcome by thermal energy and is not suitable if a permanent bond is desired. It following that non polar liquids will not readily bond to polar solids and vice versa, because there is no interaction between the two substances at the molecular level, even if there is a good adaptation Familiar Example of this Problem : Inability of hydrophobic (water-repellent) silicon rubber impression materials to adapt to the hydrophic (water loving) moist surfaces of the soft
- 6. tissues. In the impression materials this problems is overcome by the incorporation of surfactants (Pratten and Craig 1989). CHEMICAL ADHESION: If an adsorbed molecule dissociates on contact with a surface and the constituent atoms rearrange themselves in such a way as to form covalent or ionic bonds, a strong adhesive bond can result. This form of adhesion is known as chemisorption. The feature that distinguishes the chemical bond from the physical type of chemically to their surface of application to form strong bonds and require identifiable reactive groups on both surfaces. Covalent bonding occurs for an isocyanate adhesive, which can bond to soft tissues via surface hydroxyl and amino group. An ionic bond is believed to form between the carboxyl groups of the glass polyalkenoate cements and calcium ions in the enamel and dentin (Wilson 1991). Glass – Polyalkenoate Cement : These form an ionic bond to enamel and dentin, that is so strong that it exceeds the tensile strength of the cement. So, consequently the cohesive fracture of the cement frequently takes place rather than fracture of the adhesive interface. Coupling Agents : As we know, the incompatibility between polar and non polar substances was obvious. Such is the situation when hydrophobic resins such as BisGMA, are to be bonded to dentin or ceramic surfaces. The incompatibility between the adhesive and the substrate can be overcome by the use of a coupling agent. Coupling agent and primer as said before are commonly referred to as adhesion promoters. The difference between the primer is that, coupling agent is integral to the creation of adhesive bond whereas primer helps in adhesion but not an integral part of bonding. Function of coupling agent is to provide a strong link between two materials that would otherwise form an adhesive bond. A coupling agent can be considered as having the general formulae. M-S-R Where H represents – Non polar organo functional gel methacrylate. S spacer – ethyl (-CH2-CH2) / Oxypropyl (-O-CH2-CH2-CH2) R represents a polar functional group such as hydroxyl, carboxyl / silanol. PRINCIPLES OF ADHESION: Word adhesion is derived from the Latin word adharrere which is compound of ad, or to and hoerere or to stick. In adhesive terminology, adhesion or bonding is the attachment of one substance to another. The surface / substrate that is adhered to is termed the ADHEREND. The adhesive / adherent, or in the dental terminology the bonding agent or adhesive system ; defined as the material that, when applied to surfaces of
- 7. substances can join them together, resist separation and transmit loads across the bond. The adhesive strength /bond strength is the measure of the load, bearing capability of the adhesive. The time period during which the bond remains effective is referred to as durability. Adhesion refers to the forces or energies between atoms / molecules at an interface that hold two phases together. In dental literature, adhesion is often subjected to tensile / shear forces in debonding tests and the mode of failure is quantified. If the bond fails at the interface between two substrates, the modes of failures is referred to as adhesive. It is referred to as cohesive if failure occurs in one of the substrates, but not at the interface. But the mode of failure is often mixed. Four Different Theories have been advanced to account for the observed phenomena of adhesion. a. Mechanical Theories : Solidified adhesive interlocks micromechanically with the roughness and irregularities of the surface of the adherend. b. Absorption Theories : All kinds of chemical bonds between the adhesive and adherend, including primary (ionic and covalent) and secondary (hydrogen, dipole interaction and London dispersion) valence forces. c. Diffusion Theories : Adhesion is the result of bonding between mobile molecules. Polymers from each side of an interface can cross over and react with molecules on other side. Eventually, the interface will disappear and the two parts will become one. d. Electrostatic Theories : Electrical double layer forms at the interface between a meal and a polymer making a certain, yet obscure, contribution to the bond strength. The phenomenon of adhesion depends on certain factors, the main factors are ; 1) Surface energy 2) Wetting 3) Contact angle When two substances re bought into intimate contact with each other, the molecules of one substance adhere or are attracted to molecules of another. This force is called adhesion while unlike molecules are attracted, and cohesion when molecules of the same kind are attracted. The material film added to produce the adhesion is known as adhesive, and the material to which it is applied is called the adherend. The principle of adhesion and the factors associated with this phenomenon. Surface Energy: For adhesion to exist, the surfaces must be attracted to one anther at their interface. Concerned to dental structures, enamel which contains primarily hydroxyapatite – has high surface free energy. Wetting: It is difficult to force two solid surfaces to adhere. Regardless of who smooth these surfaces may appear, they are likely to be extremely rough when viewed on an atomic / microscopic scale. Consequently when they are placed in apposition, only the peaks in contact. Because these areas usually constitute
- 8. only a small percentage of total surface area, no perceptible adhesion takes pale. One method of overcoming this difficulty is to use a fluid that flows into these irregularities to provide contact over a greatest part of the surface of the solid. For example : When two polished glass plates are placed one on to of the other and are pressed together, they exhibit little tendency to adhere for reasons previously described. However, if a film of water is introduced between them, considered difficulty is encountered in separating the two plates. The surface energy of the glass is sufficiently great to atleast the molecules of water. To produce adhesion in this manner, the liquid must flow easily over the entire surface and adhere to solid. This characteristic is known as wetting. IF the liquid does not wet the surface of the adherend, adhesion between the liquid and adherend will be negligible or non existent. When surface energy is more wetting is proper. Contact Angle: The extent to which an adhesive wets the surface of an adherend may be determined by measuring the contact angle between the adhesive and the adherend. The contact angle is the angle formed by the adhesive with the adherend at their interface. If the molecules of the adhesive are attracted to the molecules of the adherend as much as or more than they are to themselves, the liquid adhesive will spread completely over the surface of the solid, and no angle will be formed. Thus, smaller the contact angle between the adhesive and an adherend, the better the ability of the adhesive to fill in irregularities on the surface of the adhered. Complete wetting occurs at a contact angle of 0o and no wetting occurs at an angel of 180o . According to this theory of wetting and surface free energy, adhesion to enamel is much easier to achieve than is adhesion to dentin. Enamel contains hydroxyapatite, which ahs high surface free energy whereas dentin is composed of two distinct substrates hydroxyl apatite and collagen, which has low surface energy. In the oral environment, the tooth surface is contraindicated by an organic saliva pellicle and low critical surface tension of approximately 28 dynes/cm. Likewise, instrumentation of the tooth substrate during cavity preparation produces a smear layer with a low surface free energy. Therefore the neural tooth surface should be thoroughly claimed and pretreated prior to bonding procedures to increase its surface free energy and hence to render it more receptive to bonding. FACTORS EFFECTING ADHESION: 1) Clinical factors 2) Factors effecting adhesion to mineralized tissue I. Clinical Factors a) Saliva and Blood Contamination
- 9. These contaminants act in a negative manner for adhesion. Although dentin is a net substance, the constituents of saliva and blood create an environment that can destroy dentin bonding. b) Moisture Contamination From Hand Pieces : Contamination from hand pieces can be due to lack of drying devices on air lines leading from compressor, leakage of plumbing lines or due to condensation of water in air lines. This will definitely effect the bonding mechanism. This can be solved by blowing air from hand piece or syringe on to a dry surface. c) Oil Contamination from Hand Pieces / Air Water Syringes : Oil contamination from airline occurs due to lack of maintenance of air compressors. This can e prevented by using effective oil filters. Oil and water contamination are the most potential and significant factors present in tooth adhesion, because there presence is relatively unknown and the result is unexpected. Note : Bonding to dentin is compromised but the influence on adhesion to etched enamel is less. d) Surface Roughness of Tooth Structure : Increase in surface area created by surface roughness may explain slightly better bonds to dentin. It is possible that mechanical retention may be increased slightly by microscopic roughness produced on dentin and enamel by rotary cutting instruments. e. Mechanical Undercuts in Tooth preparation : f. Fluoride Content of Tooth Increased fluoride content of enamel has shown to resist acid etching. Clinicians generally need double the time to etch the fluoresced enamel. Fluoride presence in dentin appears to influence bonding of adhesive agents negatively (Nystrom Holtan and Douglas 1990). g. Location and Size of Dentinal Tubules : Dentinal canals at the external surfaces of the tooth or near the DEJ have small diameters. As they approach the pulp, they become larger dentinal canals. Such variations in the size o the dentinal tubules can affect adhesion. Hence if canals are small, attachment is less and if canals are large, attachment is enhanced. h) Presence of Plaque, Calculus, Extrinsic Stains / Debris : Presence of above said factors will impair effective bonding. Hence before any bonding procedure the surfaces should be thoroughly cleaned with scalers, abrasive prophy pastes using rubber cusp or with abrasive rotary instruments. i) Presence of Bases / Lines on Prepared Teeth : Varnishes, copal cellulose or polyamide varnishes and resin liners affect the bonding of the subsequently placed restorative material to the tooth surface. Composite resins displaced over glass ionomer liner, the bond of resin to the tooth is less than bond of the glass ionomer to the tooth or the bond resin to glass ionomer. j) Tooth Dehydration :
- 10. Overdrying the dentinal surfaces will cause collapse of exposed collagen. Such collapse may prevent resin infiltration and impair boding. So drying only until the obvious shine of moisture is gone is necessary. k) Presence of Residual Temporary Cements : Dentin / enamel that has been in contact with eugenol – containing temporary cements or state – containing non eugenol temporary cements disturb the bonding of the resin to the tooth surfaces. Parameters Affecting Adhesion to tooth Tissue / Mineralized Tissue : The strength and durability of adhesive depends on several factors. Important parameters may include ; a. Physicochemical properties of adhesive and adherend. b. Structural properties of the adherend. c. Formation of surface contaminants during cavity preparation. d. Development of external stresses that counteract the process of bonding and their compensation mechanisms. e. Mechanism of transmission and distribution of applied loads through the bonded joint. Furthermore: - Oral environment o Subject to moisture o Physical stresses o Changes in temperature and pH o Dietary components o Chewing habits Also considerably influences adhesive interactions between materials and tooth structures. Factors Related to Adherend: a. Physico Chemical Properties of Enamel and Effect of Acid Etching : As the composition and structure of enamel and dentin are substantially different, adhesion to the two tissues will also be quite different. Enamel consists of 96.97% by weight of inorganic material mainly HA. The remaining is 4% - 12% of water and organic material (1% to 2% weight). In the oral environment, an organic pellicle covers the enamel surface creating a chemically complex surface with low reactivity. This results in poor bonding enamel surface. Here the critical surface tension is approximately 28 dynes/cm. The cutting of enamel surface during cavity preparation removes this organic biofilm but does not increase the enamel surface energy. Whereas etching (40%) increases the critical surface energy to 72 dynes/cm. The creation bonding area and surface roughness make bonding of hydrophobic resin possible. b) Physico Chemical Properties of Dentin Composition of dentin by volume is ; Organic : Collagen - Type I - 18% Water 12%
- 11. Inorganic : HA - 70% Dentin has low surface energy 44.8% dynes / cm owing to its high protein content, so wetting of such a low energy surface is difficult and adhesion is hard to achieve. So to achieve adequate wetting on this low surface energy, dentin is conditioned to various treatments to increase the surface free energy and thereby help in bonding properly. Transformed Dentin Structure due to Physiologic and Pathological Process: Dentin is a dynamic substrate subjected to continuous physiologic and pathologic changes in composition and microstructure.Aging causes dentin undergo physiologic dentinal sclerosis and relative sclerosis in response to slow progressive or mild irritation. There is formation of reparative / reactive dentin as a defense mechanism to any injury or caries etc. So this transformed dentin structures due to these physiologic and pathologic process i.e. Sclerosed / reparative dentin ahs areas of complete hypermineralization without tubular exposure, even when etched with an acid. All these morphological and structural changes, result in dentin substrate that is less receptive to adhesive treatment than is normal dentin. d) Smear Layer : When the tooth surface is instrumented with rotary and manual instrument during cavity preparations, cutting debris is smeared over the enamel and dentinal surfaces forming what is termed as smear layer. Definition: Any debris, calcific in nature, produced by reduction or instrumentation of dentin, enamel or cementum or as a ‘contaminant’ that precludes the interaction with the underlying pure tooth tissue. This iatrogenically produced layer of debris has a great influence on any adhesive bond formed between the cut tooth and the restorative material. The morphology, composition and thickness of the smear layer are determined to a large extent by the type of instrument used, the method of irrigation employed and by the site of dentin at which it is formed.Its composition reflects the structure of the underlying dentin mainly containing pulverized Ha and altered collagen, mixed with saliva, bacteria and other grinding surface debris. The thickness of the smear layer has been reported to vary from 0.5 – 5 µm. Although smear layer occludes the dentinal tubules with the formation of smear plugs, the smear layer is porous and penetrated by submicron channels, which allows a small amount of dentinal fluid to pass through. Smear layer is reported to reduce dentinal permeability by 86%. e) Internal and External Dentinal Wetness : The dentinal permeability and consequently, the internal dentinal wetness depend on several factors, including the diameter and length of the tubule, the viscosity of dentinal fluid and the molecular size of substances dissolved in it, the pressure gradient, the surface area available for diffusion, the patency of the tubules, and the rate of removal of substances by pulpal circulation.
- 12. Occlusal dentin is more permeable over the pulp horns than at the centre of the occlusal surface, proximal dentins more permeable than occlusal dentin, and coronal dentin is more permeable than root dentin. High dentinal permeability allows bacteria and their toxin to easily penetrate h dentinal tubules to the pulp, if the tubules are not hermetically scaled. The variability in dentinal permeability makes it a more difficult substrate for bonding than enamel. Removal of the smear layer creates a wet bonding surface on which dentinal fluid excludes from the dentinal tubules. This aqueous environment effects adhesion, because water competes effectively, by hydrolysis, for all adhesion sites on the hard tissue. Early DBA failed primarily because their hydrophobic resins were not capable of sufficiently wetting the hydrophilic substrate. IN addition, bond strengths of several adhesive systems were shown to decrease as the depth of the preparation increased, because dentinal wetness was greater. No significant differences in bond strengths is observed between deep and superficial dentin when smear layer is left intact. Bond strengths of more recent adhesive systems that remove the smear layer appear to be less affected by differences in dentinal depth, probably because of their increased hydrophlicity provides better bonding to the wet dentinal surface. Besides internal dentinal wetness, external wetness / environmental humidity, has been demonstrated to negatively affect bond strengths to dentin. For instance, environmental humidity is affected by rubber dam. The bond strengths obtained with most adhesive systems decrease as the level of humidity/ exte. Wetness in the air arises, but some systems appear to be more sensitive than others. FACTORS RELATED TO ADHESIVE: 1. Physical properties of adhesive – Wettability. 2. Polymerization contraction of restorative resins. Methods of composition of polymerization shrinkage a) Flow b) Hygroscopic expansion c) Elastic modulus d) Cervical sealing 3. Thermal coefficient of expansion 4. Transmission of stress across the restorative tooth interface. 5. Biocompatibility. ADHESION TO ENAMEL: Adhesion to enamel is achieved through acid etching of highly mineralized substrate which substantially enlarges its surface area for bonding. This enamel bonding technique, known as acid-etch technique was introduced by Buonocore in 1955. Enamel etching transforms the smooth enamel surface into an irregular surface with a high surface free energy of about 72 dynes/cm, more than twice that of etched enamel. An unfilled liquid acrylic resin with low viscosity, the
- 13. enamel bonding agent wets the high surface energy and is drawn into the microporosities by capillary attraction. Enamel bonding agents re commonly based on bisGMA/UDMA with diluents such as TEDGDMA and HEMA. The bond between enamel and the restorative material is established by polymerization of monomers inside the microporosities and by copolymerization of remaining carbon – carbon double bonds with the matrix phase of the resin composite, producing strong chemical bonds. Acid etching removes about 10 µm of enamel surface and creates a microporous layer from 5-50 µm deep. Three etching patterns have been described ; Type I: Predominant dissolution of prism core and peripheries left intact – most common. Type II: Predominant dissolution of prism peripheries. Type III: No prism structure is evident. Mostly seen by action of strong chelating agents, but it is also seen with acids. This shows there is no one specific pattern seen here. Different patterns may be due to difference in chemical composition and crystalline orientation. Variation may be seen from site to site or tooth to tooth. Enamel bonding depends on resin tags becoming interlocked with surface irregularities created by etching. Resin tags are formed circularly between enamel prism peripheries (micotags are formed at the cores of enamel primers). A much finer network of thousands of smaller tags is usually found across the end of each rod, where individual HA crystals have been dissolved leaving crypts of outlined by organic material. These fine tags are called microtags. Macro and microtags are the basis of micromechanical bonding. Microtags are more important because of their larger number and grater surface content. The effect of acid etching on enamel depends on several parameters : 1. Kind of acid used 2. Acid concentration 3. Etching time 4. Form of etchant – gel /semi gel / acquired solution gel is preferably – better control. 5. Way in which wetting is activated (rubbing / irritating and or repeated application of fresh acid). Etchant should always be applied in debbing action. It should not be applied in subbringaction, because rubbing action may fracture the thinned enamel rods thereby reducing the depths of the created alleys and irregularities and obliterating what is left of then with fractured enamel pieces. 6. Whether enamel is instrumented before etching. 7. The rinsing time 8. The chemical composition and condition of enamel. 9. Whether enamel is on primary or permanent teeth. Primary teeth – prismless enamel and therefore require longer etching time. 10.Whether enamel is fluoridated, demineralised or stained.
- 14. Effects of acid Conditioning on the Surface Enamel: Generally acid conditioning of enamel 935% - 40% of H3PO4 for 60 seconds) will cause the following changes. 1. Removes residual pellicle to expose the inorganic crystallite component of enamel. 2. In the crystalline part – it causes preferential dissolution of interprismatic enamel first, fooled by top of prisms themselves. The east dissolvable are the sides of prisms. 3. Increases surface area upto 2000 times of its original unetched surface and also increases wettabiliy. 4. It will create valleys and deepening. Valleys in place of interprismatic enamel and top of prisms having circumscribed depressions. Depth of these irregularities will range from 5 µ to 25 µ. 5. Acid etching will expose proteinaceous organic matrix substance of enamel which can to restorations retention if it becomes inadequately embedded within the restorative material. 6. Increases the surface energy with creation of reactive polar sites. 7. Mechanical cleansing and acid etching of enamel will assume removal of substrate, enamel cuticles, salivary deposits, plaque composites and any possible adhesives. 8. The enamel surface, thus exposing a cleanser lesser contaminated and more wettable enamel. 9. Treatment with H3PO3 will add to enamel surface a highly polar phosphate group which will increase the adhesive availability to the enamel surface. PHOSPHORIC ACID AS ETCHANT: - Most commonly used etchant. - Concentration – 30%, 40% 37% with etching time ≤ 15 seconds and washing time of 10-20 seconds } Most acceptable and most receptive enamel surface for bonding. - Calcium dissolution and etching depth increase as the concentration of H3PO4 increases until a concentration of 40% and at higher than this it will start showing reverse effect. - At concentration greater than 50% There occurs a formation of monocalcium phosphate monohydrate on the etched surface which revents any further dissolution. - At concentration less than 27% There forms a precipitate of dicalcium phosphate dehydrate that can not be easily removable. - Etching time also has been reduced from traditional 60 seconds to 15 seconds and its shown that it has shown similar surface roughness and etching pattern as that of 60 seconds. - Currently it is recommended that enamel of teeth need not be etched for more than 15-20 second except for the enamel which is acid resistant because of high fluoride content. Primary teeth also require longer etching time since the enamel is more aprismatic than that of permanent
- 15. teeth. Advantages of shorter etching time it yields acceptable bond strengths while conserving enamel and saving time. - Rinsing time is important. R.T. of atleast 15 second is important to remove dissolved CaPO4, which otherwise might impair infiltration of monomers into the etched enamel microporosities, from the etched surface. - Recently rinse time of 1 second have been shown not to impair bond strength/ promote microleakage at the enamel site. - The use of ethanol to remove residual water from the etched pattern has been reported to enhance the ability of resin monomers to penetrate the surface irregularities (Gwinett 1992, Qusit V, Quist J 1985). - Modern primers frequently contain drying agents such as ethanol / acetone, with a similar effect. ALTERNATIVE ENAMEL ETCHANTS: As H3PO4 is said to be more aggressive, other alternatives have been suggested like ; 1) EDTA 2) Pyruvic acid 3) Sulphuric acid Ethylene diamine tetraacetic acid – is a strong decalcifying agent, promotes only low bond strength to enamel, probably being EDTA does no etch preferentially. Pyruvic acid: 10% buffered with glycine to a pH of about 2.2, promotes high bond strengths to enamel, but has been found to be in practical because of its instability. Sulphuric acid: 2% used for 30 seconds has shown to be as effective as H3PO4 whereas high H2SO4 concentration produce heavy crystal deposits which interfere with bonding and cannot be washed away easily. With the introduction of total-etch systems, in which enamel and dentin are etched simultaneously, weaker acids re applied to enamel. With this total etch concept, the term etching is often referred to as conditioning. Etchant is referred to as conditioning agent: The concentration and length of application of the conditioning agents are adapted to provide a microporous etch pattern in enamel and causing extreme demineralization of the dentinal surface. Apart from H3PO4 acid – sued in concentration ranging from 10% to 40% other inorganic acids such as nitric acid – 2.5% concentration. Organic Acids : - Citric acid - Maleic acid - Oxalic acid : 1.6% - 3.5% Recent innovations : Candiprimers / SEP which serve simultaneously as conditioner and primer. The rationale behind these acid monomer solution is the formation of continuum between tooth surface and adhesive material by simultaneous demineralization and resin penetration of enamel surface with the 10%
- 16. acidic monomers that can be polymerized in situ. The candiprimer is applied and dispersed with air and rinsing. Though acid conditioning remains the most popular method of bonding composite resin to enamel, other methods have also been tried. One such method which was tried was depositing CaSO4 crystals on the surface of enamel by treatment with a solution of polyacrylic acid and potassium sulphate. It was suggested that these crystals trapped resin to retain it mechanically. New proposed method by MAIJER and D.C. SMITH have proposed a new method of bonding that involves crystal growth of enamel surface. The system consists of treating a clean tooth surface with a 50% solution of polyacrylic acid containing sulfate ions (SO4- ions). The liberated Ca ions will react with these sulfate ions forming CaSO4. 2H2O in 1 or 2 minutes. As these crystals nucleated with in the tooth and grow outwardly in a spherulic habit, with irregular surfaces they are similar to an etched enamel with loss of tooth substrate. Lasers have been used for enamel / dentin preparation prior to the restorative material placement. Laser etching is a process of continuous vaporization and microexplosion due to vapourisation of water trapped within the hydroxyapatite matrix. In general, more material is removed by the micro explosion of entrapped water than by direct vaporization of the HA crystals. The amount of surface roughening is dependent upon the tupe and wavelength of the laser. CO2 and Nd:YAG proved most effective lasers for etching. However, studies have shown that changes in surface morphology and bond strength after laser etching are quite similar to acid etching. KCP Technique: Kinetic cavity preparation – here both enamel and dentin bombarded with aluminium oxide particles. Similar to sand blasting. References : - Critical Concepts on adhesion to Dentin. Crit Rev Oral Biol Med 1997 ; 8 (3) : 306-35. - Principles of Adhesion. Oper Dent 1992 ; Suppl.5 : 1-19. - Current Concepts in Dentin Bonding. JADA 1993 ; May 124 (5) : 26- 36. - Dentin Bonding – Past and Present. Cur Dent 1996 ; Nov-Dec. 44 (6) : 498-507. - New Trends in Dentin / enamel adhesion. JADA 2000 ; Nov.13 (Spec No.) : 250-300. BONDING TO DENTIN : The classic concepts of operative dentistry have been challenged in the last two decades by the introduction of new adhesive techniques first for enamel and then for dentin. Nevertheless, adhesion to dentin still remains difficult. Adhesive materials can interact with dentin in different ways – mechanically, chemically or both. The importance of micromechanical
- 17. bonding, similar to what occurs in enamel bonding, ahs become accepted over the last decade. Researchers now believe that dentin adhesion relies primarily on the penetration of adhesion monomers into the filigree of collagen fibres left exposed by acid etching. CHALLENGES IN DENTIN ADHESION: SUBSTRATE: Bonding to enamel is a relatively simple process with major technical requirements or difficulties. Bonding to dentin, on the other hand, presents a much greater challenge. Severe factors account for this difference between enamel and dentin bonding. Enamel is highly mineralized tissue, composed of more than 90% (by volume) hydroxyapatite. Dentin contains substantial proportion of water and organic material primarily type I collagen. Dentin contains a dense network of tubules that connect the pulp with DEJ. The tubules are lined by a cuff of hypermineralized dentin called peritubular dentin. The less mineralized intertubular dentin contains collagen fibrils with the characteristic collagen banding. The intertubular dentin is penetrated by submicron channels, which allow the passage of tubular liquid and fibres between neighboring tubules, forming intertubular anastomoses. Dentin is intrinsically hydrated tissue, penetrated by a maze of 1 to 2.5 µm diameter fluid-filled dentin tubules. Movement of fluid from the pulp to the DEJ is a result of a slight but constant pulpal pressure. Pulpal pressure has a magnitude of 25-30 mm of Hg or 34-40 mm of H2O. Dentin tubules enclose cellular extension from the odontoblasts and therefore are in direct communication with the pulp. Inside the tubule lumen, other fibrous organic structures (the lamina lamitans) can be observed, these substantially decrease the functional radius of the tubule. The relative area occupied by dentin tubules decreases with increasing distance from the pulp. The number of tubules decreases from about 4,5000/mm3 close to the pulp, to about 20,000/mm3 near the DEJ. The tubules occupy an area of only 1% of the total surface near the DEJ, whereas they compromise 22% of the surface close to the pulp. The average tubule diameter ranges from 0.63 µm at the periphery to 2.37 µm near the pulp. Adhesion can be affected by the remaining dentin thickness after tooth preparation. Bond strengths are generally les sin deep dentin that in superficial dentin. But some dentin adhesives like 4-META monomer, do not seem to be affected by dentin depth. Whenever tooth structure is prepared with a bur/other instrument residual organic and inorganic components form a ‘smear layer’ of debris on the surface. Smear layer fills the orifices of dentinal tubules (forming smear plugs) and decreases dentinal permeability by upto 86%. Composition of smear layer is basically HA and altered natural collagen. Its altered collagen may even acquire a gelatinized consistency as a result of the friction and heat created by preparation procedure.
- 18. Removal of smear layer and smear plugs with acidic solutions may result in an increase of the fluid flow onto the exposed dentin surface. This fluid may interfere with adhesion, because hydrophobic resins do not adhere to hydrophilic substrate if the resin tags are formed in the dentinal tubules. Additional factors affect dentin permeability - Use of vasoconstrictors in local anaesthetics – decreased pulpal pressure in a fluid flow in tubules. - Radius and length of tubules - Viscosity of dentin fluid - Pressure gradient - Molecular size of the substances dissolved in tubular fluid - Rate of removal of substances by the blood vessel sin pulp affect permeability. All these variables make dentinal dynamic substrate and consequently a very difficult substrate for bonding. II. Stresses at Resin – Dentin Interface : Composite shrink as they polymerize, creating stresses of upto 7 MPa within the composite mass, depending on the configuration of the preparation. When composite is bonded tone surface only, stresses within composite are relieved by flow from the unbonded surface. However stress relief within a 3-D bonded restoration is limited by its configuration factor / C-factor. Unrelieved stresses in the composite may cause internal bond disruption as well as marginal gaps around the restoration that increase microleakage. Immediate bond strengths of approximately 17 MPa may be necessary to resist the contraction stresses that develop in composite during polymerization to prevent marginal debonding. Water sorption by the resin may composite for the effect the polymerization shrinkage because resin may expand and seal off marginal gaps, but this occurs only over a relatively long period of time. Water sorption is directly proportional to the resin content. Enamel bond strengths are usually sufficient to prevent formation of marginal gaps by polymerization contraction stresses. These stresses may, however be powerful enough to cause enamel defects at margins. Extension of enamel cavosurface level may increase the enamel peripheral seal. Microleakage around dentin margins is potentiated by this discrepancy in linear coefficient of thermal expansion between the restoration and the substrate. Treatment of dentin for Optimal Bonding: The characteristics of successful bonding of a resin composite to dentin includes micromechanical attachment between resin and demineralized, primed surface layer of intertubular dentin. This complex referred to as the hybrid layer is best achieved by acidic conditioning agents which remove the smear layer, produce a surface demineralization to a depth of 3-6 µm and expose the dentinal collagen frame work. In some cases smear layer is not removed but rather dissolved or modified to include it within the bonding process. Application of hydrophilic
- 19. resin primers facilitates subsequent penetration of low viscosity adhesive resins into microporous collagen scaffold and dentinal tubules. Polymerization of this infiltrated resin stabilizes the surface hybrid layer. Meticulous application of these steps effect a gap free bond. Other areas of concern during dentinal bonding are complex histological structure and variable composition of dentin at different locations. It consists of 50% volume of in organic content, 30% of organic material, 20% of water / fluid content. The high protein content – respectively for low surface surgery of dentin (44.8 dy/au2 ), which differentiated from etched enamel. Wetting of such a low surface energy – difficult. Further H2O is an essential component of natural dentin and hence surface drying is difficult to achieve than is generally realized. The acquired environment is difficult to bond to since H2O competes effectively for all the adhesion sites. DENTAL ADHESIVE SYSTEM: The dental adhesive system consists a conditioner (etchant), primer and bonding agent (adhesive). Criterial for Ideal Dental Adhesive System (Philips and Rage) 1961 - Provide a high bond strength to dentin that should be present immediately after placement land that should be permanent. - Provide a bond strength to dentin similar to that to enamel. - Show good biocompatibility to dental tissue including pulp. - Minimize microleakage at the margins of restorations. - Prevent recurrent caries and marginal staining - Be easy to use and minimally technique sensitive - Possess good shelf life - Be compatible with a wide range of resins - System should not be toxic or sensitizing to the operators and patients. - Should seal the tooth surface from oral fluids. Etchants, Conditioners, Primers and Bonding Agents : There is confusion regarding these terms because they are often used interchangeably. Etchants: Basically implies the dissolution of the etchant and reaction substrate products are removed by rinsing. Conditioning: Involves cleaning, structural alternation and increasing adhesiveness of the substrate. Primer: That is monomer dissolved in solvents such as water, acetone, or alcohol are applied to the etched or conditioned dentin substrate but are not rinsed off. Primers are available in one bottle or two bottle version. The 2 bottle version polymerized following mixing application and solvent removal. Bonding Agent: Usually an unfilled resin that consists of a hydrophilic monomers such as BisGMA, UDMA, TEGDMA and hydrophilic monomers
- 20. such as HEMA. Some recent commercial products combined with primer and bonding agent in one bottle (Prime and Bond). Conditioner: Most commonly use din the initial stage of clinical application of total etch system and are therefore applied simultaneously to enamel and dentin. CONDITIONER OF DENTIN: Definition: Conditioning – Alteration of dentin surface including the smear layer with the objective of producing a substrate capable of micromechanical and possibly chemical bonding to a dentin adhesive. Effects: Physical Effect Chemical effect Physical: Increase / decreases the thickness and morphology of smear layer. Increase / decrease the morphology of dental tubules. Chemical: - Modifications of the fraction of organic matter. - Decalcification of inorganic portion. Performed by - Chemical - Thermal - Mechanical CHEMICAL CONDITIONING: Both acids and calcium chelators – rely on removing the smear layer are used as chemical conditioners. Acid Conditioners: Earlier acid treatment was restricted to enamel and not used on dentin with a fear of pulpal damage. But with more of research and Fusayama’s pioneering research on total etching with 37% H3PO4 – simultaneous etching is being accepted. Acid conditioning are employed with the objective of not only removing the smear layer but also simultaneously demineralizing superficial dentin of 3-7 µm to expose a microporous collagen scaffold into which therein will punctuate. On intertubular dentin, the exposed collagen fibres are often additionally covered by an amorphous layer which is of variable thickness and has microporosities which is attributed to combined effect of denaturation and collapse of residual smear layer collagen. This collagen smear layer’ may reduce the permeability of underlying dentin to resin monomers and is highly cross linked and insoluble in acids. At the tubule orifices, peritubular dentin is often completely dissolved to form a funnel shape structure and expose circularly oriented collagen fibrils which are often additional retentive sites at the tubule wall. After conditioning, maintenance of a moist dentin surface is recommended, following wet bonding technique to prevent collapse of unsupported collagen and promote wetting and infiltration of subsequently applied resin. Several acids are used for the purpose of conditioning. These
- 21. include phosphoric acid, maleic acid, citric acid, nitric acid, oxalic acid, pyruvic acid and hydrochloric acid. Among these, H3PO4 was first acid to used as the conditioner at a concentration of 37%. Recently acid concentration and etching times have been refined. A 10% solution of H3PO4 appears to provide better bond strength than the higher concentration. However, results of enamel bond strength become questionable when these lower concentration acids are used. Nitric acid is a stronger acid than the phosphoric acid. DBA (Eg. Tenure, Mirage bond) that use nitric acid conditioners are highly adhesive and provide good tubule seals. 10% citric acid continued with 3% Ferric chloride is used as smear layer remover and etchant. Another combination etchant is 10% citric acid and 20% CaCl2 (eg. Clearfil linear bond). Composite to H3PO4 etching, this combination etchant decalcifies dentin to a lesser depth, and tubules do not open into a funnel shape. Maleic acid (eg. Scotchbond) results in removal of smear layer but not smear plugs. CHELATORS: Contrary to the strong acid etchants, chelators remove the smear layer of decalcification or significant physical changes on the underlying dentin substrate. Also no funnel shaped changes are evident with the use of these agents; instead a chelate is formed. A chelate refers to a compound with a central rectal ion surrounded by covalently bonded atoms, ions or molecules called ligands which possess additional bonds for chemical reaction. The best known chelator conditioner is EDTA adjusted to a pH of 7.4. It was developed for use in Gluma system when used for 30 seconds, the smear plugs were not fully removed with this conditioner. THERMAL CONDITIONING: The recent trend to use lasers in conditioning of dentin. These may serve as a potential alternative to acids for conditioning of dentin. It is speculated that the lasers cause recrystlalization of dentin resulting in fungi form appearance that contributes to increased microrelation or possible chemical adhesion of a restorative material to the tooth structure. Further, they remove the organic elements, leaving behind an apatite substance in a new alpha form. The carbonized black spot that results after hazing is easily washed off with water. PRIMING: Primers are the 2nd step in bonding procedure are the actual adhesion promoting agents that contain monomers with hydrophilic properties, which have an affinity for the exposed collagen fibrils and hydrophobic properties for copolymerization with adhesive resin. These monomers, usually HEMA and 4-META are dissolved in solutions of acetone / ethanol.
- 22. EFFECT OF CONDITIONING: Three layers are seen. 1st Layer : Presence of an upper diffuse black layer 7 any ultrastrucural arrangement implies that, over this distance, the collagen fibrils might have been denatured by acid conditioning. Another explanation for this dark amorphous material might be that of the residual, demineralised insoluble and perhaps denatured collage from original smear layer has fallen down on the surface during etching. In a further step this denatured collagen layer was probably incorporated by the resin infiltrating the decalcified dentin surface layer creating the so called resin impregnation base. 2nd Layer : Underneath this layer closely packed collagen fibrils with small interfibrillar spaces were arranged parallel to the dentin surface presumably restricting deep resin impregnation to the interfibrillar tunnel like spaces. Induced the resin impregnation base frequently bulged out into the underlying collagen network and appeared to be confined by obstructive, parallel running collagen fibrils. Consequently the resin impregnation would primarily occur at the upper denatured collagen layer with increasing gradient of intensity to the underlying collagen fibril arrangement. The presence of an amorphous substance in the interfibrillar spaces might represent such confined resin interdiffusion into the tunnel like structure. 3rd Layer : Otherwise referred as HIATUS has fewer collagen fibers with mineral inclusion. This hiatus was observed in all polymer thickened specimens, in 90% of specimens etched with aqueous H3PO4 and 60% of specimens etched with silica thickened gels. Depth of Demineralization depends on : 1) Kind of acid 2) Application time 3) Acid concentration and pH 4) Surfactant thickness and modifiers. PRIMING AND WETTING: Uses of Primers: Promote resin promotion into the moist, demineralized dentin with the aim of achieving complete resin penetration. The dentin adhesive resin must wet the dentin if adhesion is to take place liquids wet a surface when they spread across it readily rather than remaining braded on the surface. Critical surface tension of a liquid allows a drop to spread across the surface so that its contact angle is reduced to zero. It is desirable that the adhesive liquid have a surface tension equal to or some what less than the critical surface tension for the solid substrate. Smear layer covered of dentin has critical surface tension equal to 42 dynes/cm2 but that following demineralization by EDTA has a surface tensions – 29 dynes / cm2 . 2.5% nitric acid 27 dynes /cm2
- 23. This unlike surface energy of enamel, the surface energy of dentin decreases probably due to higher concentration of collagen. When dentin required with an acidic conditioner is rinsed with water the solubilized Ca++ and PO4 ions and reaction products should be extracted from spaces between collagen fibrils. When the strategy of wet bonding is applied, the collagen fibril network is effectively suspended in water. During the priming phase resin monomers and solvents must diffuse through the long narrow spaces between fibrils to reach the bottom of the demineralized zone. The primer solvents should be either water or water inscrible. The primer monomer should be hydrophilic because they must compete with water, infact diffuse through water especially in the depth of demineralized zone. Collagen fibrils contain both bound and unbound water. If the collagen fibrils are to be enveloped by resin, the unbound water must displaced by resin monomers during bonding process. So that a layer of hydrophilic resin may coat each collagen fibrils. ADHESIVE RESIN: Also called the bonding agent - Consist primarily of o Hydrophilic monomers (BisGMA and UDMA) o Hydrophilic monomers o Viscosity regulator o Wetting agent – HEMA - Function – Major role in stabilization of hybrid layer by formation of resin tags i.e. resin extension into tubules. - Types – Auto cure – theoretically advanced because it polymerizes at the interface by body heat. Disadvantages – It is slow. o Light cure – It is polymerized prior to the application of composite resin. - In this way, the adhesive resin is not displaced and adequate light intensity is available to sufficiently cure and stabilize the resin tooth bond to counter act the polymerization shrinkage of the resin composite. - Modes of application : Spreading of adhesive resin over the surface to which it is bonded should be done preferentially by brush thinning rather than air thinning. - Adhesive should be copiously placed using a brush tip. - Adhesive resin layer thickness of 100 µm. - Blowing of adhesive resin layer may reduce its thickness too much, decreasing its elastic buffer potential. - The adhesive resin should always be used prior to application of restorative resin composite. In this way adhere resin is not displaced when the restorative resin composite is applied. - Procuring the adhesive resin will stabilize the resin tooth bond and consequently activate the elastic stress relaxation mechanism.
- 24. Functions: - A sufficiently thick layer of adhesive resin – may be due to its relatively high elasticity – acts as stress relaxation buffer (elastic bonding concept). - Polymerization content stresses generated during the placement of composite resin was found to be significantly absorbed and relieved by the application of an increased thickness of two stiffness adhesive. - It also aids in – Absorbing masticatory forces, Tooth flexure effect, thermal cycling shock. - Because oxygen inhibits resin polymerization on oxygen inhibited layer of about 15 µm will always be formed on top of adhesive resin even after light curing. This O2 inhibited layer offers sufficient double MMA bonds for copolymerization of the adhesive resin with the restorative resin. SMEAR LAYER AND ADHESIVE STRATEGIES: What is smear layer? When tooth surface is instrumented with rotary and manual instruments during cavity preparation, cutting debris is smeared over the enamel and dentinal surface forming what is termed – smear layer. Definition: Any debris, calcific in nature produced by reduction/ instrumentation of enamel and dentin or contaminant that precludes the interaction with underlying tissue. Smear layer Treatment – 2 Options : 1) Clinical asset : Acts as effective natural cavity liner that seals dentinal tubules and reduces permeability. 2) Disadvantages : Interferes with adhesion of restorative material surviving as a focus for bacteria and it should be removed. Techniques for smear layer treatment : 1) No Re at al. The smear layer is left place of modification and the DBA indirectly applied to it. Eg. Scotchbond and Prisma bond. Resin would infiltrate there the entire thickness of the smear layer and even bond to underlying matrix or penetrate into tubules. 2) Dissolution of smear layer : Dissolved smear layer plays an vital role in chemical attachment of DBA to dentin. Eg. Scotchbond and Mirage. 3) Removal of smear layer by acid etching : Acid etching agents are used to remove smear layer and develops attachment directly to intact dentin (then primer) 4) Modification of smear layer : This allows interaction of DBA with the smear layer and improves the attachment of smear layer to dentin. Eg. Bonding agent – Prisma 2, XR Bond, All Bond. 5) Removal and replacement of smear layer : Removal of smear layer by acid etching and replacement with another mediating agent. Tenure
- 25. replaces smear layer with oxalate crystals which are deposited in dentinal tubules. MARBIDIZATION: Hybridization / formation of a hybrid layer, occurs following an initial demineralization of the dentinal surface with an acidic conditioner, exposing a collagen fibril network with interfibrillar microporosities that subsequently become interdiffused with low viscosity monomers. This zone in which resin of the adhesive system micro mechanically interlocks with dentinal collagen – is termed as hybrid layer / hybrid zone. Three Layers of hybrid Layer : 1st Layer – Top most – Amorphous electron – dense phase – which can be attributed to denatured collagen – Clearfil. Optibond and Super Bond D-liner : More loosely arranged collagen fibrils and individual collagen fibrils are directed towards adhesive resin and the interfibrillar spaces filled with resins. Scotch bond multipurpose and single bond – hybrid layer is covered by an amorphous phase, which may have originated in a chemical reaction of polyalkenoic cid copolymer of the primer with residual calcium. Middle Layer of Hybrid Layer: Contains c/s and longitudinally sectioned collagen fibrils separated by electronucleant spaces. These interfibrillar channels which have typical dimensions of 10-20 nm, represent the reason wherein HA crystals had been deposited and have been replaced by resin as a result of the hybridization process. Residual mineral crystals are sometimes scattered between collagen fibrils. Base of Hybrid Layer : Char. By gradual transition to the unaltered dentin, with a partially demineralized zone of dentin containing HA crystals enveloped by the resin or by a more abrupt transition. RESIN TAG FORMATION: The contribution of resin tag formation for bond strength has been a matter of speculation. Bond strength values droop in deeper dentin where the number of size of dentinal tubules is greater and intertubular occupies less of total bonding area. This indicates that presence of intertubular dentin is more important than the development resin tags in the bonding process. MECHANISM OF DENTIN BONDING: Composite resins do not show an intimate microscopic contact with dentin when placed directly into the cavity. To overcome this, an intervening layer of fluid is used, which fills in the microscopic space, polymerizes and combines with the composite resin and components of dentin. The basic chemical composition of these dentin bonding adhesives can be conceived as ; M-R-X CH3
- 26. M – Methacrylate group CH2 = C R – Spacer CO – O –R – X X – Reactive group capable of bonding to dentin surface The bonding mechanisms for all the three are presented in Figure 16.11 (Sikri Pg.358). Agents that use a phosphate group in their group in their bonding to calcium ions are referred to as phosphate bonding systems and are most the common ones employed. The constituent ‘Z’ in the phosphate based adhesives may be chlorine, a hydroxyl or a phenyl group. BONDING OF THE ORGANIC PORTION OF DENTIN: Bonding to the organic part of dentin involves interaction with the amino (-NH), amido (-CONH2), hydroxyl (-OH) or carboxylate (-COOH) groups present in the collagen of dentin. Removal of hydrogen from any of these groups allows combination with chemicals present in DBA. Compounds that have a capacity to react with one or more groups of collagen are isocyanates, carboxylic acid chlorides, carboxylic acid anhydrides and aldehydes. Eg. Adhesives that rely on bonding to org. Part of dentin Dentin atheist (Isocyanate based) gluma (Aldehyde based) ROLE OF WATER IN BONDING PROCESS: When prepared dentin is acid etched, the smear layer and plugs are removed and the underlying 2-7 µm layer of dentin is demineralized. Solutions used for etching are generally acidic and contain H2O to ionize the acids and dissolve and extracted minerals. Post-etching rinsing with water removes this dissolved mineral and leaves a demineralized dentins surface covered with water. About 70% of the demineralized dentin is occupied with water in areas from where the mineral has been removed. Functions of Water: It is responsible for maintaining the collagen in an expanded state and thereby preserving the spaces needed for infiltration of resin. IT acts as plasticizer for collagen and keeps in soft state. If its dehydrated : Dentin is dried/ exposed to air. Water evaporates leaves collagen in a collapsed stiffened state because of surface tension forces. So this reduces the ability of the subsequently applied agents to penetrate the collagen web. Also when collagen fibrils are brought closer, 2o forces start becoming active between adjacent peptide chains in the collagen triple helix, which is not possible when water is present – thereby increasing the stiffness or modulus of elasticity for collagen. REWETTING: - Upon addition of water, the collagen net work re-expands to about 100% of its original volume.
- 27. - It is believed that critical water concentration exists that prevents collapse of the network or allow reexpansion of dried dentin over a period of 10-30 seconds. Non Aqueous Primers: When such primers are applied to dry dentin, the collagen is not rewetted by H2O network continues to exist in a collapsed stiffened state with little / no resin penetration because of reduced porosity around collagen fibrils. Water Based Primers : When such primers are applied to air dried, shrunken and demineralized dentin – 2 events occur depending upon the concentration of primers. a) If the H2O concentration of pumice is low – H2O soluble resin monomer and/or organic solvent will stiffen the collagen meshwork faster than water can plasticize the collagen and it will not completely re-expand. CLASSIFICATION OF DENTIN BONDING AGENT: I. By Deggrange / Jean Roulet Type 1: Those that bond directly to smear layer and the sue of an acidic primer. Type 2: those that use acidic primer to alter the smear layer prior to or during bonding subdivided to a) Which are 3 separate identifiable components – essentially consisting of asepexate primer, coupling agent and unfilled resin. b) Those that have a reduced number of components i.e. usually 2. i. Or the coupling agent and unfilled resin. ii. Or the coupling agent and unfilled resin. Eg. Scotch Bond 2 Combines primer and coupling agent SEP. Here conditioner – Primer Primer Coupling agent c) When the H2O content of primer is large enough to plasticize the collagen faster than the resin / solvent stiffens it, the hydrophilic resin monomers infiltrate the network as it is gradually expanding. Excessive H2O in primer should be avoided as it dilutes the monomer concentration drastically. Dry Bonding Wet Bonding Over Wetting Bonding Technique Dry ↓ Collapse of collagen ↓ Lesser space available for resin infiltration Moist ↓ Collagen maintained ↓ Optimal hybrid layer Over wet ↓ Swelling of collagen ↓ Lesser space available for resin penetration
- 28. CLASSIFICATION OF DBA – BASED ON CHRONOLOGICAL ORDER: I. First Generation Adhesives : Initiating his enamel acid – etching technique, Buonocore et al in 1956 reported that glycerophosphoric acid dimethacrylate (GPDM) could bonding to HCl acid etched dentinal surfaces. The bond strength attained was only 2-3 MPa. After failures of this early dentin acid etching technique, research efforts fraussed primarily on developing chemical adhesion to dentin. DBA’s were no longer unfilled resins composited which intended purely to enhance wetting of the dentinal surface. The became big functional organic monomers with specific reactive groups that were claimed to react chemically with inorganic Calcium-HA and/or organic collagen components of dentin. The traditional concept of chemical adhesive potential base don bifunctional molecule. With a methacrylate group M Linked to reactive group – X By an intermediary group – R Development of N-phenyl glycine glycidyl methacrylate (NPG-GMA) was the basis of first commercially available DBA – Cervident (SS White). This NPG GMA – acted as primer and adhesion promote between enamel / dentin and resin materials by chelating with surface dentin. Since Ca+ +, ions of the tooth substructure area mediator in the bound formation, agents of this type a expected to form stronger bonds to enamel than to dentin. II. Second Generation DBA: Developed for clinical use in early 1980. These products were base don phosphorous esters of methacrylate derivatives such as BisGMA or HEA. Bonding mechanism involved enhanced surface wetting and ionic interaction between negatively charged phosphate groups and (+)vely charged calcium. The primary chemical adhesion is not thought to play a major site in the bonding process. Clearfil (Kuraray, Japan) – 1st agent in this series - composed of ethyl alcohol solution content, tertiary amine as the activator catalyst liquid – BisGMA monomer containing phosphate ester, benzyl peroxide. Bond is by attraction between (-)ve changes of O2 on the phosphorous group and (+)ve charged calcium ions in dentins surface. Drawbacks in First and Second Generations: - Lack of adequate bond strength that could over come contraction stresses during stresses. - Being hydrophobic nature – close adaptation to the hydrophilic dentin could not be dentin. III. Third Generation Dentin Bonding agent: Basis for 3rd generation of dentin adhesives was laid by Japnese philosophy of etching dentin to remove the smear layer gained acceptance.
- 29. 3rd generation adhesives unlike the 2nd generation ones either modify or completely remove the smear layer to allow resin penetration into underlying dentin before the application of the actual adhesive. The postulated bonding mechanism of the dentin – etching technique was that etched dentin would provide micromechanical retention for the restorative resin composite by allowing penetration of the resin bonding agent into the opened dentinal tubules. The extra step comprised of conditioning and primary of dentin but made the procedure more complicated and time consuming. The three steps – conditioning, priming and application of bonding agent – may be done either separately or the components combined to reduce it to two steps. Dentin conditioner is an acidic solution that removes the smear layer and is rinsed off water application. The primer solution usually contains an adhesion promotes in a solvent such as water, ethanol or acetone. These are applied to the surface and dried, presumably leaving the adhesion promotes on the dentin with its hydrophobic groups exposed to create a favourable surface for the bonding agent. In some systems, the conditioner and primer may be combined to form the “self etching primer”. First system of third generation – oxalate bonding system/ FNP system – Initial system utilized a solution of acidic ferric oxalate. IV. FOURTH GENERATION ADHESIVES: Till now, the strategies for dentin adhesion were based upon the formation of resin tags penetrating into tubules of conditioned dentin formation of precipitate on pre treated dentins surface followed by chemical and mechanical bonding to resin and chemical union to either inorganic / organic components of dentin. Recent concept by Nakabayashi (1991). Classification – Sikri : Based on Mode of application. a. In which adhesives modify the smear layer and incorporate into the bonding process. b. In which adhesives completely remove smear layer and are subdivided into 2/3 step application. 2 step – conditioning + (Primer and adhesive) 3 step – conditioning + Priming + adhesive application. Action of these agent principally based on combined effect of hybridization and resin top formation. c. In which the adhesives dissolve the smear layer rather than remove it – 2 steps. 1st step – Combined conditioner and primer (SEP) 2nd Step – Application of adhesive Principal : Partially demineralize the smear layer and underlying dentin surface with removing dissolved smear layer remnants and unplugging the tubule orifices – Rationale – demineralize dentin simultaneously penetrate with monomers and polymerize in situ.
- 30. IV. Classification of Dentin Bonding Agent – based on mode of action I. Those that bond with calcium ion (Base don phosphate esters of BisGMA) Eg. Scotchbond 1 and Bondlite. II. Those that bond with amine / hydroxyl group (Based on isocyanate / aldehyde) Eg. Gluma. III. Those that bond with repreciptiated smear layers. Eg. Scotchbond 2 and Tenure. Clinical Factors in Dentin Bonding: 1. Isolation 2. Bond to enamel 3. Roughen sclerotic dentin 4. Use mechanical retention 5. Have dentin moist after etching 6. Apply and dry primers correctly 7. Do not over thin bonding resin 8. Use flexible restorative system 9. Fill incrementally 10.Delay finishing 11.Rebound Margins 12.Follow mean directions BONDING IN OTHER CLINICAL SITUATIONS: Spectrum of bonding is quite wide. Almost every material and technique has tried to achieve bonding between two variables. Bonding spectrum in dentistry : Enamel (Etch) Silane (Etch) Metal GIC Etch Composite Resin Etch Dentin bonding Ceramic Agent Dentin BONDING OF GLASS IONOMER TO HARD TISSUE: - Can adhere to enamel and dentin - Also can bond to reactive polor substrate- base metals
- 31. - Primary mechanism of bonding – chemical mainly micro mechanical also. BONDING OF COMPOSITE TO GIC – MECHANICAL GIC commonly sued under composite as a dentin substitute – sandwich technique / bilayered technique. - 37% H3PO4 used etch enamel and GIC - Acid treatment – improves bond to composted by producing rough surface in which glass particle stand out of matrix. - Thin liquid (low viscosity) resin applied is able to penetrate into micropores between particles – thereby providing mechanical interlocking. - Cement should be fully set before etching. - Normally 20 minutes second but for fast set – 2-3 minutes, slow set for an hour / so. Light cure no need for etching. - Etching period 15-30 second. - Above 30 seconds prone to degradation by acid. - Higher the strength of cement better clinical results. - Few authors suggests layer of varnish over GIC with the rationale that polyshrinkage of composite will not disturb underlying cement. III. Bonding of Composite to Porcelain Partly – Mechanical interlocking Partly – Chemical union Mechanical Retention: Etching the surface of porcelain with HF acid / grit blasted with aluminia – increase surface roughness. Time for etching depends – Etchant concentration and type of porcelain used. To improve mechanical bonding – gap between bonding medium and porcelain minimized using low viscosity resin which penetrates into pores by capillary action. Chemical Union: By rinsing etched surface with silane coupling agent. Mechanical interlock is more important than chemical adhesion. Silane coupling agents - shown to reduce gap between porcelain and compressive presumably – improving upon wettability and hence promoting mechanical interlocking. IV. Bonding of Amalgam to Resin - Relating new treatment modality and made bonding between amalgam and tooth structure, amalgam and amalgam, amalgam and metal – successful possibility. - Advantages – Increases retention and increases fracture resistance. - Reduces microleakage - Decreases chances of recurrent caries
- 32. Agents: - All Bond - Linear Bond -2 - Amalgam Bond and - Panavia - They have dual characteristic – Hydrophilic, so that it wets the hydrophilic enamel and hydrophobic – amalgam which is hyophobic. - 4-META, MDP – used comonomers. - Bond – Between resin and amalgam – micromechanical as amalgam interlocks with fluid resin during condensation. SUCCESS AND FAILURES OF ADHESIVES: 1) Material factors - Like hydrophobic bonding agents - Incomplete resin penetration - No significant hybrid layer 2) Substrate – As said before 3) Size and shape of lesion 4) Maxillary vs mandibular arch because of – less chances of contamination and – Lower tooth flexural effects in upper jaws. 5) Patients age : Increased age – dentin sclerosed – Decreased clonal adhesiveness, increased tooth flexure. 6) Tooth flexure : Influencing factor on retention. Adhesives especially at cervical restoration. Heavy centric occlusal and eccentric forces respectively for general compressive and tensile force s- cervical area – gradually dislodge and debond the resin restoration. So compressive with adequate elastic capacity like micro filled are preferred in rich lesion. 7) Dentinal wetness : Bonding agents with effective wetting capacity ensure successful bonding. 8) Elastic bonding concept : Due to shrinkage during polymerization – Debonding can occur. - So intervening adhesive resin – sufficiently elastic to absorb the poly stress. - Can be achieved by using – relation thick layer of separately polymerized unfilled / semi filled resins.
