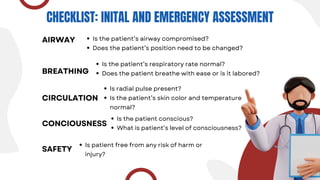
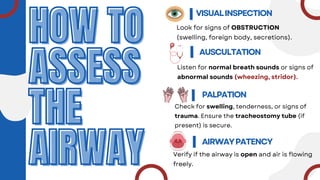
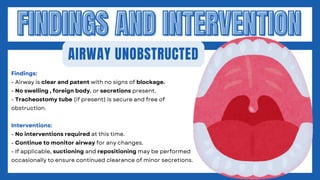
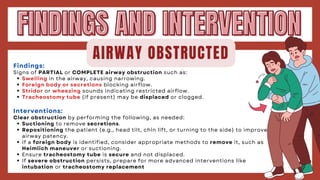
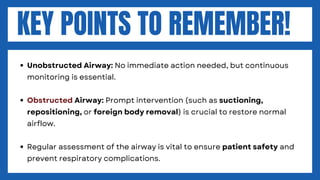
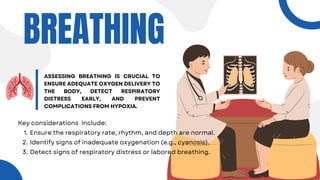
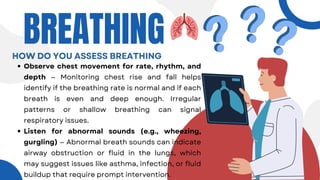
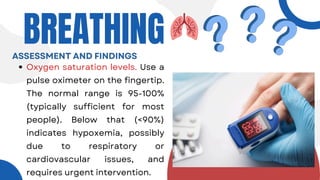
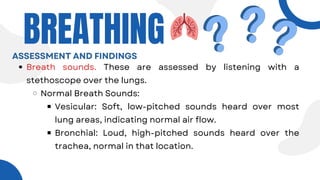
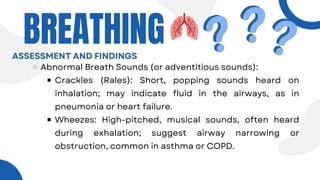
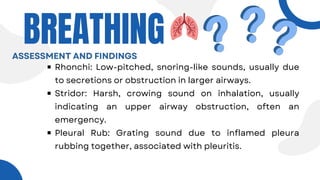
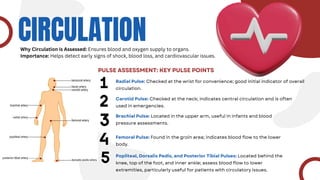
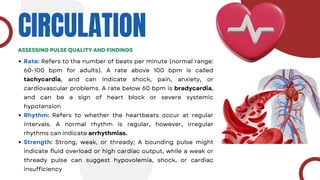
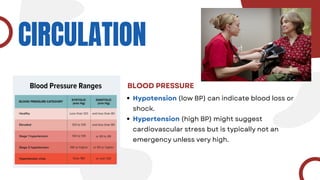
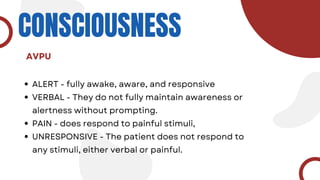
The document discusses the ABCCS framework, which emphasizes airway, breathing, circulation, consciousness, and safety in patient assessment and emergency care. It outlines assessment techniques and interventions needed to ensure patient safety and effective monitoring of vital functions. The importance of a systematic approach in nursing practice is highlighted for swift and effective response to emergencies.