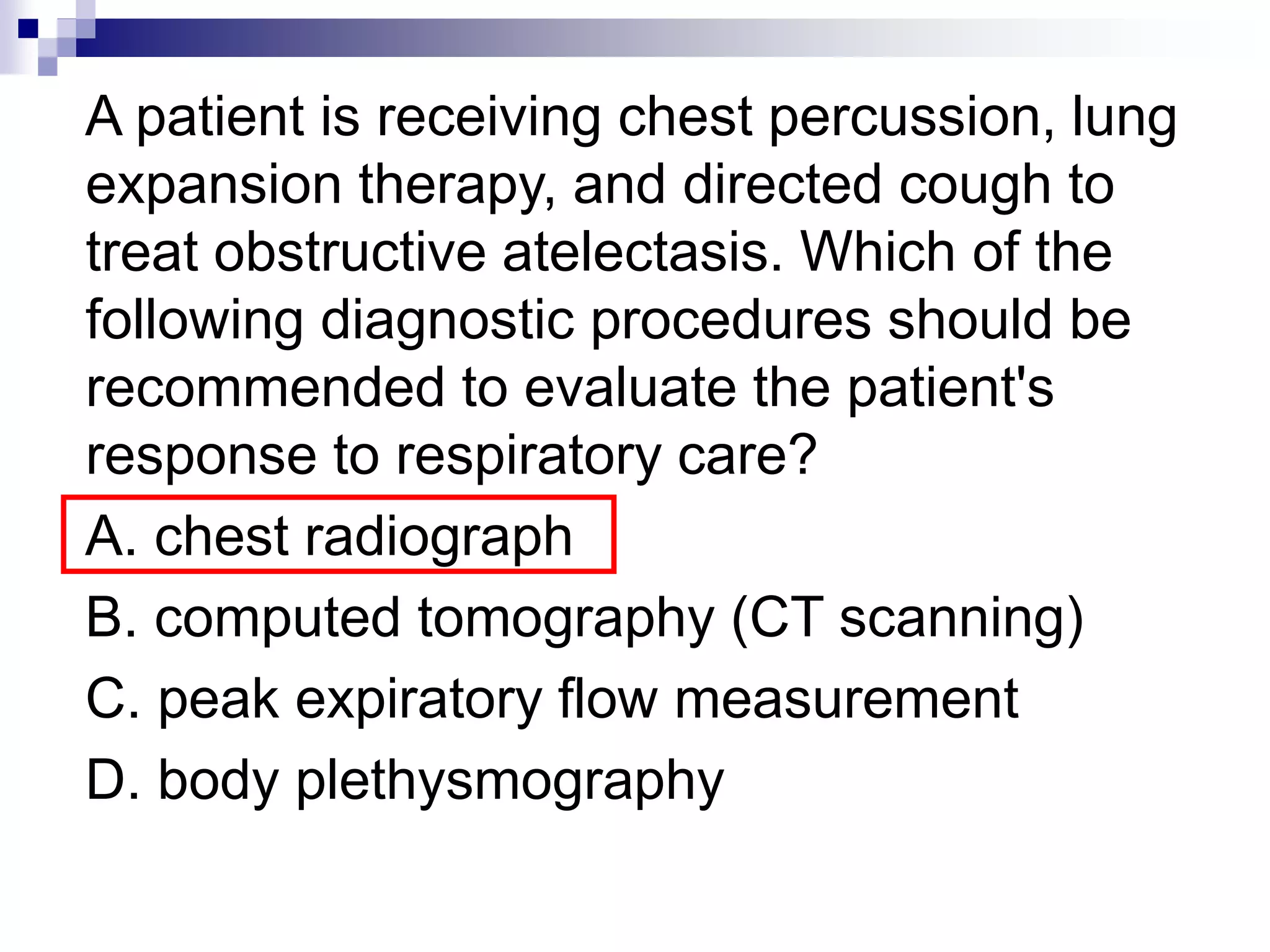
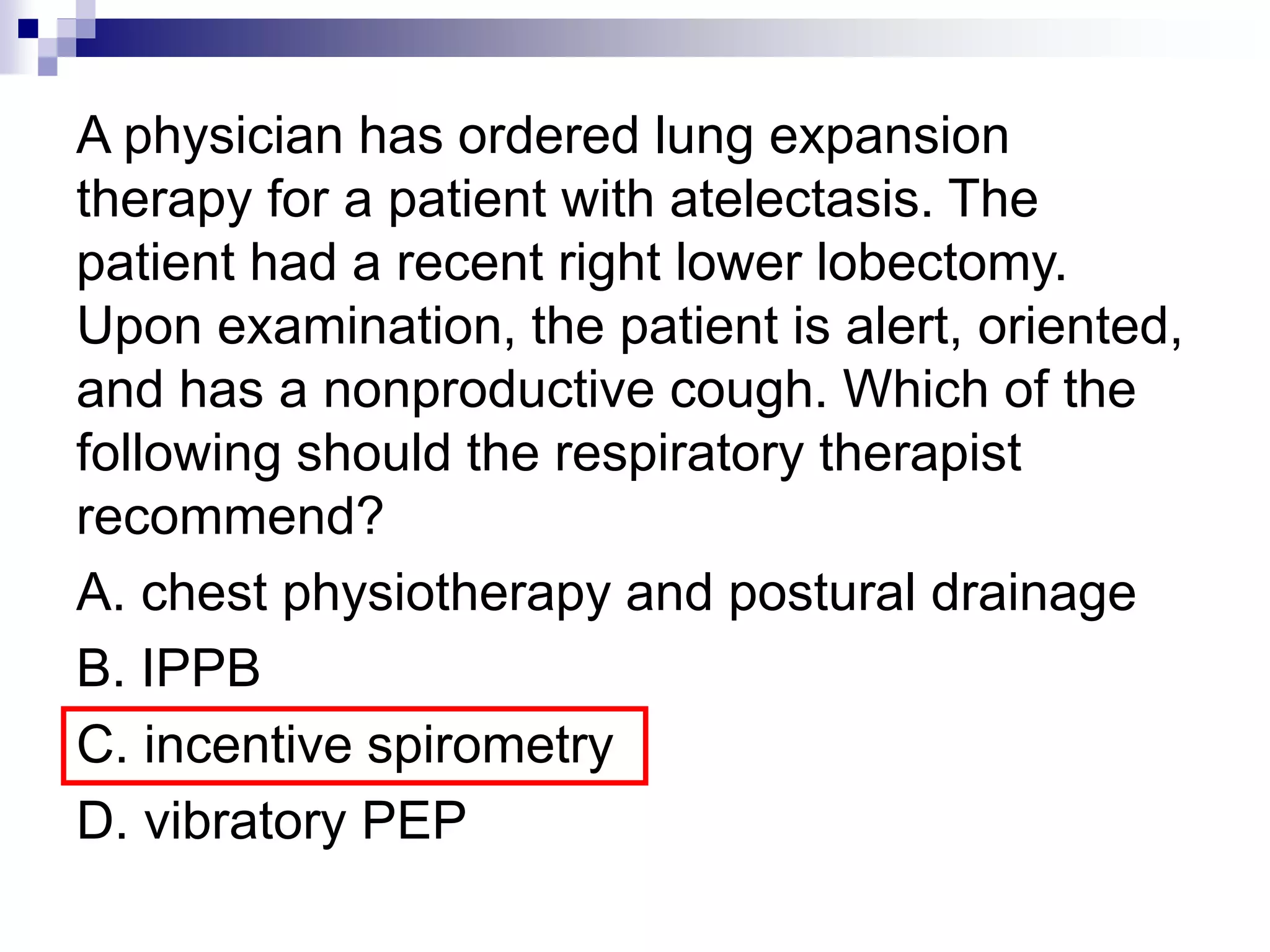
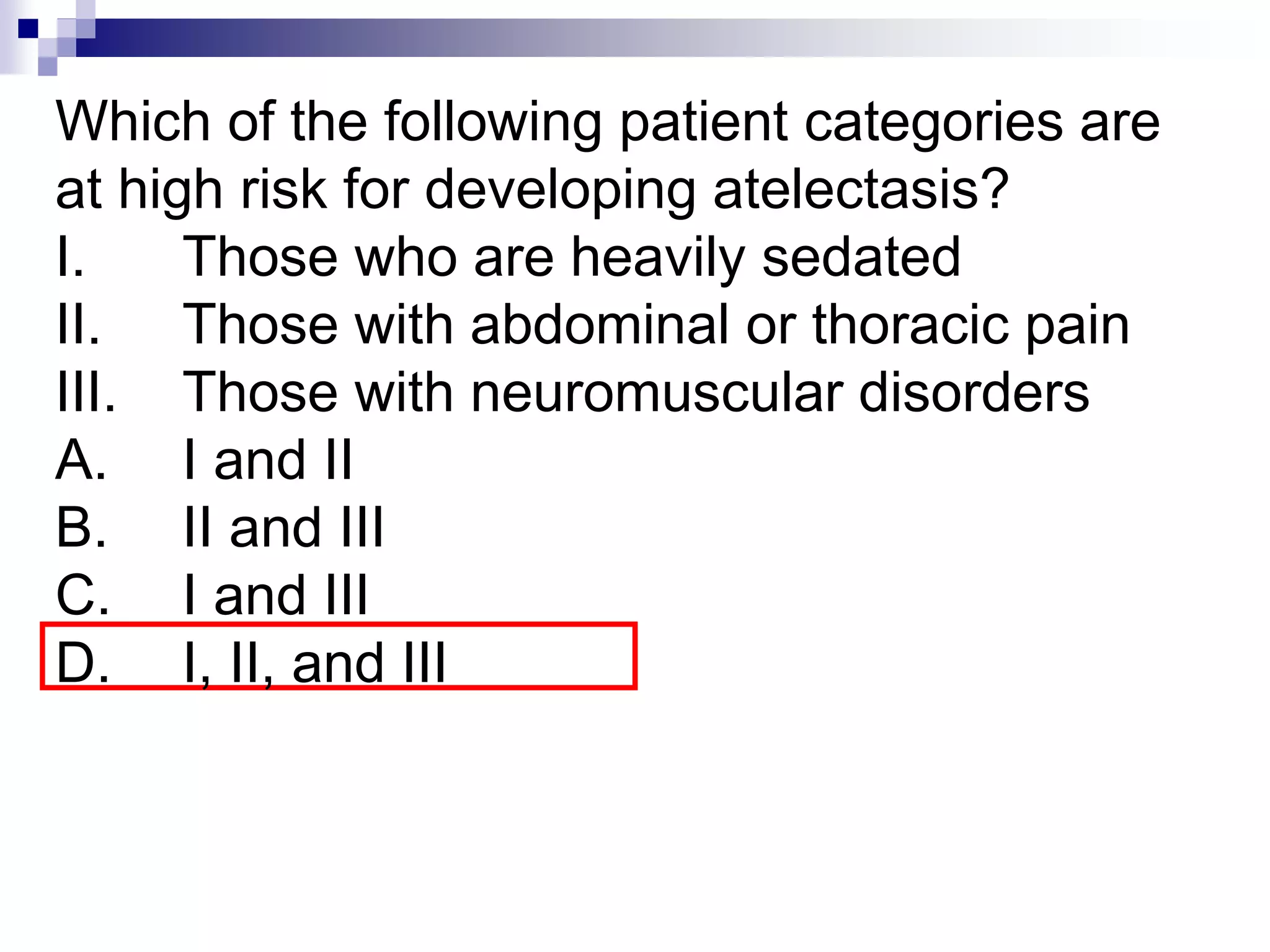
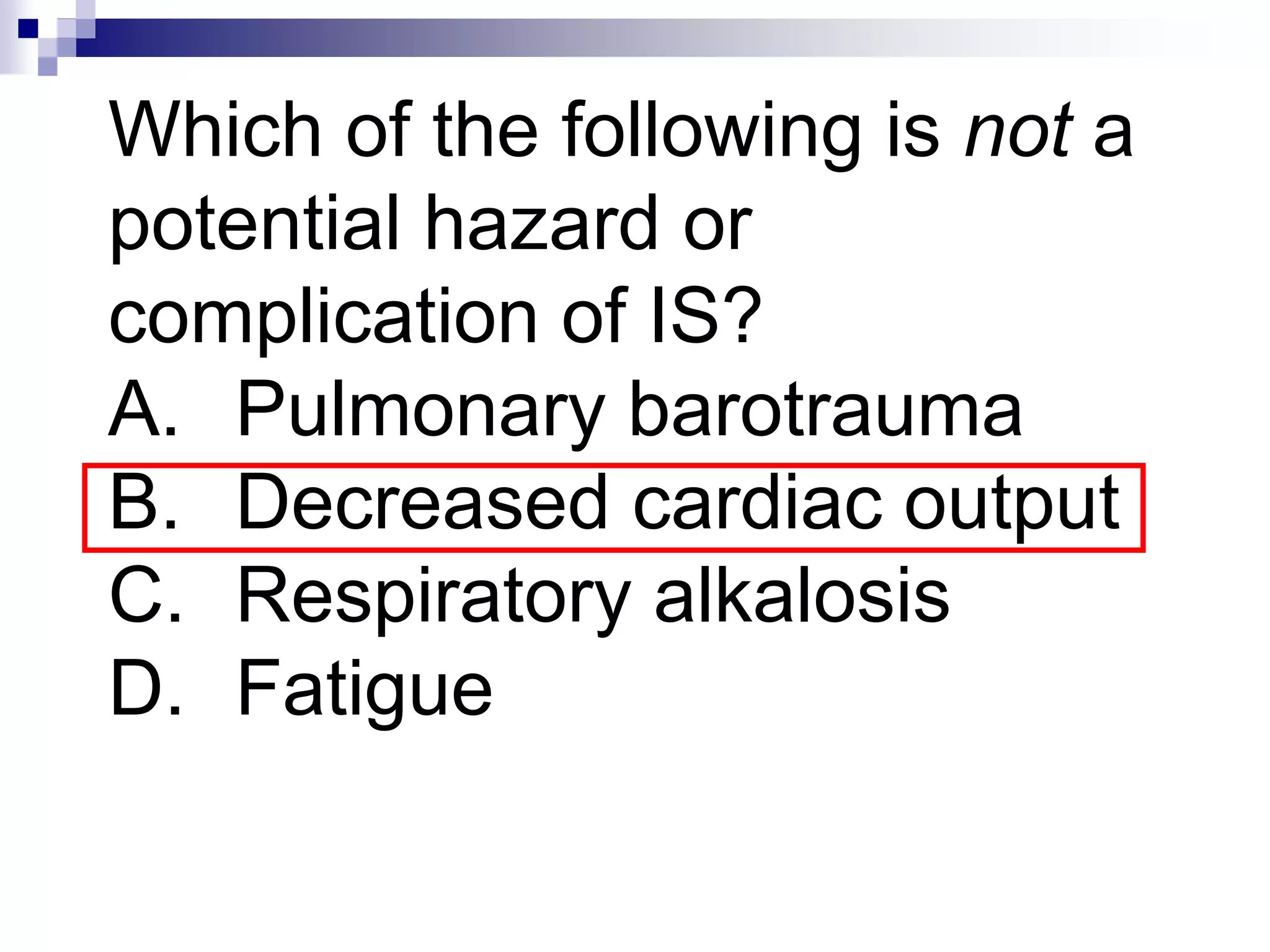
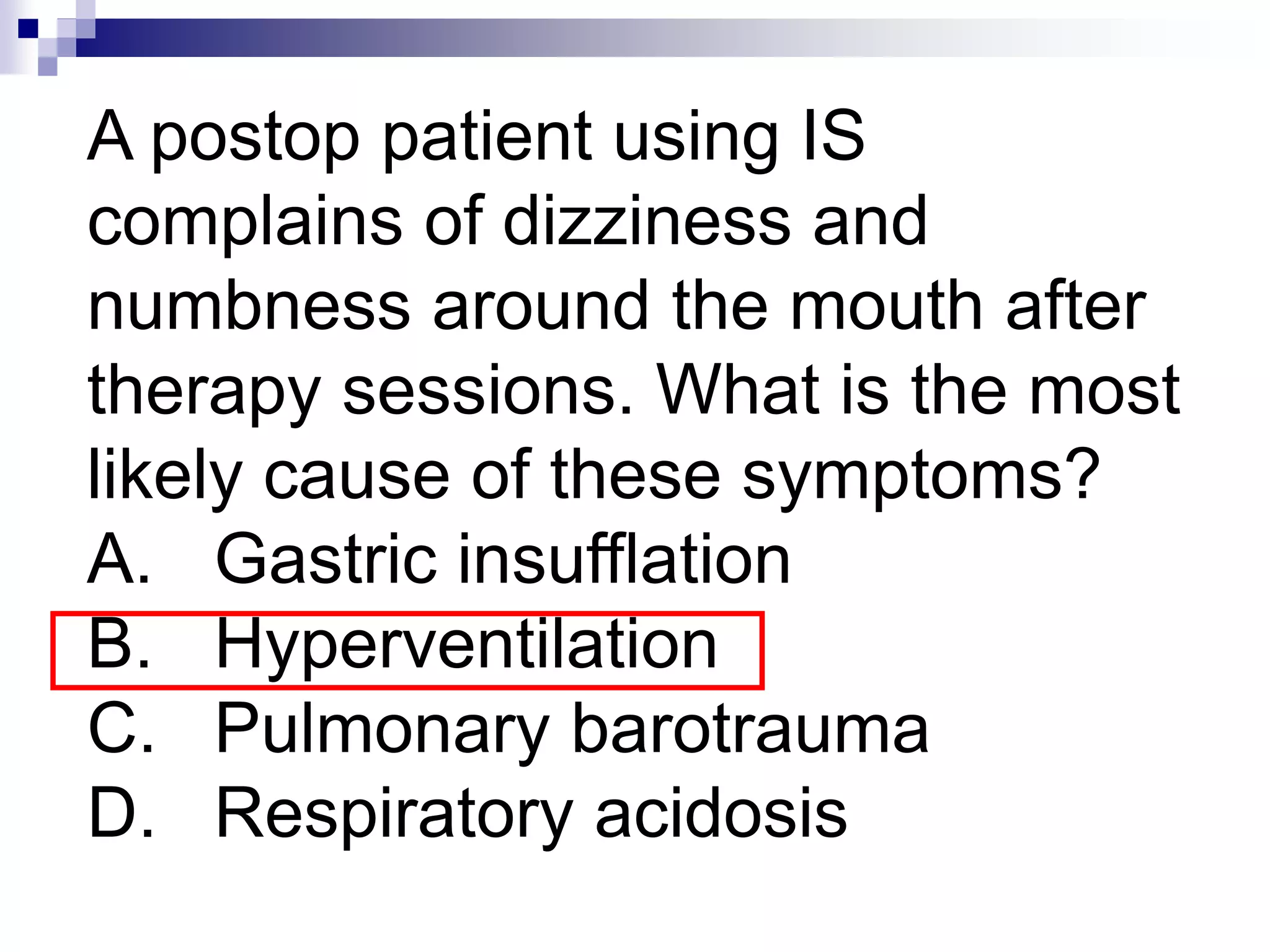
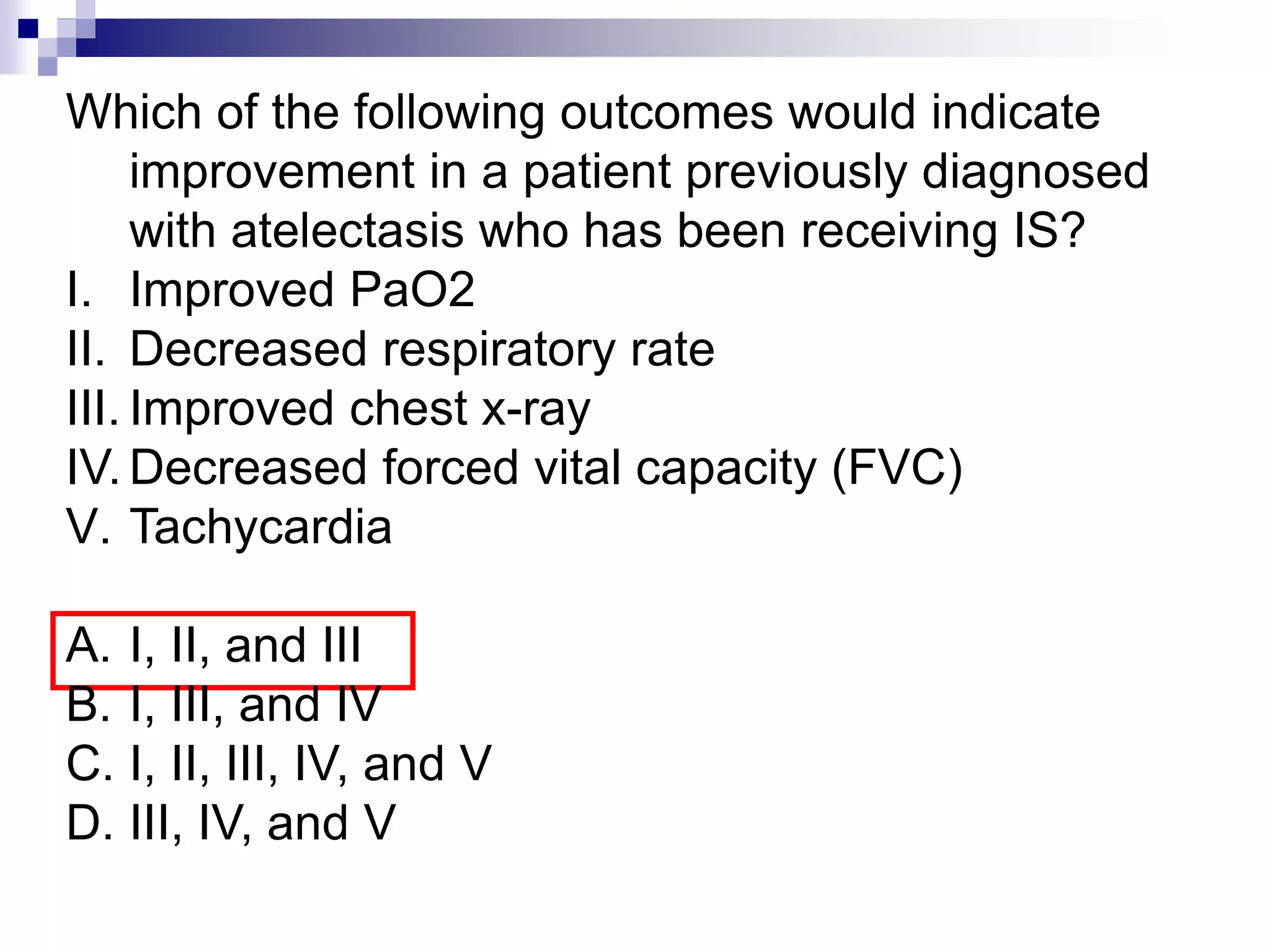
The document discusses various respiratory therapies including incentive spirometry (IS), intermittent positive pressure breathing (IPPB), and continuous positive airway pressure (CPAP). It provides information on settings, indications, contraindications, and potential complications or outcomes of these therapies. It also addresses techniques to prevent atelectasis and factors that can lead to atelectasis.