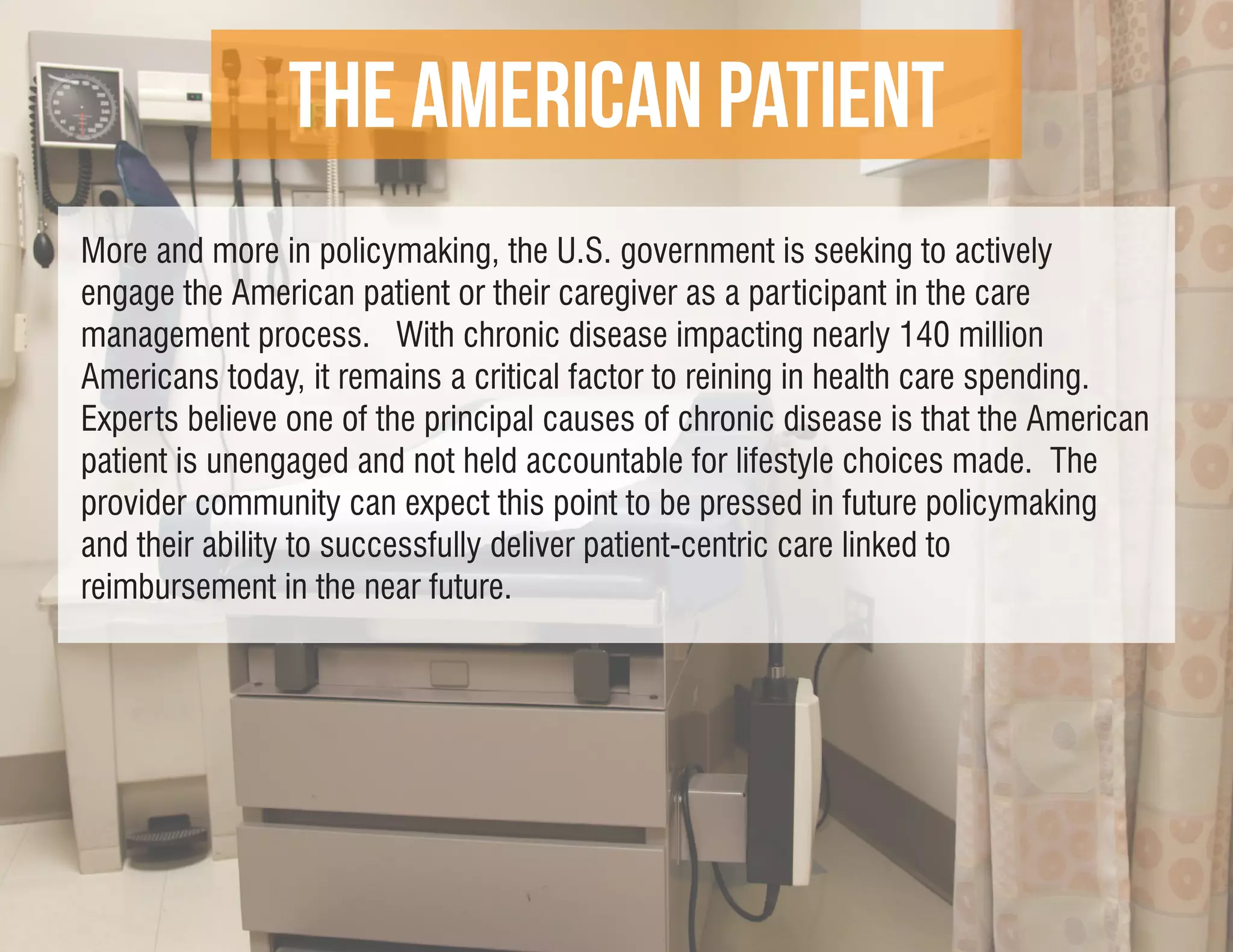
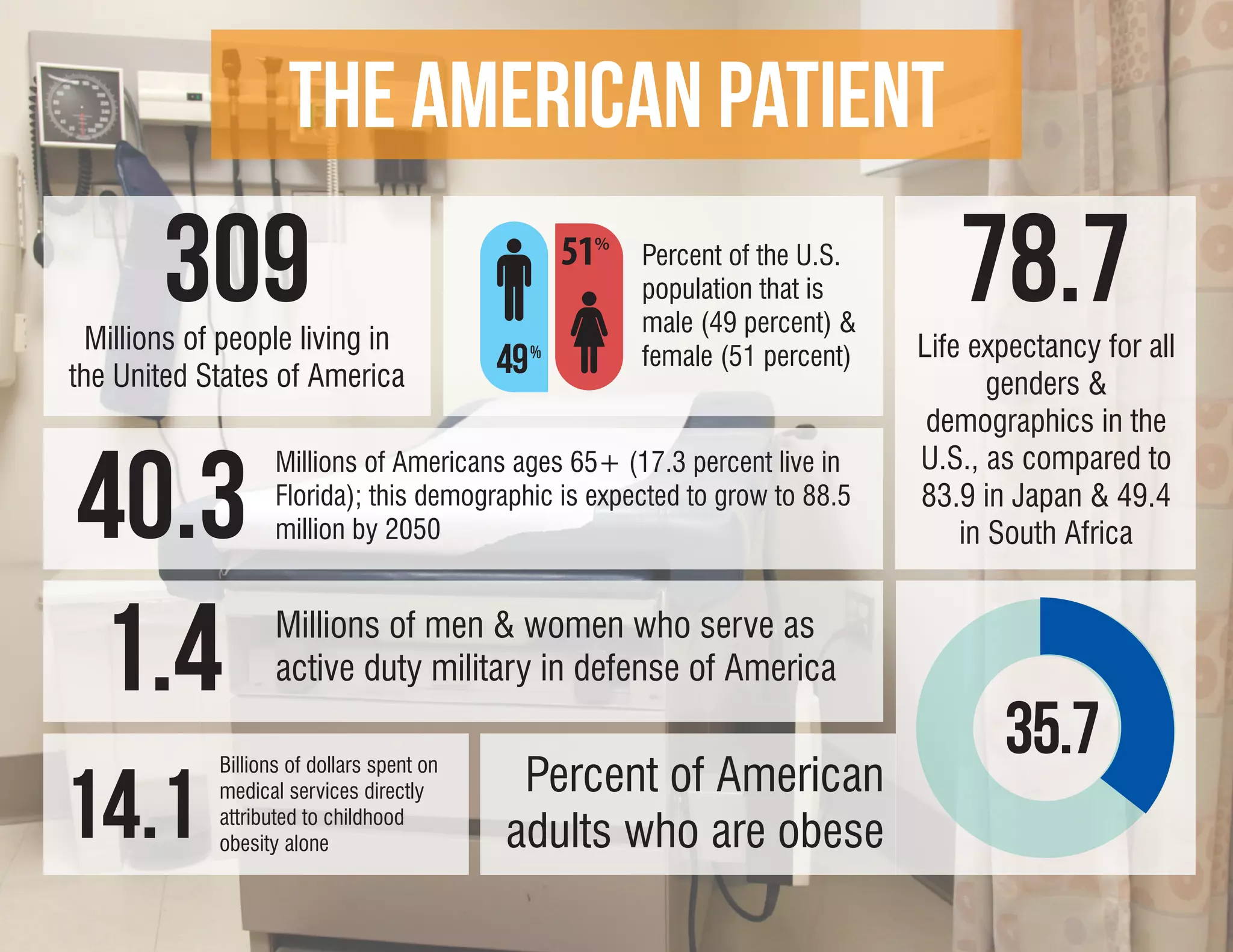
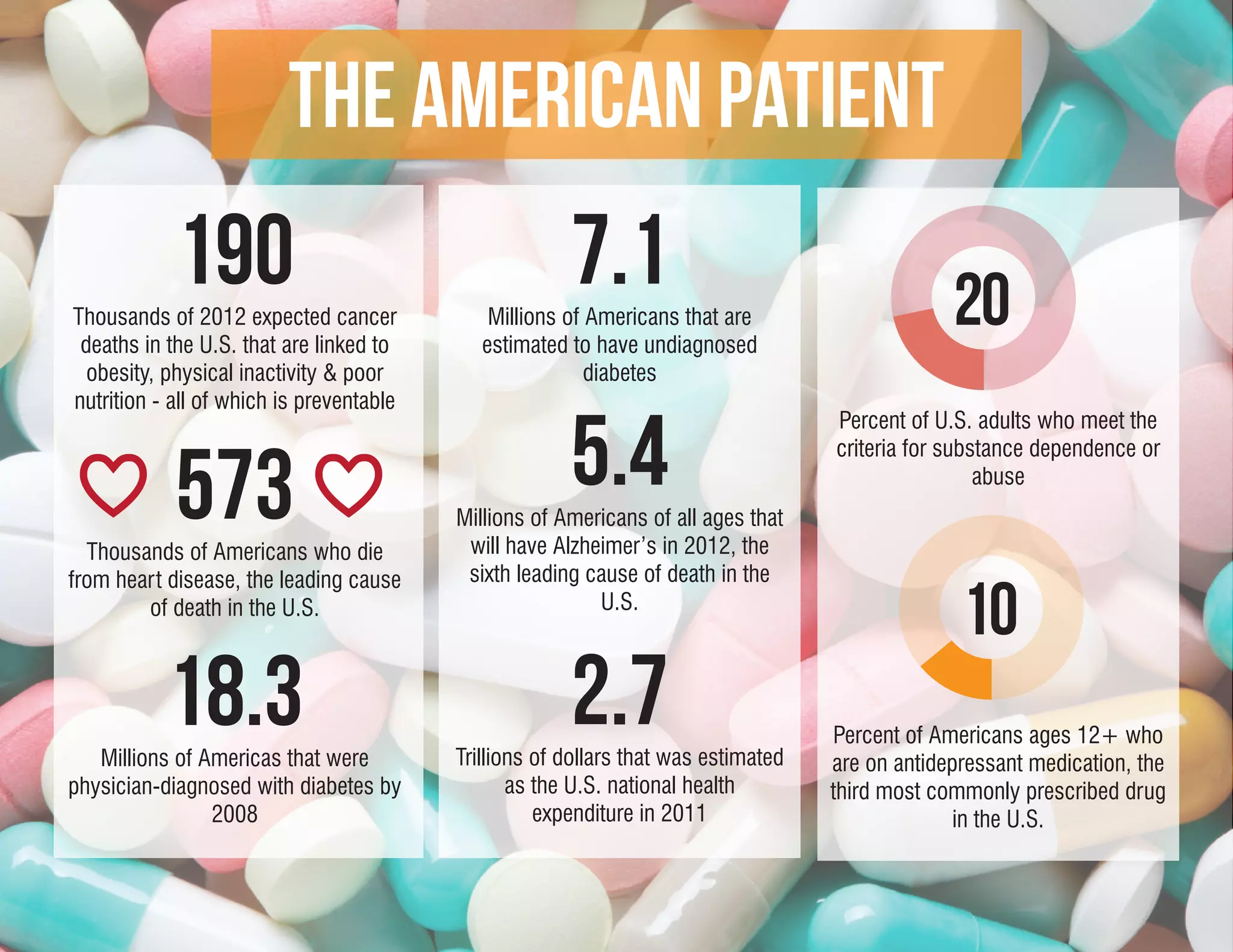
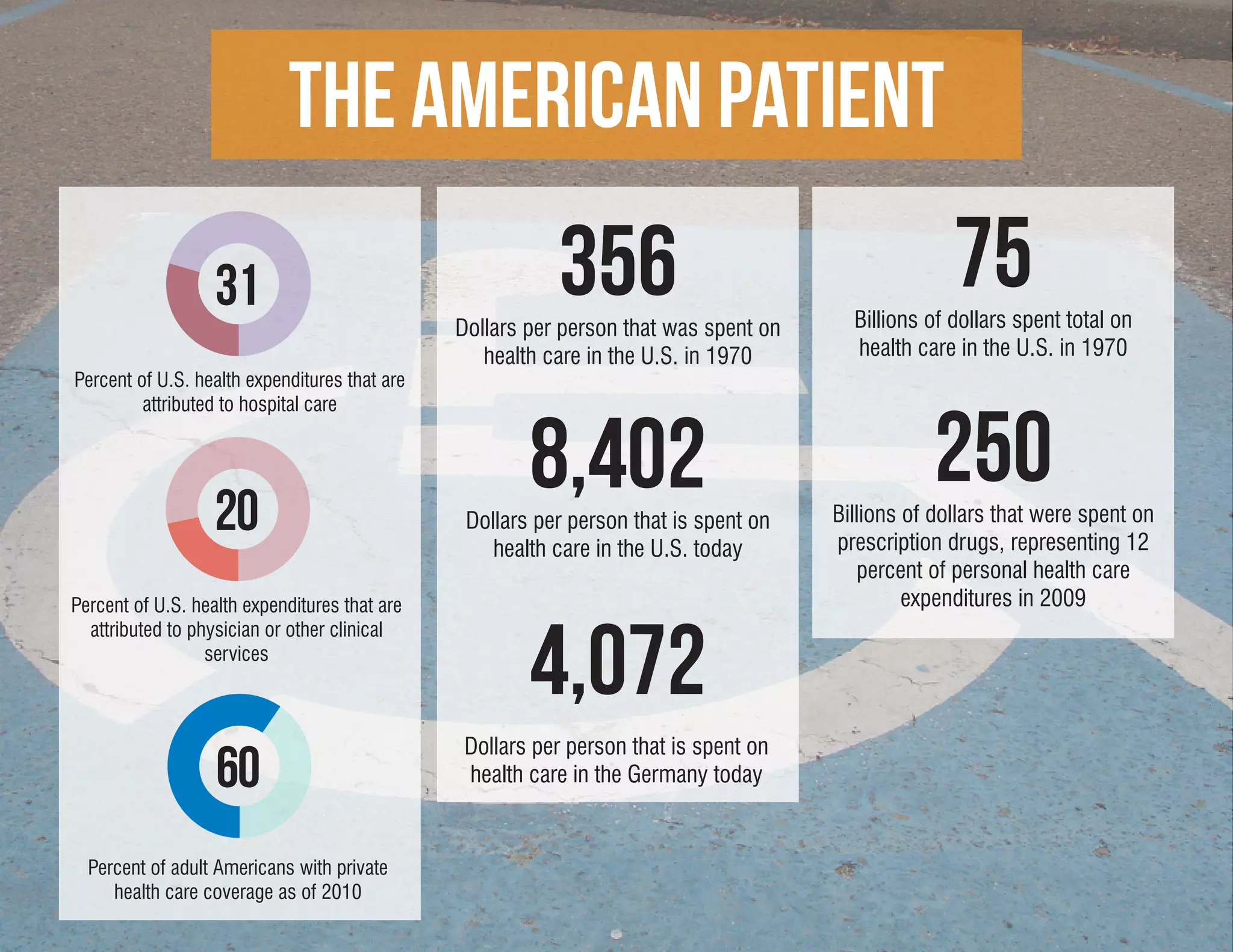
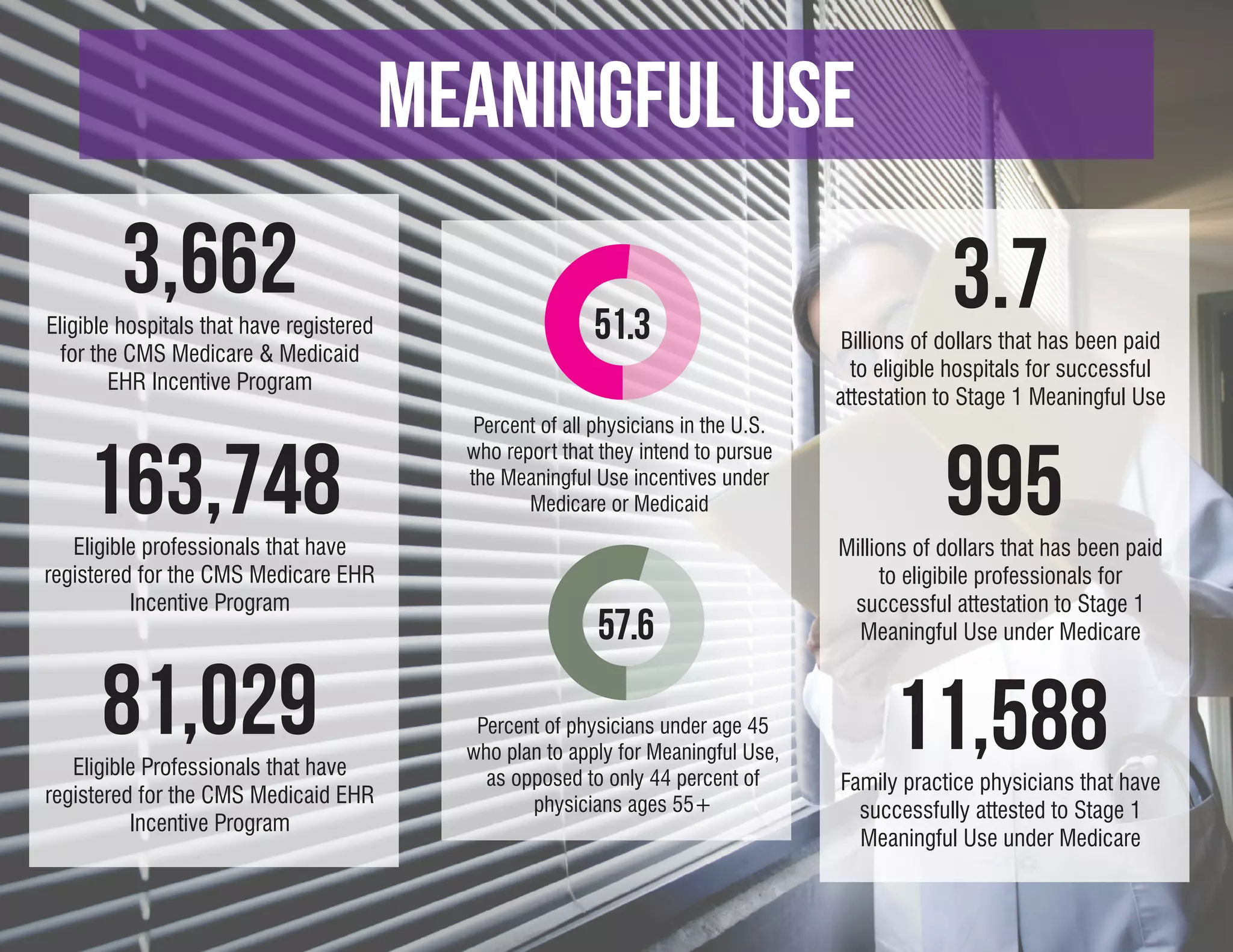
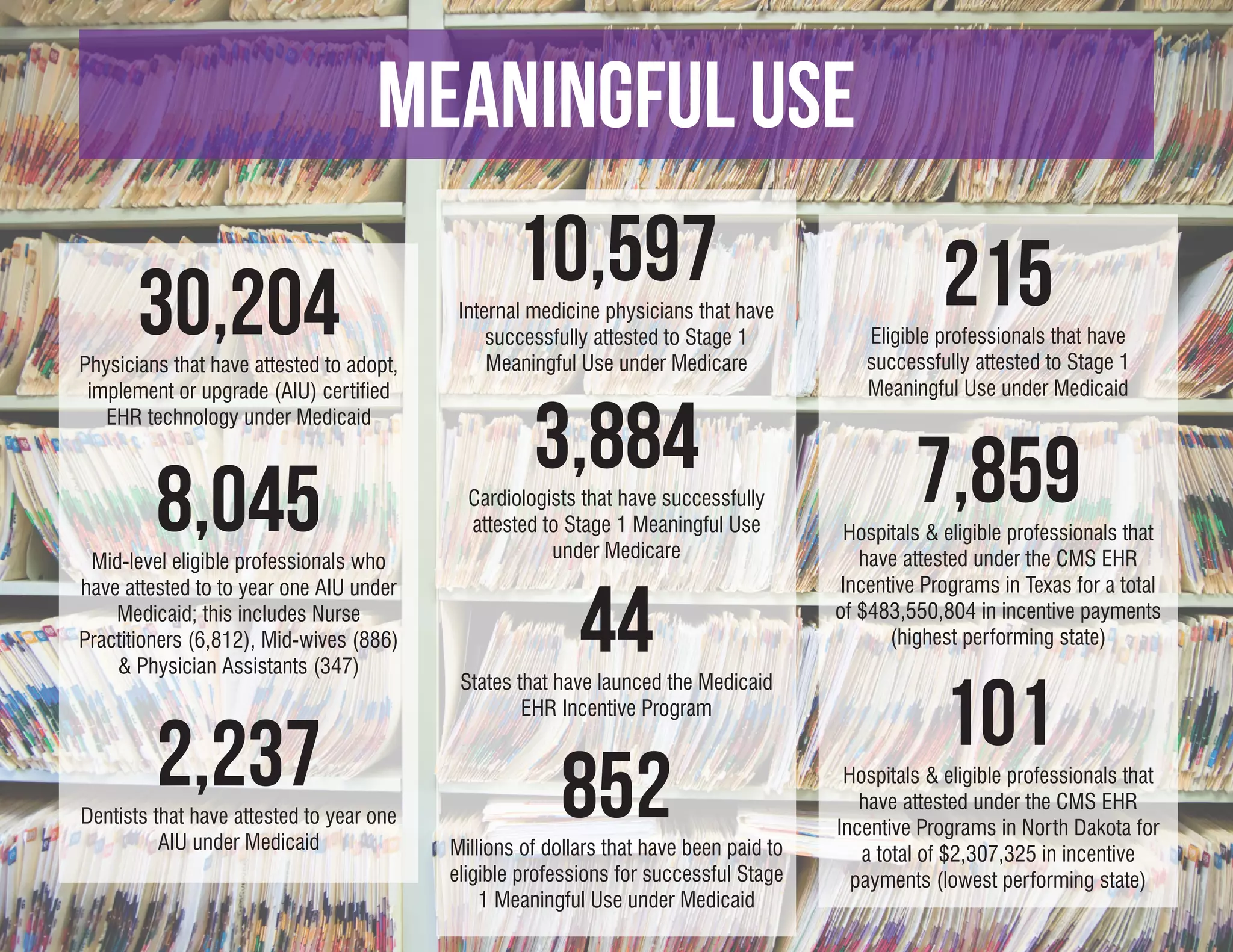
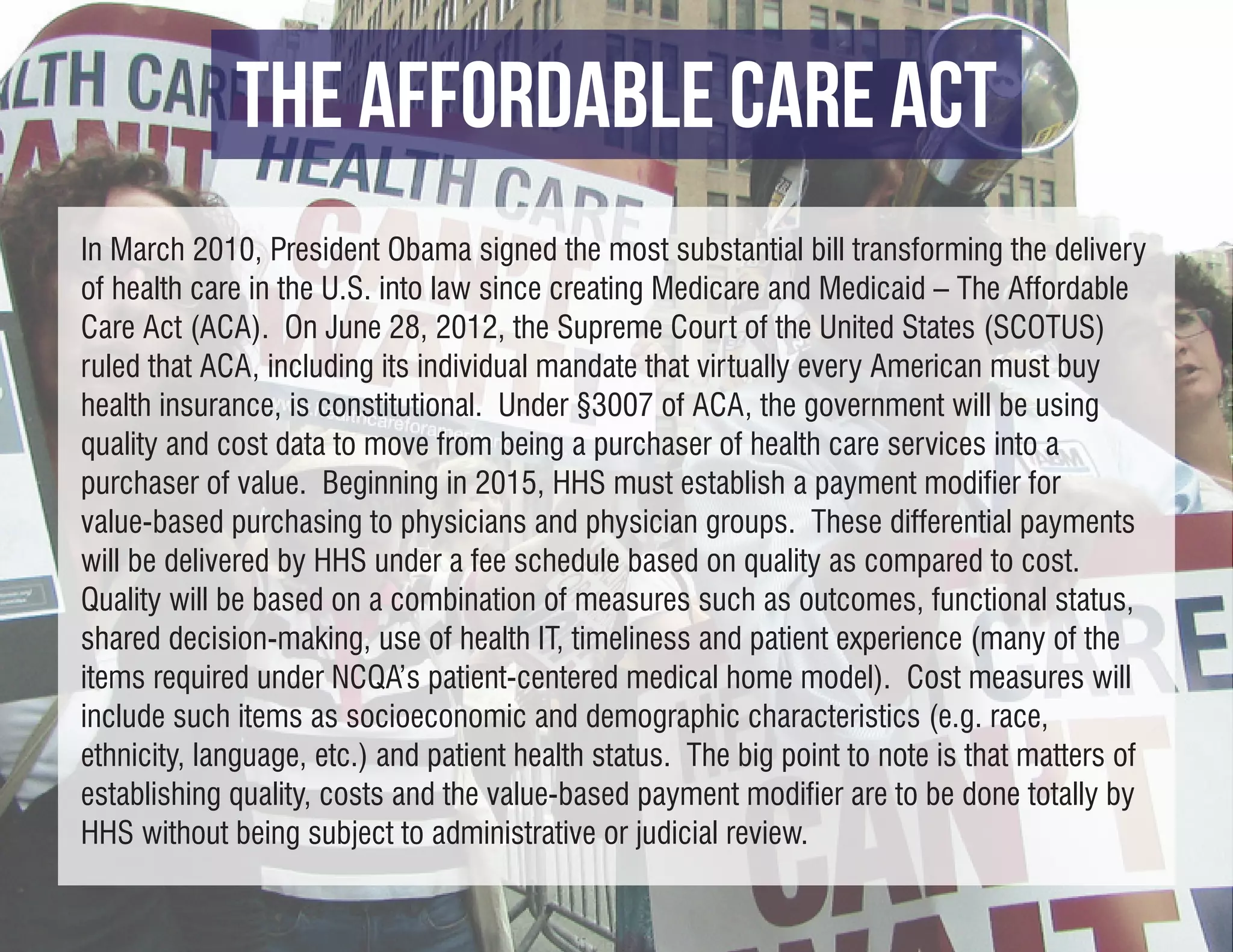
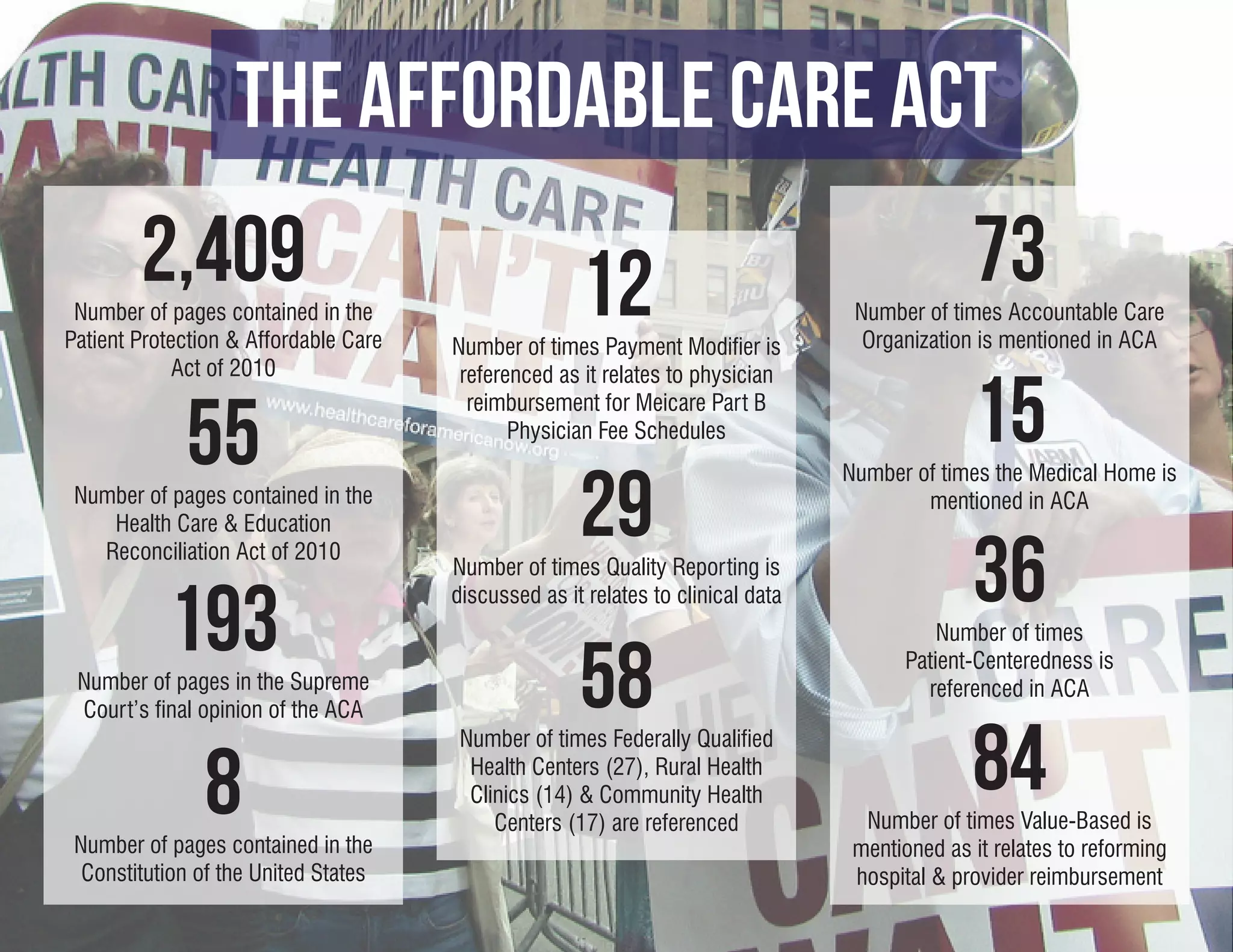
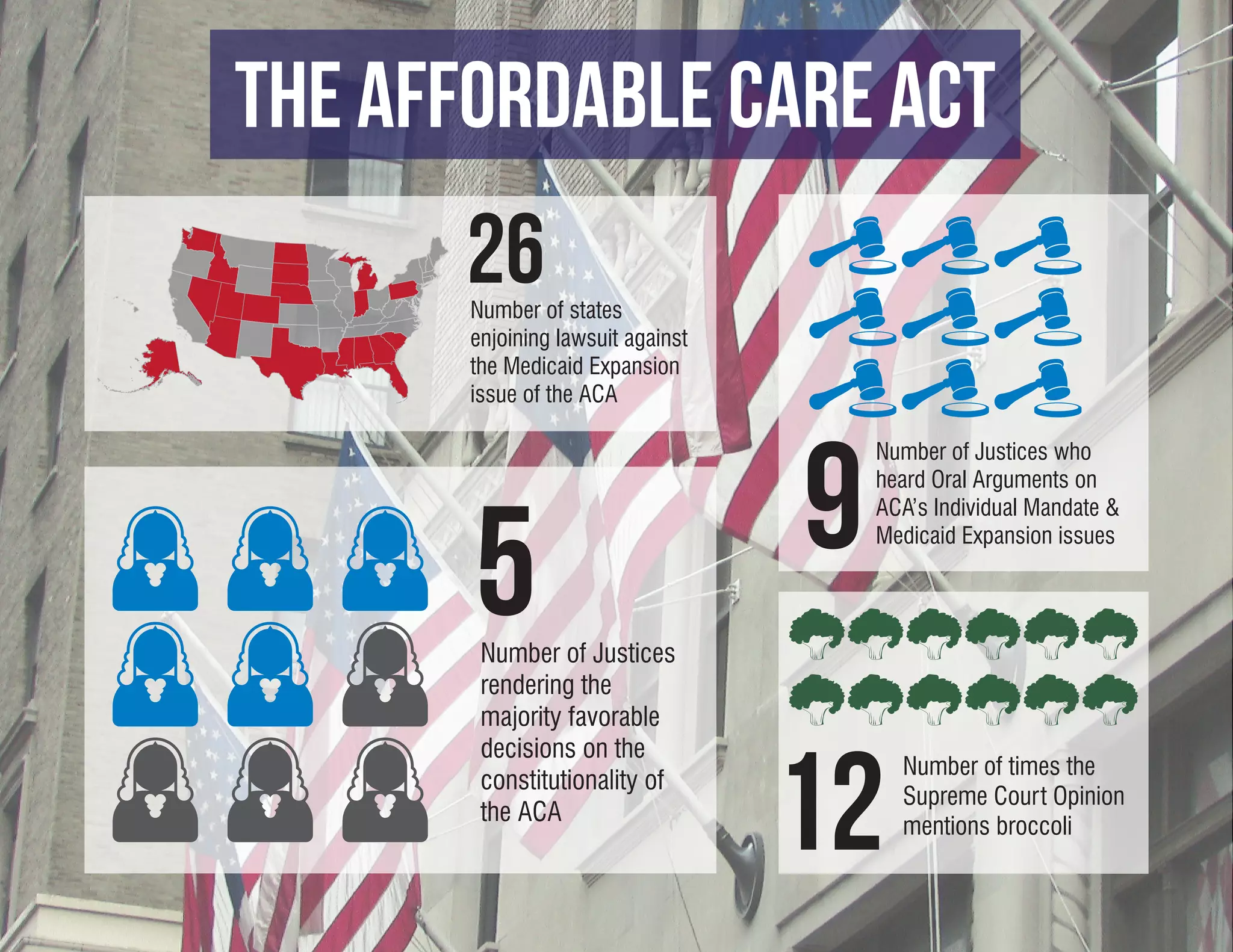
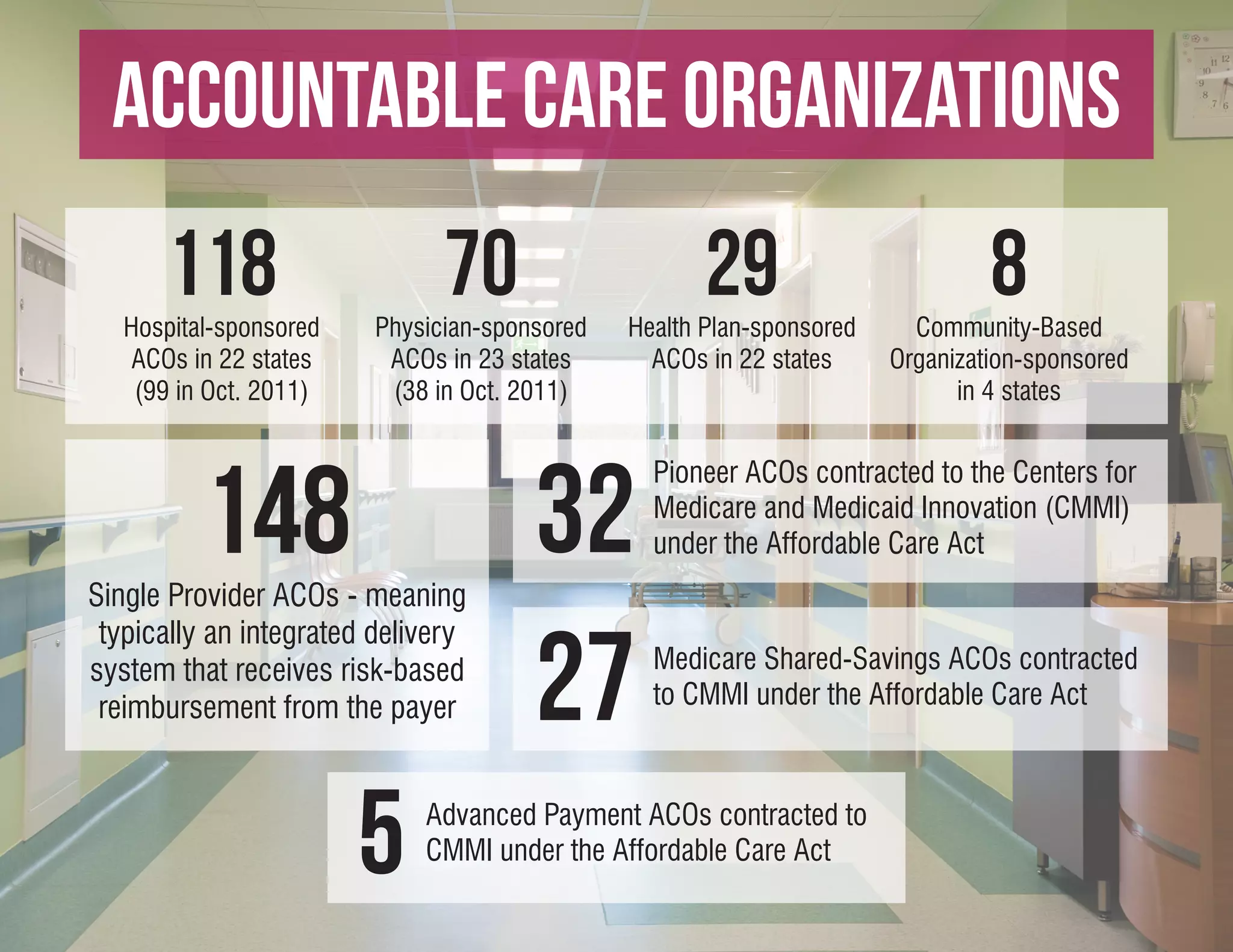
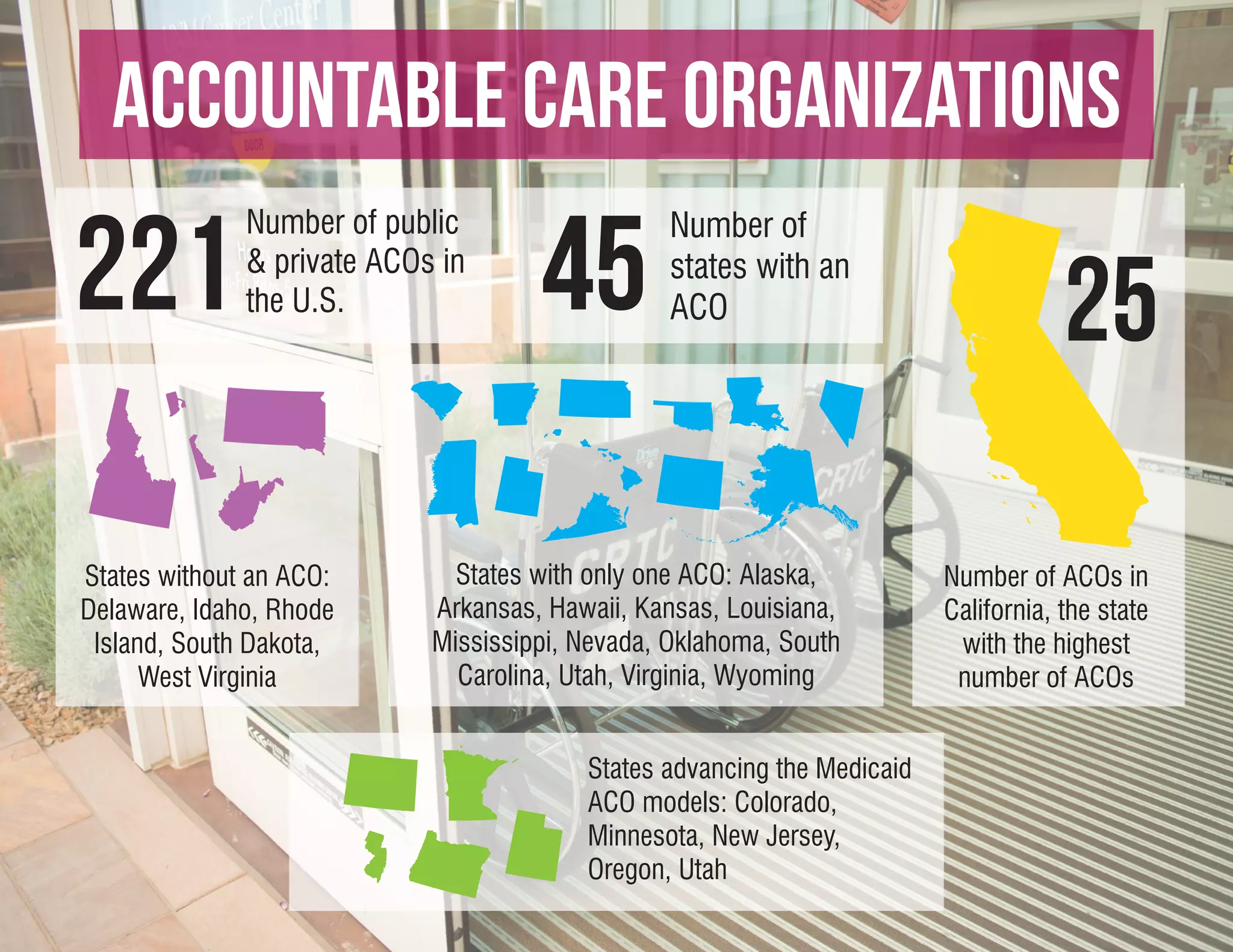
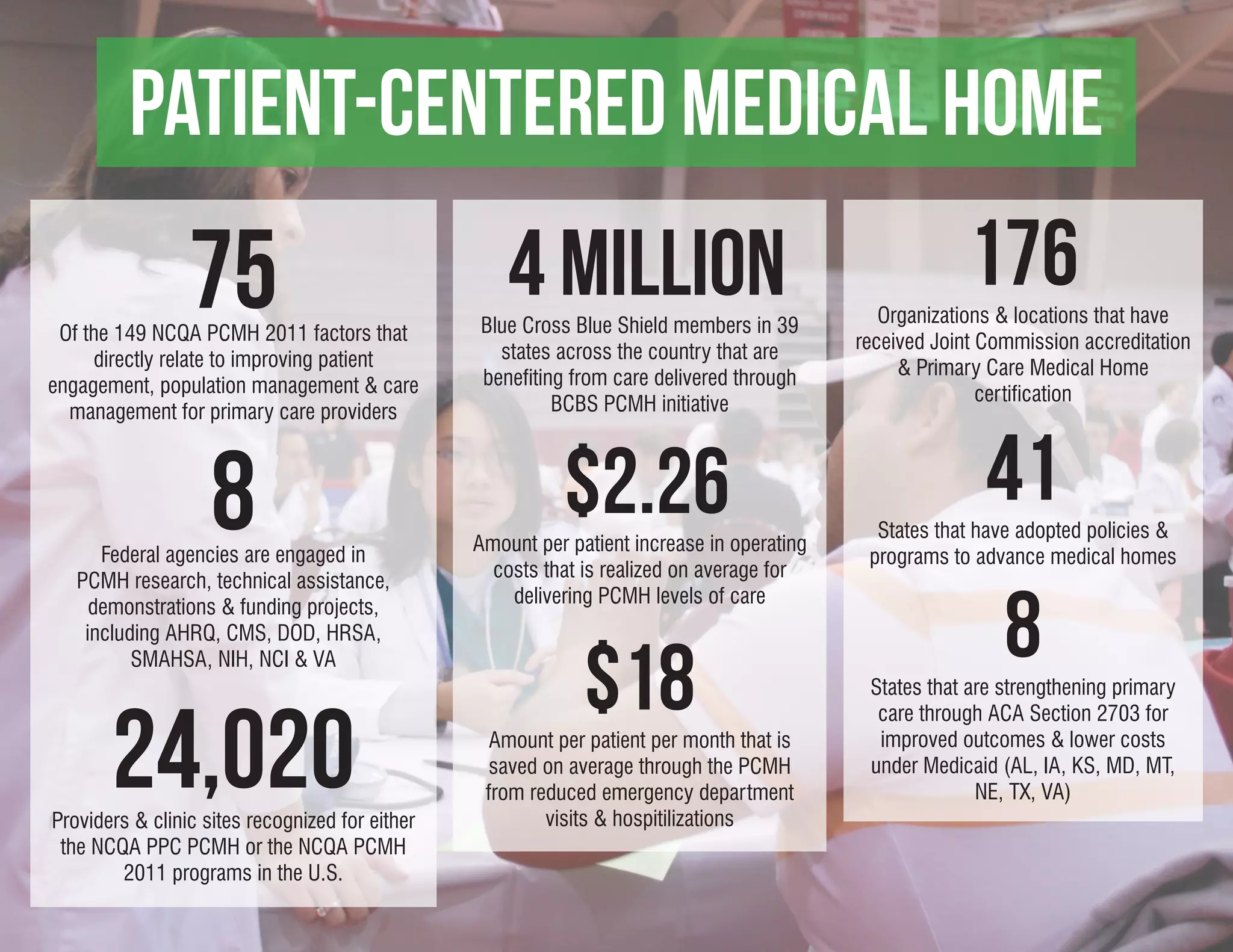
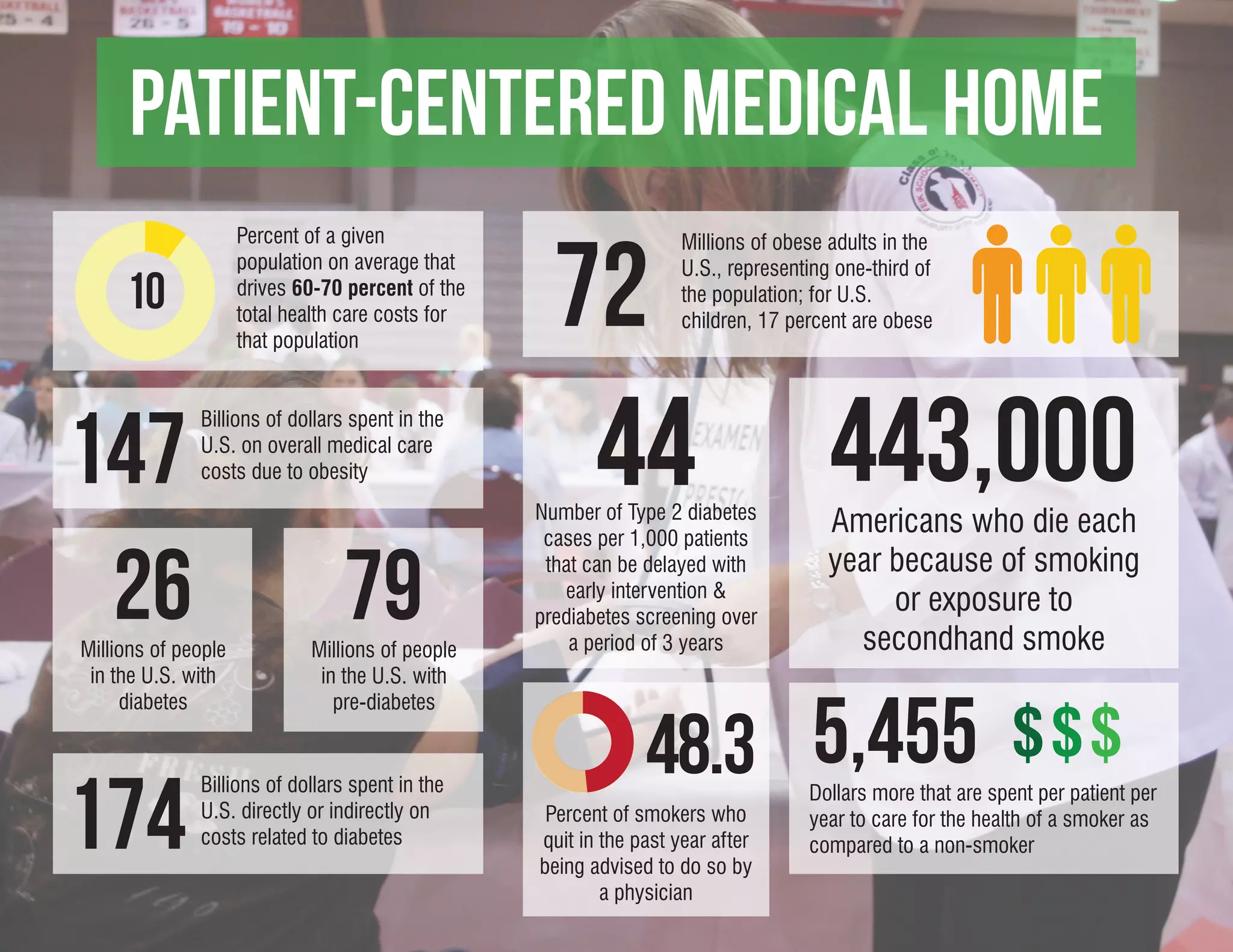
The document discusses the increasing role of the American patient in healthcare policymaking, particularly in managing chronic diseases and promoting preventive care. It highlights key healthcare initiatives, including the Affordable Care Act, meaningful use of electronic health records, and the establishment of Accountable Care Organizations to enhance patient-centered care. Furthermore, it outlines the fiscal implications of healthcare costs and demographics, emphasizing the importance of patient engagement and accountability in reducing healthcare expenditures.