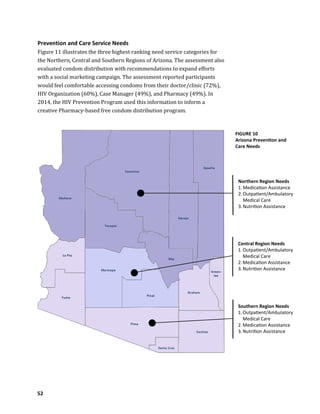
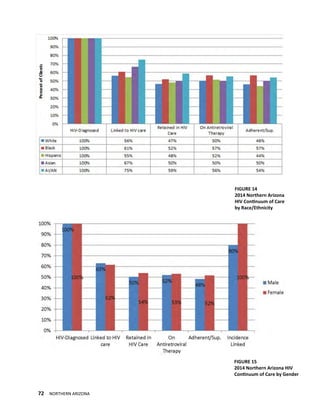
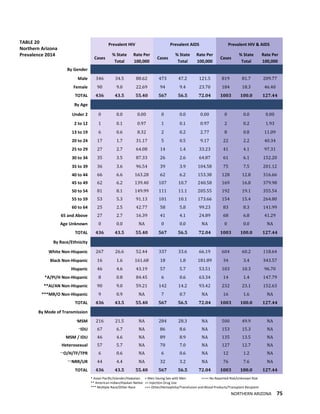
This document is Arizona's 2017-2021 plan to end the local HIV epidemic through integrated HIV prevention and care. It was developed by the HIV Statewide Advisory Group and Ryan White Planning Council with input from hundreds of stakeholders across the state. The plan aims to address barriers to care and improve engagement in prevention and treatment services through regional strategies tailored for northern, central, and southern Arizona. The goal is to end the HIV epidemic in Arizona within the next five years through coordinated, evidence-based approaches.