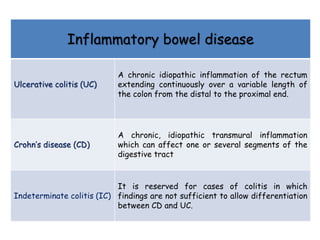
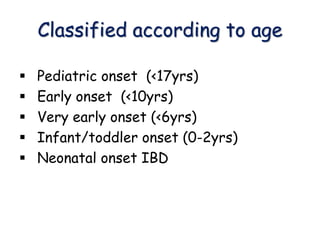
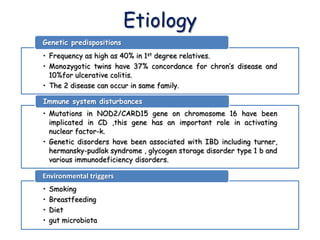
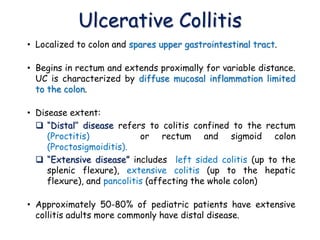
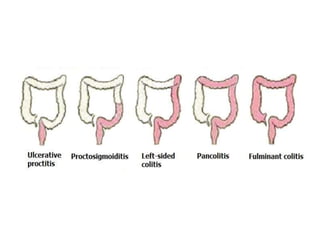
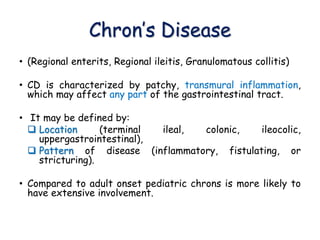
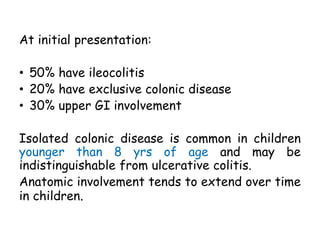
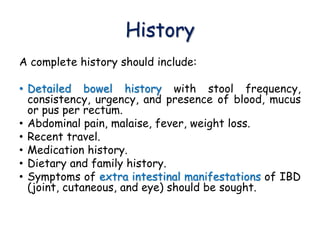
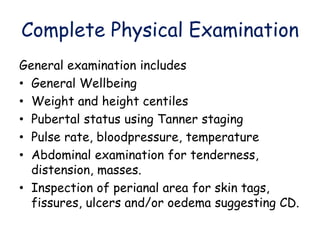
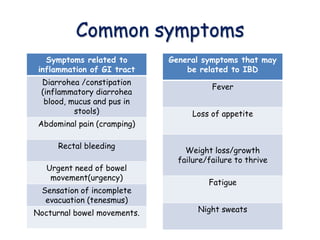
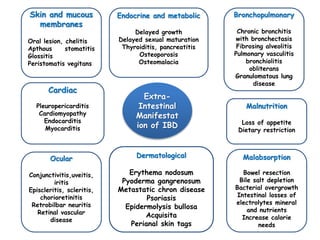
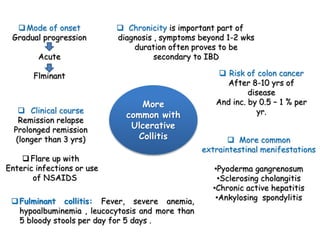
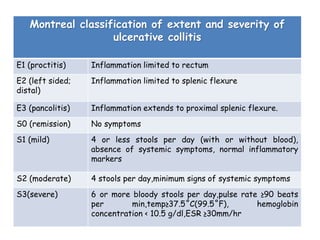
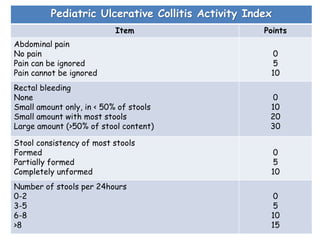
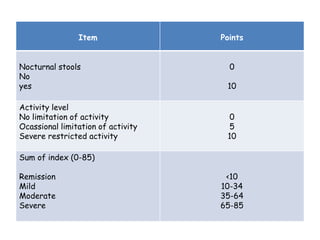
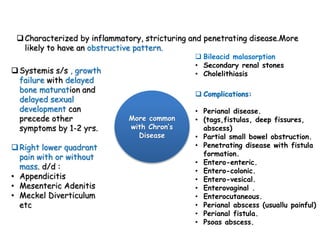
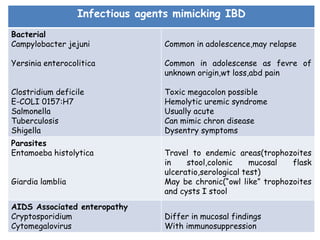
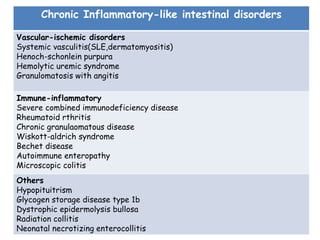
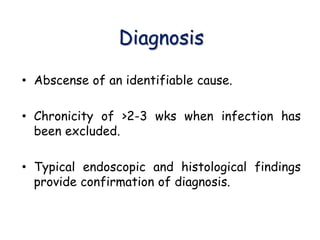
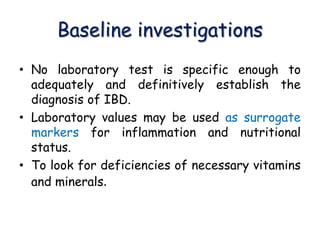
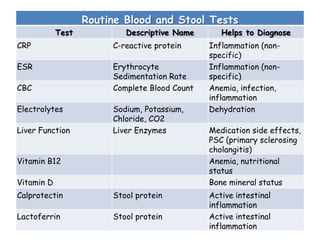
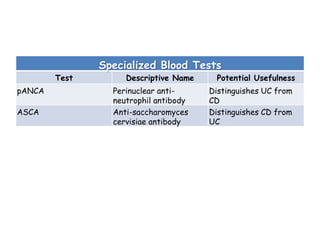
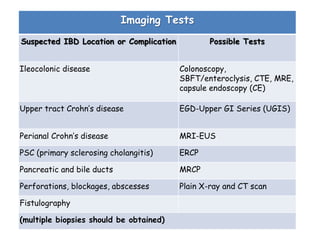
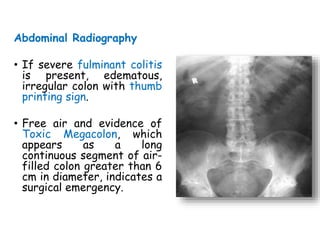
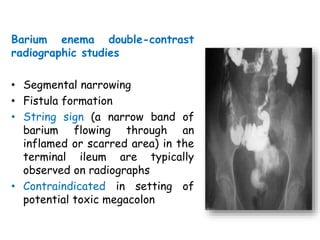
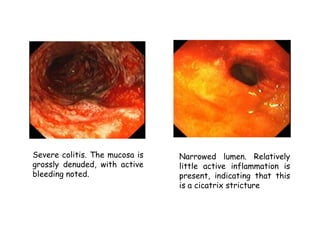
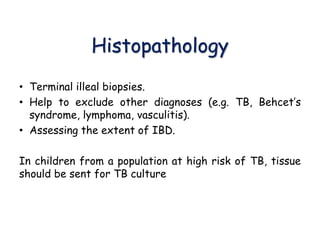
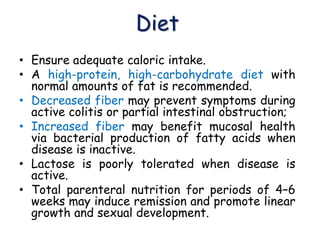
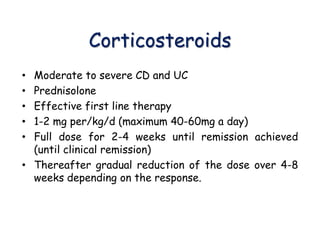
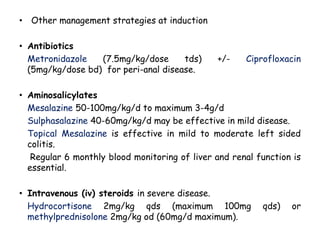
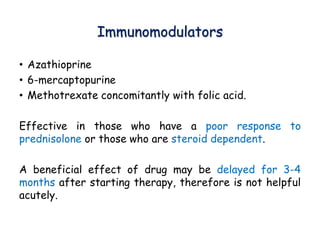
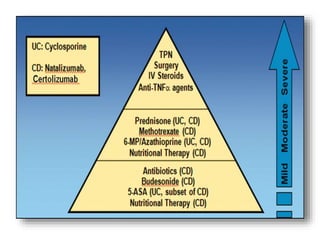
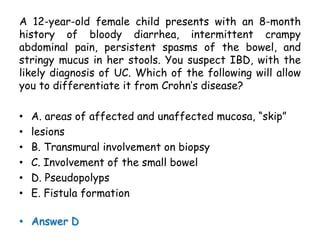
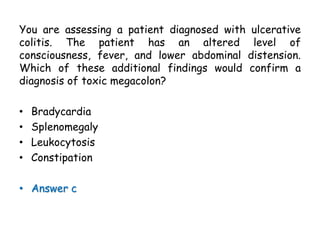
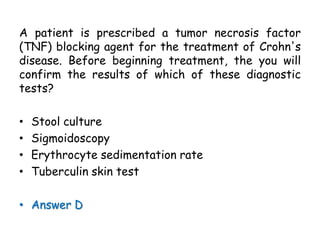
This document provides information on approaching the treatment of inflammatory bowel disease (IBD) in children. It defines the two main types of IBD as ulcerative colitis (UC) and Crohn's disease (CD). For diagnosis, it recommends a complete history, physical exam, baseline blood and stool tests, and specialized tests as needed. Treatment goals are remission induction and maintenance through medication, diet, and ensuring adequate nutrition. First-line medications include corticosteroids, aminosalicylates, antibiotics, and nutritional support through enteral or parenteral means as needed.