Nutrition management of enteral feeding - guidelines and procedures ect2353
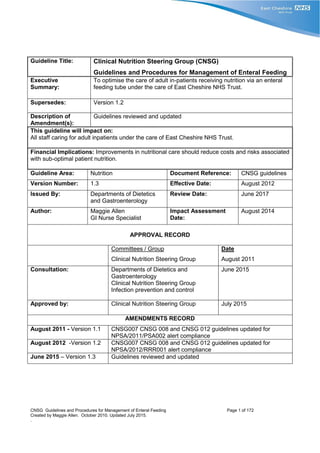
- 1. CNSG Guidelines and Procedures for Management of Enteral Feeding Page 1 of 172 Created by Maggie Allen. October 2010. Updated July 2015. . Guideline Title: Clinical Nutrition Steering Group (CNSG) Guidelines and Procedures for Management of Enteral Feeding Executive Summary: To optimise the care of adult in-patients receiving nutrition via an enteral feeding tube under the care of East Cheshire NHS Trust. Supersedes: Version 1.2 Description of Amendment(s): Guidelines reviewed and updated This guideline will impact on: All staff caring for adult inpatients under the care of East Cheshire NHS Trust. Financial Implications: Improvements in nutritional care should reduce costs and risks associated with sub-optimal patient nutrition. Guideline Area: Nutrition Document Reference: CNSG guidelines Version Number: 1.3 Effective Date: August 2012 Issued By: Departments of Dietetics and Gastroenterology Review Date: June 2017 Author: Maggie Allen GI Nurse Specialist Impact Assessment Date: August 2014 APPROVAL RECORD Committees / Group Clinical Nutrition Steering Group Date August 2011 Consultation: Departments of Dietetics and Gastroenterology Clinical Nutrition Steering Group Infection prevention and control June 2015 Approved by: Clinical Nutrition Steering Group July 2015 AMENDMENTS RECORD August 2011 - Version 1.1 CNSG007 CNSG 008 and CNSG 012 guidelines updated for NPSA/2011/PSA002 alert compliance August 2012 -Version 1.2 CNSG007 CNSG 008 and CNSG 012 guidelines updated for NPSA/2012/RRR001 alert compliance June 2015 – Version 1.3 Guidelines reviewed and updated
- 2. CNSG Guidelines and Procedures for Management of Enteral Feeding Page 2 of 172 Created by Maggie Allen. October 2010. Updated July 2015. . The following guidelines are to be used in association with CNSG 006 East Cheshire NHS Trust Enteral Feeding Policy for Adults MAIN INDEX SECTION CONTENTS PAGE CNSG007 GUIDELINES FOR INSERTION AND MANAGEMENT OF NASOGASTRIC TUBES 3-26 CNSG 008 GUIDELINES FOR INSERTION AND MANAGEMENT OF NASAL BRIDLES 27-37 CNSG 009 GUIDELINES FOR INSERTION AND MANAGEMENT OF GASTROSTOMY TUBES 38-70 CNSG 010 PROTOCOL FOR FIRST ASSISTANT ROLE IN PEG INSERTION 71-79 CNSG 011 GUIDELINES FOR SUSPECTED PERITONEAL LEAK POST PEG INSERTION 80-81 CNSG 012 GUIDELINES FOR MANAGEMENT OF A JEJUNAL TUBE 82-98 CNSG 013 GUIDELINES FOR ADMINISTRATION OF FEED 99-111 CNSG 014 GUIDELINES FOR ENTERAL FEEDING COMPLICATIONS AND MANAGEMENT 112-130 CNSG 015 MICROBIOLOGICAL GUIDELINES FOR ENTERAL FEEDING 131-139 CNSG 016 GUIDELINES FOR ADMINISTRATION OF MEDICATION VIA ENTERAL TUBES 140-153 CNSG 017 GUIDELINES FOR ASSESSMENT AND MONITORING OF PATIENTS RECEIVING ENTERAL FEEDING Available on Trust Intranet CNSG 018 GUIDELINES FOR ENTERALLY FED PATIENTS ADMITTED TO HOSPITAL 154-156 PATIENT INFORMATION AND FORMS FOR PRINTING CARE PATHWAY FOR PERCUTANEOUS ENDOSCOPIC GASTROSTOMY (PEG) TUBES 158-165 ADVICE POST PEG REMOVAL 167 PRE-DISCHARGE TRAINING CHECKLIST- GASTROSTOMY FEEDING 167-168 NASOGASTRIC (NG) TUBE INSERTION AND MONITORING FORM 169-171
- 3. East Cheshire NHS Trust CNSG 007 Guidelines for Insertion and Management of Nasogastric Tubes Page 3 of 172 Created by Maggie Allen, October 2010. Updated March 2015. Guideline Title: Guidelines for Insertion and Management of Nasogastric Tubes Executive Summary: To optimise the care of adult in-patients receiving nutrition via a nasogastric tube under the care of East Cheshire NHS Trust. Supersedes: Version 1.2 Description of Amendment(s): Guidelines reviewed - no major changes This guideline will impact on: All staff caring for adult inpatients under the care of East Cheshire NHS Trust. Financial Implications: Improvements in nutritional care should reduce costs and risks associated with sub-optimal patient nutrition. Guideline Area: Nutrition Document Reference: CNSG 007 Version Number: 1.4 Effective Date: August 2011 Issued By: Departments of Dietetics and Gastroenterology Review Date: June 2017 Author: Maggie Allen GI Nurse Specialist Impact Assessment Date: August 2014 APPROVAL RECORD Committees / Group Clinical Nutrition Steering Group Date August 2011 Consultation: Departments of Dietetics and Gastroenterology Clinical Nutrition Steering Group October 2010- August 2011. June 2015 Approved by: Clinical Nutrition Steering Group July 2015 AMENDMENT RECORDS August 2011 - Version 1.1 Guidelines updated for NPSA/2011/PSA002 alert compliance. May 2012 -Version 1.2 CNSG007 CNSG 008 and CNSG 012 guidelines updated for NPSA/2012/RRR001 alert compliance. June 2015 – Version 1.3 Guidelines reviewed April 2016 – Version 1.4 Addition to NG insertion and monitoring chart – to add ‘decision maker, name, date and time’.
- 4. East Cheshire NHS Trust CNSG 007 Guidelines for Insertion and Management of Nasogastric Tubes Page 4 of 172 Created by Maggie Allen, October 2010. Updated March 2015. GUIDELINES FOR INSERTION AND MANAGEMENT OF NASOGASTRIC TUBES INDEX Section Contents Page 1.0 Definition 5 2.0 Indications 5 3.0 Contraindications 5 4.0 Assessment 6 5.0 Referral 6 6.0 Consent 6 7.0 Types of tubes and tube selection 7 8.0 Insertion of nasogastric tubes 8-10 8.1 Procedure 8-10 9.0 Confirmation of position 11-15 9.1 pH Testing 12 9.1.1 Obtaining and checking aspirate 12-13 9.1.2 Methods for successfully obtaining gastric aspirate 13 9.1.3 Recommended pH strips and usage 13 9.1.4 PH Values 13 9.1.5 Documentation of pH result 13 9.2 X-ray testing 13-14 9.2.1 When to X-ray 13 9.2.2 How to X-ray 14 9.2.3 Who should read the X-ray 14 9.2.4 Documentation of X-ray 14 9.3 Who should check the position of the tube 14 9.4 When to check the position of the tube 15 9.5 Unsafe methods for checking NG position 15 10.0 Management of a nasogastric tube 16 10.1 When to replace a should a nasogastric tube 16 10.2 Securing a nasogastric tube 16 10.3 Flushing 16 10.4 Blocked tube 16 11.0 Nasal care 16 12.0 Mouth care 17 13.0 Removal of a nasogastric tube 17 13.1 Planned 17 13.2 Accidental 17 13.3 Repeated unplanned removal 17 14.0 Escalation procedure for patient requiring NG tube insertion 18 15.0 Discharge of patients on NG feeding 19 Appendix 1 References and bibliography 20-21 Appendix 2 Links to supporting documents Nasogastric insertion and monitoring form NPSA alerts relating to NG use Manufacturer’s information Patient information 22 Appendix 3 Algorithm to check NG position 23-24 Appendix 4 Flow chart to guide decision making for tube feeding route 25 Back to main index
- 5. East Cheshire NHS Trust CNSG 007 Guidelines for Insertion and Management of Nasogastric Tubes Page 5 of 172 Created by Maggie Allen, October 2010. Updated March 2015. 1.0 DEFINITION back to index A Nasogastric (NG) tube is a flexible tube that can be inserted transnasally into the stomach. It is commonly used for delivery of feed, fluids, medication, or drainage of gastric contents. Table 1 ADVANTAGES DISADVANTAGES COMMON COMPLICATIONS RARER COMPLICATIONS Readily available Easily inserted Easily reversed Rapid start of enteral feeds Few contraindications to placement Easily dislodged Uncomfortable Aesthetically displeasing Pulmonary intubation Pulmonary aspiration Reflux Nasal and mucosal ulceration Epistaxsis Gastrointestinal bleeding Oesophageal gastric and duodenal perforation Pneumothorax 2.0 INDICATIONS back to index Nutritional support and hydration. Nasogastric feeding is the most common method of providing short-term artificial nutritional support in the acute setting. Decision to feed with a nasogastric tube should be a multidisciplinary approach. NG tube feeding should be considered for patients who: - are malnourished. have a functioning gastrointestinal (GI) tract. require short-term tube feeding (up to 4-6 weeks). require long-term tube feeding (if an alternative route is inappropriate or not possible i.e. Percutaneous Endoscopic Gastrostomy (PEG) Radiologically Inserted Gastrostomy (RIG) or Parenteral Nutrition (PN). are unable to fulfil their nutritional requirements with normal /modified diet nutritional supplements. are not predicted to fulfil their nutritional requirements with normal / modified diet nutritional supplements. have increased nutritional requirements e.g. sepsis, trauma, post-op stress & burns. See appendix 5 for flow chart to guide decision making for tube feeding route 3.0 CONTRAINDICATIONS back to index Table 2 Absolute Relative Non-functioning GI tract e.g. ileus. Large gastric aspirate and/or high risk of aspiration. Intractable vomiting not resolved by anti-emetics. Basal skull fracture, as the tube may enter the brain if incorrectly positioned (oro-gastric positioning may be appropriate). Oesophageal varices Mucositis Vomiting responding to anti-emetics Recent radiotherapy to head and neck Advanced neurological impairment Obstructive pathology in oropharynx or oesophagus preventing passage of the tube e.g. stricture, tumour, pharyngeal pouch. Procedure may need to be done under endoscopic or fluoroscopic control. Specialist input advised.
- 6. East Cheshire NHS Trust CNSG 007 Guidelines for Insertion and Management of Nasogastric Tubes Page 6 of 172 Created by Maggie Allen, October 2010. Updated March 2015. 4.0 ASSESSMENT back to index Before a decision is made to insert a nasogastric tube, an assessment is undertaken to identify if nasogastric feeding is appropriate for the patient, and the rationale for any decision is recorded in the patient’s medical notes. The decision to insert a nasogastric tube for the purpose of feeding must be made following careful assessment of the risks and benefits by at least two competent health care professionals including the senior doctor responsible for the patient’s care. The decision to initiate enteral feeding should involve the patient, carer/family, and members of the multi-disciplinary team including speech and language therapists and dietitians as appropriate. The patient must be assessed for the most suitable route of enteral feeding e.g. stomach or small bowel and most suitable type of tube. The indication and rationale of the route and type of tube for enteral feeding will be clearly written in the patient’s medical notes. As a minimum, documentation should include signed, dated and timed entry, of the process of initial risk assessment that evaluates the benefits against the risks of introducing a nasogastric tube for the purpose of feeding. The following group of patients are at a high risk of incorrect tube positioning, dislodgement and aspiration. Appropriate specialist advice should be taken if the patient has: Maxillo-facial disorders Laryngectomy Recent radiotherapy to head and neck Any disorder of the oesophagus/pharynx e.g. varices, stricture, pharyngeal pouch. Nasal C.P.A.P. Oro-gastric positioning may be indicated following head injury or neuro surgery. High Risk also includes patients who: - Are comatose/semi-comatose Are ventilated/sedated Have a swallow dysfunction Have recurrent retching/vomiting Need to be nursed prone 5.0 REFERRALS back to index All patients requiring NG feeding should be referred to a dietitian. This may not be possible if the decision to feed is made out of hours. In this case the dietetic referral should be phoned through to the dietetic answer machine x1126. Patients with the any of the above conditions or requirements as seen above in section 4 above will be referred a Trust employee with expert knowledge of insertion of NG tubes. 6.0 CONSENT back to index Informed consent must be obtained from the patient prior to the procedure as per Trust policy for consent. The consent must be recorded in the patient’s medical notes. If the patient lacks capacity for consent, the decision to treat must be made within the patient’s best interests. The goals of the treatment should be clearly identified in the patient’s medical notes. The procedure should also be discussed with the family where appropriate.
- 7. East Cheshire NHS Trust CNSG 007 Guidelines for Insertion and Management of Nasogastric Tubes Page 7 of 172 Created by Maggie Allen, October 2010. Updated March 2015. 7.0 TYPES OF TUBES AND TUBE SELECTION back to index Nasogastric tubes are manufactured in a range of sizes and materials (polyvinal chloride (PVC), polyurethane and silicone. Feeding tubes must comply with: - 1. National Patient Safety Alert (NPSA) 19 (2007) Promoting safer measurement and administration of liquid medicines via oral and other enteral routes. Enteral feeding systems should not contain ports that can be connected to intravenous syringes, or that have end connectors that can be connected to intravenous or other parenteral lines. Enteral feeding systems should be labelled to indicate the route of administration. 2. National Patient Safety Alert (NPSA 2011) Reducing the harm caused by misplaced nasogastric feeding tubes in adults, children and infants. The tubes should be fully radio-opaque with externally visible markings to enable accurate measurement, identification and documentation of their position (NPSA 2011). NB. PVC tubes (e.g. Ryles) are not recommended for feeding as they harden in contact with gastric acid and can cause internal ulceration (Payne-James et al 2001). In addition, they do not comply with NPSA guidance. Recommended tube size 8 Fr - recommended for standard use 10Fr - recommended if large volumes of medication are required via the tube (increased risk of blockage). Rationale for use of fine bore feeding tube More comfortable Less likely to interfere with eating and drinking Less risk of reflux Less likely to delay the return of swallowing mechanism Guidewires Fine bore tubes usually have a guidewire to aid insertion. The manufacturer’s guidance should be adhered to, primarily, to ensure the guidwire is firmly positioned prior to use and never reinsert the guidewire whilst the tube is within the patient. back to index
- 8. East Cheshire NHS Trust CNSG 007 Guidelines for Insertion and Management of Nasogastric Tubes Page 8 of 172 Created by Maggie Allen, October 2010. Updated March 2015. 8.0 INSERTION OF NASOGASTRIC TUBES back to index The procedure will be carried out by an appropriate healthcare professional who has received training in the procedure and has been assessed as competent. More advanced skills may be required if the patient is at a high risk of a tube being misplaced during insertion (see section 4) Additional training or expert input should be sought if required. Placement should be delayed if there is insufficient experienced support available to accurately confirm nasogastric tube placement (e.g. at night), unless clinically urgent, and that the rationale for any decisions made is recorded in the patient’s medical notes. 8.1 Procedure back to index Equipment Clinically clean surface, CE accredited pH indicator strips, tissues, 60ml enteral/oral syringe, gloves/apron, nasogastric tube. Freshly drawn tap water to flush the tube once position confirmed. Lubricating Jelly (may not be necessary if the tube has a water activated lubricant coating e.g. Corpak Corflo tubes Nasal/cheek dressing to secure tube (included in some packs). Glass of water/coloured fluid and a straw (only if the patient has a safe swallow reflex) Table 3 Action Rational Prior to the procedure, check the medical and nursing notes for complications, e.g. anatomical variations due to surgery or cancer. These may affect the procedure and result in further complications. Patients with head injury or facial trauma may have the feeding tube passed through the mouth and down into the stomach to bypass nasal damage and cerebral oedema. Assess the patient’s requirements. The appropriate tube is inserted to meet the patient’s needs and clinical condition and that the tube is acceptable and comfortable. Explain the procedure to the patient (even if the patient appears not to understand). To ensure that the patient understands and is able to give consent, also to co-operate with the procedure. Arrange a signal so that the patient can communicate with the nurse during the procedure e.g. raise a hand. Helps to alleviate fear as the patient has some control over the procedure. Assist the patient in a semi-upright position. Support the head in a slightly forward position. Assists swallowing and helps prevent tracheal placement if the swallow is compromised. Check that the nostrils are patent by asking the patient to sniff with one nostril closed. Repeat with the other side. Alternate nostrils if replacing a tube. Helps identify potential obstruction. Prevents nasal irritation and potential ulceration. Wash hands and put on non-sterile gloves and an apron. Minimises cross infection (Anderton 1995). Unpack the tube, close the end connectors. If the tube has a guide wire, gently push it into the tube until it is fixed (see manufacturer’s guidelines in packet). Check that the tube is not kinked. Prevents the tube from coiling back on itself during insertion.
- 9. East Cheshire NHS Trust CNSG 007 Guidelines for Insertion and Management of Nasogastric Tubes Page 9 of 172 Created by Maggie Allen, October 2010. Updated March 2015. Table 3 continued Action Rational Place the tip of the tube (the distal opening, if the tube is weighted) at the xiphisternum and measure up to the tip of the nose and then to an ear lobe (NEX measurement). Note the measurement on the tube. Ensures that the correct length of tube is placed in the stomach. Lubricate the tube. Use a thin coating of water based jelly. If the tube is hydrophilic e.g. Corpak Corflo immerse the distal end of the tube in water to activate the lubricant. If re-passing a Corflo, use a lubricant. Facilitates easy passage of the tube. Insert the tip of the tube into the chosen nostril, advancing it, horizontally, gently along the floor of the nostril, parallel to the nasal septum, to the nasopharynx and then oropharynx. The patient may sneeze. Reassure. If resistance is met, withdraw slightly and alter the angle of insertion, otherwise try the other nostril. Follow the natural anatomy of the nose. If the patient is able to swallow small sips should be taken at this stage. An assistant may be required to help give thickened fluids to swallow. The swallowing action places the epiglottis over the trachea so allowing the tube to enter the oesophagus. Also the patient has something else to focus on. If liquids are contra-indicated, sometimes placing a cold spoon on the tongue may initiate a swallowing reflex. Advance the tube down the oesophagus with successive swallows until the correct measurement or mark is seen at the nostril. If the tip of the tube is in the oesophagus there is a high risk of aspiration. If too much tube is inserted it might kink in the stomach, or pass through the pylorus into the duodenum. Check the position (see section 9.0 below) To verify position in the stomach NB DO NOT FLUSH the tube before gastric placement has been confirmed. Internal guidewires/ stylets should NOT be lubricated before gastric placement has been confirmed. Water activation of the lubricant may give an inaccurate low pH result. NPSA/2012/RRR001 Fix the tube in position (See section 10.2) Helps prevent dislodgement. NB. This should be done after successful verification of the tube’s position, as it may need to be moved to obtain aspirate. If X-ray is required, the tube should be secured to the nose/cheek. back to index
- 10. East Cheshire NHS Trust CNSG 007 Guidelines for Insertion and Management of Nasogastric Tubes Page 10 of 172 Created by Maggie Allen, October 2010. Updated March 2015. Table 3 continued back to index CAUTION Never advance the tube against resistance, pull back slightly and retry. If the patient shows signs of respiratory distress i.e. coughing gasping or cyanosis, the tube may have entered the trachea. Pull the tube back or remove to allow time to recover. If respiratory distress is prolonged or worsens, seek medical assistance. Top tips (expert opinion): back to index Hold the tube straight rather than coiled in your hand. If the patient has a swallowing difficulty, altered consciousness or inability to cooperate: a) rotate the tube in your hand so that the tip points slightly upwards. This will position the tip in the correct position on the nasopharyngeal wall. b) tip the patient’s chin towards the chest. c) advance the tube through the nostril and into the nasopharynx until resistance is felt (usually 12-14cm marking on tube), there may be an involuntary swallow reflex stimulated by the tube. Advance the tube with the swallow. If no reflex, advance the tube slowly or the tube will back up into the mouth. Gentle pressure will allow the tube to pass into the oesophagus. If after 3 attempts NG insertion has failed or pulled out by the patient on three consecutive occasions, escalate as soon as possible to an experienced practitioner (senior nurse/clinician/nurse specialist). Action Rational Document Type of tube, size and lot number Name of person inserting the tube The cm measurement on the tube at the exit point from the nostril. The pH value (if gastric aspirate obtained) Which nostril The health care professional (HCP) reading the X-ray should record the result in the patient’s notes (See section 9.2.4 for further guidance) Ease of insertion Tracking and traceability For audit and training requirements Allows the user to assess whether the tube has changed position. Allows staff to compare with previous readings Prevents the same nostril being used To identify whether the tube is safe for use. For tracking and accountability. Useful information for other healthcare professionals inserting subsequent tubes. Dispose of clinical waste as per Trust policy. The guide wire must be placed in the sharps bin. Prevent contamination and sharps accident. Wash hands as per Trust policy Minimise risk of contamination
- 11. East Cheshire NHS Trust CNSG 007 Guidelines for Insertion and Management of Nasogastric Tubes Page 11 of 172 Created by Maggie Allen, October 2010. Updated March 2015. 9.0 CONFIRMATION OF TUBE POSITION back to index NOTHING should be introduced down the tube before gastric placement has been confirmed; DO NOT FLUSH the tube before gastric placement has been confirmed; Internal guidewires/ stylets should NOT be lubricated before gastric placement has been confirmed. http://www.nrls.npsa.nhs.uk/resources/type/alerts/?entryid45=133441 pH testing is used as the first line test method, with pH between 1 and 5.5 as the safe range, and that each test and test result is documented on a chart kept at the patient’s bedside. An attempt at pH testing must be carried out following every nasogastric tube insertion even if the criteria for x-ray testing are met. This will allow for a baseline recording. Studies suggest a 90% + success rate in obtaining aspirate. X-ray is used only as a second line test when no aspirate could be obtained or pH indicator paper has failed to confirm the position of the nasogastric tube. NPSA/2011/PSA002 alert: Reducing the harm caused by misplaced nasogastric feeding tubes in adults, children and infants. 9.1 pH Testing back to index 9.1.1 Methods for successfully obtaining gastric aspirate Aspiration of gastric contents is sometimes difficult. The table below offers suggestions. A combination of these may be required. Refer to algorithms 1 and 2 in appendix 3 for further guidance. Patience is required. Table 4 ACTION RATIONAL Always use a large enteral syringe (50cc min). Small syringes have insufficient draw. Insert 20 – 30mls of air, then aspirate. Repeat several times, aspirating after each injection of air. If unable to aspirate air, move the tube in or out until air is returned. Usually a small amount of fluid will be returned with the air (0.5mls is sufficient to cover the pH strip). The most common position for a return of aspirate is when the tube markings show between 52-60cm at the exit from the patient’s nose (expert opinion). Pushes the tube away from the gastric mucosa, which may occlude the tube. Allows the stomach to inflate and redistribute the position of fluid slightly (Colagiovanni 1999). Lie the patient on their left side. Gastric fluid will pool in a different position. Alter the position of the tube and retry. The tube may be positioned insufficiently, or too far into the stomach. Flush the tube with water following aspiration Gastric acid causes the protein in the feed to coagulate and increases the risk of tube blockage.
- 12. East Cheshire NHS Trust CNSG 007 Guidelines for Insertion and Management of Nasogastric Tubes Page 12 of 172 Created by Maggie Allen, October 2010. Updated March 2015. 9.1.2 Recommended pH strips and usage Tube position must be checked using pH indicator strips that are CE marked, intended by the manufacturer to test human gastric aspirate and have a clear definition between pH 5-6 (NPSA 2005, 2011). pH strips must be used and stored according to manufacturer’s instructions. The reagent section should not be contaminated before use through handling or inappropriate storage. It is not accepted practice to put gastric aspirate onto the syringe wrapping/cover and then to run reagent strips through the aspirate. This may alter the pH reading (NPSA 2005). NB. The lids must be kept on the containers when not in use. One box per patient – sharing has a high risk of cross contamination. The box must be decontaminated once it is no longer required for a patient. back to index 9.1.3 pH Values A pH of less than 5.5 is a reasonable indicator of gastric placement. (NPSA 2005) The pH of pulmonary fluid is normally above 6 The pH of intestinal fluid is normally above 6 Gastric pH levels may be elevated above 5.5 due to: - a) Medication i.e. H2 antagonists and proton pump inhibitors which inhibit or reduce acid production; antacids temporarily reduce gastric acidity by neutralising hydrochloric acid. b) Reflux of intestinal contents into the stomach (Metheny et al 1994b). c) Dilution of gastric acid due to: recent feed/flush: wait half an hour and retry. continuous feeds: consider stopping the feed for half an hour (Colagiovanni 1999). CAUTION: Stopping feed should be carried out with extreme caution for patients on insulin infusions for tight glycaemic control and only if other methods have failed. Stop insulin infusion whilst the feed is turned off (NPSA 2005). If aspirate values are higher than normal, it can be hard to assess the position of the tube. Using algorithms 1 and 2 in appendix 3 will help individuals to assess and rationalise their decision making in order to make NG tube management as safe as possible. 9.1.4 Documentation of pH result Each pH test and result must be documented on the nasogastric monitoring form kept at the patient’s bedside. back to index
- 13. East Cheshire NHS Trust CNSG 007 Guidelines for Insertion and Management of Nasogastric Tubes Page 13 of 172 Created by Maggie Allen, October 2010. Updated March 2015. 9.2 X-Ray testing Table 5 Method Advantages Disadvantages X-ray 2nd line testing method. See section 9.2 for indications This is the most accurate method of confirming positioning. No guarantee that the tube is still in position once the patient has returned to the ward and for the subsequent duration of NG feeding. Risk of frequent exposure to X-rays. Delay in commencing feeding via the tube. Cost and resource implications. Impractical for patients based in the community (Colagiovanni 1999). 9.2.1 When to X-ray back to index X-ray following insertion is only indicated if: The patient is unconscious with no gag reflex (ICU protocol). The patient has altered anatomy e.g. known large hiatus hernia, pharyngeal pouch, previous surgery on the upper GI tract. There is absence of aspirate pH testing is inconclusive. Difficult tube insertion. Fractured base of skull. Recent radiotherapy to head and neck. Recent surgery to head and neck. X-ray should not be used routinely to confirm tube position during subsequent use. If you are unable to confirm position using the above guidelines, refer to algorithms 1 and 2 in appendix 1 for further guidance for checking the tube position following failure to obtain aspirate or inconclusive pH values. An attempt at pH testing must be carried out following every nasogastric tube insertion even if the criteria for x-ray testing are met. This will allow for a baseline recording. Studies suggest a 90% plus success rate in obtaining aspirate. (NPSA 2011). 9.2.2 How to X-ray back to index When ordering an X-ray check, the request form must clearly state that the purpose of the x-ray is to establish the position of the nasogastric tube for the purpose of feeding. The radiographer is responsible for: - Ensuring that the nasogastric tube can be clearly seen on the x-ray to be used to confirm tube position. Adjusting the exposure of the x-ray to allow the nasogastric tube to be visible to the bottom of the film. Ensuring that the film is centred lower than would normally be appropriate for a chest x-ray so that it shows the abdomen as far as possible below the diaphragm. Adjusting the x-ray film to show the bottom of both hemi-diaphragms in the midline.
- 14. East Cheshire NHS Trust CNSG 007 Guidelines for Insertion and Management of Nasogastric Tubes Page 14 of 172 Created by Maggie Allen, October 2010. Updated March 2015. X-rays that are not as described above will not allow accurate interpretation of nasogastric tube placement and should not be allowed out of the x-ray department. If there is any difficulty in interpretation the advice of a radiologist should be sought. Any nasogastric tubes identified to be in the lung should immediately be removed whether in the x- ray department or clinical area. 9.2.3 Who should read the X-ray? back to index X-rays must be checked by an appropriately trained clinician/advanced nurse practitioner, with evidence to support this skill. 9.2.4 Documentation of X-ray Documentation following X-ray should include: who authorised the x-ray who confirmed the position of the nasogastric tube. This person must be evidenced as competent to do so confirmation that any x-ray viewed was the most current x-ray for the correct patient the rationale for the confirmation of position of the nasogastric tube, i.e. how placement was interpreted, and clear instructions as to required actions. For example: 19 January 2011, 10:30 – Dr A. Smith – core surgical trainee X-ray taken at 10:15 today NG tube passed down midline, past level of diaphragm and deviates to left Tip is seen in stomach Plan: NG tube safe to use for feeding Dr A. Smith 9.2.5 Cautions There is no guarantee that the tube is still in position once the patient has returned to the ward and for the subsequent duration of NG feeding. The tube position i.e. centimetre marking at the tube’s exit from the nostril, should be checked and compared with the position post insertion, by the member of staff using the tube immediately prior to use. Risk of frequent exposure to X-rays. Delay in commencing feeding via the tube. Cost and resource implications. Impractical for patients based in the community 9.3 Who should check the position of the tube? back to index Any health professional/carer/patient prior to using the tube. In the majority of cases nurses pass the tube and manage subsequent feeding. A nurse may be involved in training a patient/carer to manage the tube.
- 15. East Cheshire NHS Trust CNSG 007 Guidelines for Insertion and Management of Nasogastric Tubes Page 15 of 172 Created by Maggie Allen, October 2010. Updated March 2015. 9.4 When to check the position of the tube back to index After initial tube insertion At least once per shift if continuous feeds are in progress Before each bolus feed, fluid or drug administration. If the patient complains of discomfort or feed reflux in the throat or mouth. If the patient suddenly shows signs of respiratory distress, e.g. breathlessness, strider, cyanosis or wheezing. Vomiting or violent retching. Severe coughing bouts. If the measurement marking the tube’s exit from the nose has changed. If the tube length appears to have changed. Following transfers from other clinical areas if feed in progress. 9.5 Unsafe methods for checking NG position back to index Table 6 METHOD REASON WHY UNSAFE Auscultation – the injection of 20 –30mls of air into the tube via a syringe whilst listening with a stethoscope over the left upper quadrant or epigastrium for a distinctive sound whooshing sound. Auscultation cannot predict whether tube tip location is in the oesophagus, stomach or respiratory tract (Metheny et al 1990a and Neumann and Meyer 1995). Unsuitable for obese patients, as no sound may be heard. There are reported cases showing that NG tubes checked by air auscultation were later shown to have tracheopulmonary placement. (Rassias et al 1998). Eleven deaths reported between 2002-2004 due to misplaced NG tubes following auscultation tests and using litmus paper (NPSA 2005, Colagiovanni 1999). Checking ability to speak Fine bore tubes are small enough not to affect speech (Colagiovanni 1999). Signs of respiratory distress Fine bore tubes might not cause respiratory distress. Patients with a poor gag reflex, or altered consciousness might not demonstrate these signs. Using Litmus paper to test aspirate Insufficiently accurate Turns pink/red in contact with aspirate that has a pH value as high as 6.5 (NPSA 2005). Placing the proximal end of the nasogastric tube in water and watching for bubbles to indicate placement in the lungs. If no bubbles, the tube is in the stomach. Inaccurate and unsafe (Colagiovanni 1999).
- 16. East Cheshire NHS Trust CNSG 007 Guidelines for Insertion and Management of Nasogastric Tubes Page 16 of 172 Created by Maggie Allen, October 2010. Updated March 2015. 10.0 MANAGEMENT OF A NASOGASTRIC TUBE back to index 10.1 When to replace a nasogastric tube Refer to manufacturer’s guidelines and individual patient assessment. Table 7 TUBE TIME Ryles tube Used for aspiration only 10 days, or sooner, if causing discomfort (Dougherty and Lister 2004) Corpak Corflo tube The manufacturers of Corflo tubes do not state a time limit for usage and suggest that they can be used as long as they are functional. (Merck communication). Decision to replace will depend on: - Viability of the tube Tolerance of the procedure by the patient Difficulty in insertion Other tubes Check with manufacturer/nurse specialist 10.2 Securing a nasogastric tube back to index The tube should be fixed at the nose with a plaster. If tube has already been accidentally removed on multiple occasions a nasal retention device (bridle) should be considered (NICE Clinical Guidelines (32) 2006) . .See Guidelines for Insertion and Management of Nasal Bridles for further information. The external part of the tube should be brought to the same side of the face as the insertion nostril and allowed to rest over the ear. - A dressing (preferably clear for aesthetic reasons) should be placed over the tube along the cheek. This is recommended for the following reasons: Less irritating for the patient as it secures the tube out of their line of sight. - Does not interfere with the patient’s eating, by keeping the tube away from the mouth. - A confused patient is less likely to pull the tube out as they cannot see it or feel it when they bring their hands up to the mouth area. - Patients receiving humidified oxygen (excess moisture makes the nasal tape slip). The dressings should be checked regularly and replaced if dirty or peeling off. The skin should be cleaned of any residual adhesive prior to replacing the tape/dressing. 10.3 Flushing back to index Refer to CNSG 013 Guidelines for Administration of Feed and Fluid via Enteral Tubes. 10.4 Blocked tube See CNSG 014 Guidelines for Enteral Feeding Complications and Management. 11.0 NASAL CARE The nose should be checked and cleaned daily. If the nose appears sore or ulcerated, consider re-passing the tube via the other nostril. back to index
- 17. East Cheshire NHS Trust CNSG 007 Guidelines for Insertion and Management of Nasogastric Tubes Page 17 of 172 Created by Maggie Allen, October 2010. Updated March 2015. 12.0 MOUTH CARE back to index Maintenance of oral hygiene is essential, particularly is a patient is unable to have oral food and fluids attend to their own oral care Table 8 PROBLEM REASON ACTION Dry sore mouth Inadequate mouth care Mouth breathing Poor dental condition Clean teeth/dentures with a soft toothbrush or a damp swab wrapped around a gloved finger (depending on patient). The frequency will depend on the condition of the patient, twice daily minimum). Check the tongue and the hard palate for thickened secretions and remove. Use lip salve to protect lips from chapping. Consider use of artificial saliva if appropriate Refer to dentist if necessary. Saliva : - Tenacious Hyper-salivation Dehydration Neurological condition Unable to swallow oral secretions Ensure adequate fluids. Consider drug therapy. Consult doctor. Maintain good oral hygiene. Refer to Guidelines for the Oral Healthcare of Stroke Survivors by the British Society of Gerodontology for comprehensive guidance as to management of oral hygiene. http://www.gerodontology.com/content/uploads/2014/10/stroke_guidelines.pdf 13.0 REMOVAL OF A NASOGASTRIC TUBE 13.1 Planned The patient must be referred to the dietitian prior to discontinuation of enteral feeding for review as to whether oral intake is sufficient and whether oral supplements may be required. 13.2 Accidental If the tube is still required for nutrition, fluids or medication, it should be reinserted as soon as possible – within a 6 hour period is recommended. See below for Escalation Procedure (section 14.0) for patient requiring NG tube insertion. In addition: - Ensure that the tube is correctly positioned and secured, as above, when reinserted. Arrange for alternative fluid support as necessary. Arrange for an alternative route for medication as appropriate. 13.3 Repeated unplanned removal If unplanned removal is repeated, refer to CNSG 008 Nasal Bridle guidelines Appendix 1 flow chart to manage repeated unplanned removal of nasogastric tube. back to index
- 18. East Cheshire NHS Trust CNSG 007 Guidelines for Insertion and Management of Nasogastric Tubes Page 18 of 172 Created by Maggie Allen, October 2010. Updated March 2015. 14.0 Escalation procedure for patients requiring NG tube insertion with or without introducer. back to index Patient requires NG tube Competent nurse unavailable Competent Medical F1/F2 to insert F1 /F2 unavailable or do not have skill to insert within two hours of request: Escalate Competent Nurse identified and inserts as per Trust Guidelines for Insertion and Management of Nasogastric Tubes Fully document procedure in medical and nursing notes NG tube becomes Blocked Dislodged Accidentally removed Refer to competent nurse within area if unavailable escalate Escalate to: In hours Senior nurse /Matron for area. MNP/PSP Registrar GI specialist nurse Outreach team Out of hours Senior nurse for area Hospital senior nurse/Night sister Registrar Competent in the procedure Matrons Sam Leonard and Hayley Readiing August 2010
- 19. East Cheshire NHS Trust CNSG 007 Guidelines for Insertion and Management of Nasogastric Tubes Page 19 of 172 Created by Maggie Allen, October 2010. Updated March 2015. 15.0 Discharge of patients on NG feeding Patients must have prior to discharge: - A multidisciplinary risk assessment to assess needs (Appendix 5 Flow chart to guide decision making for tube feeding route) Referral to a dietitian Training and assessment of competency for them and/or their carers for tube care and feeding. An agreed plan if tube removed accidentally or blocked. A discharge pack to include: - o Care of NG tube o Care of equipment o Contact numbers o Feeding regimen o Position monitoring form o CE accredited pH strips o Manufacturer’s guidelines for using pH strips o Spare NG tube o 7 days feed and equipment o How to maintain oral hygiene Action plan if tube removed The plan will depend on the patient’s circumstances and the support available in the community If tube comes out overnight wait until daytime for replacement If the patient has had recent radiotherapy treatment at Christie, they will be at a high risk of procedure related complications. In the absence of specialist support, refer them back to Christie hospital. If the patient has head and neck cancer and has had treatment at Leighton hospital, they have open access to ward 10 and should return there for tube placement. Any other patients should come to come to A&E bringing their spare tube with them. back to index
- 20. East Cheshire NHS Trust CNSG 007 Guidelines for Insertion and Management of Nasogastric Tubes Page 20 of 172 Created by Maggie Allen, October 2010. Updated March 2015. APPENDIX 1 - REFERENCES AND BIBLIOGRAPHY back to index Anderton A. (1995). Reducing bacterial contamination in enteral tube feeds. British Journal of Nursing 4(7); 368-376 BAPEN (2004). Drug administration via enteral feeding tubes. A Guide for General Practitioners and Community Pharmacists. British Association for Parenteral and Enteral Nutrition, Maidenhead. BAPEN (1996) Standards and Guidelines for Nutritional Support in Hospitals (ed. T. Sizer). British Association for Parenteral and Enteral Nutrition, Maidenhead. Boyes, R.J., Kruse, J.A. (1992) Nasogastric and nasoenteric intubation. Critical Care Clinics 8(4): 865-867. British Society of Gerodontology (2010) Guidelines for the Oral Healthcare of Stroke Survivors. http://www.gerodontology.com/content/uploads/2014/10/stroke_guidelines.pdf Colagiovanni L. (1999) Taking the tube. Nursing Times 95:21 Supplement. Colagiovanni L. (2000) Preventing and clearing blocked feeding tubes. Nursing Times. 96(17): 3-4. Dougherty, L. & Lister S. (eds) (2004) The Royal Marsden Manual of Clinical Nursing Procedures, 6th edn. Blackwell Science Ltd, Oxford. Infection Control Nurses Association (2003) Enteral feeding. Infection control guidelines. ICNA in Partnership with Nutricia. Fater, K.H. (1995) Determining nasoenteral feeding tube placement. MedSurg Nursing, 4(1): 27- 32. Human Rights Act 1998 Medicines and Healthcare products Regulatory Agency (MHRA 2000) Single-use Medical Devices: Implications and Consequences of Reuse. MDA DB2000(04) Medicines and Healthcare products Regulatory Agency (MHRA 2000) Enteral Feeding Systems. MDA SN2000(27). Medicines and Healthcare products Regulatory Agency (MHRA2004) Enteral feeding tubes (nasogastric) MDA/2004/026 Mental Capacity Act 2005 Metheny N. et al. (1990a) Detection if inadvertent respiratory displacement of small bore feeding tubes: a report of 10 cases. Heart Lung 19(6): 631-638. Metheny N. et al. (1990b) Effectiveness of the ausculatory method in predicting feeding tube location. Nursing Research 39:262-7. Metheny N. et al. (1993) How to aspirate from small bore feeding tubes. American Journal of Nursing, May 86-89. Metheny N. et al. (1993) Effectiveness of pH measurements in predicting feeding tube placement: an update. Nursing Research 42(6): 324-331. back to index back to index
- 21. East Cheshire NHS Trust CNSG 007 Guidelines for Insertion and Management of Nasogastric Tubes Page 21 of 172 Created by Maggie Allen, October 2010. Updated March 2015. Metheny N. et al. (1994a) Visual characteristics of aspirates from feeding tube as a method for predicting tube placement. Nursing Research 43(5): 282-287. Metheny N. et al. (1994b) pH testing of feeding tube aspirates to determine placement. Nutrition in Clinical Practice 9(5): 185-190. National Institute for Clinical Excellence (NICE) (2013) Nutrition support in adults Evidence Update August 2013. A summary of selected new evidence relevant to NICE clinical guideline 32 ‘Nutrition support in adults: oral nutrition support, enteral tube feeding and parenteral nutrition’ (2006) Evidence Update 46 National Patient Safety Agency (2012) Harm from flushing of nasogastric tubes before confirmation of placement NPSA/2012/RRR001 22/03/12 http://www.nrls.npsa.nhs.uk/resources/type/alerts/?entryid45=133441 National Patient Safety Agency (2011) Reducing the harm caused by misplaced nasogastric feeding tubes in adults, children and infants. NPSA/2011/PSA002 http://www.nrls.npsa.nhs.uk/alerts/?entryid45=129640 National Patient Safety Agency (2007) Promoting safer measurement and administration of liquid medicines via oral and other enteral routes NPSA/2007/19 http://www.nrls.npsa.nhs.uk/alerts/?entryid45=59808 National Patient Safety Agency (2005) Reducing the harm caused by misplaced nasogastric feeding tubes NPSA/2005/05 http://www.nrls.npsa.nhs.uk/resources/type/alerts/?entryid45=59794&p=4 National Institute for Clinical Excellence (NICE) (2012) clinical guideline 139 Infection Prevention and control of healthcare-associated infections in primary and community care http://guidance.nice.org.uk/CG139 National Institute for Clinical Excellence (NICE) (2006) Nutrition Support in Adults: oral supplements, parenteral and enteral feeding. London. http://www.nice.org.uk/nicemedia/live/10978/29981/29981.pdf Neumann M.J., Meyer C.T. (1995) Hold that X-ray: aspirate pH and auscultation prove enteral tube placement. Journal of Clinical Gastroenterology 20(4): 293-295 Nursing and Midwifery Council (2015) The Code: Professional standards of practice and behaviour for nurses and midwives. London, NMC. Payne-James, J., Grimble, G. & Silk, D. (2001) Enteral nutrition: tubes and techniques of delivery. In: Artificial Nutritional Support in Clinical Practice, 2nd edn (eds J. Payne-James, G. Grimble & D. Silk). Greenwich Medical Media, London. Powell K.S. et al (1993) Aspirating gastric residuals causes occlusion of small bore feeding tubes. Journal of Parenteral and enteral Nutrition. 17(3): 243-246 Rassias A.J. et al (1998). A prospective study of tracheopulmonary complications associated with the placement of narrow bore feeding tubes. Critical Care 2: 25-28. back to index
- 22. East Cheshire NHS Trust CNSG 007 Guidelines for Insertion and Management of Nasogastric Tubes Page 22 of 172 Created by Maggie Allen, October 2010. Updated March 2015. APPENDIX 2 LINKS TO SUPPORTING DOCUMENTS/NG CAREPLAN back to index NASOGASTRIC (NG) TUBE INSERTION AND MONITORING FORM – click on to access. Patient Information leaflets Drug administration via enteral feeding tubes http://www.bapen.org.uk/pdfs/d_and_e/de_pat_guide.pdf NPSA alerts relating to Nasogastric feeding National Patient Safety Agency (2012) Harm from flushing of nasogastric tubes before confirmation of placement NPSA/2012/RRR001 22/03/12 http://www.nrls.npsa.nhs.uk/resources/type/alerts/?entryid45=133441 National Patient Safety Agency (2011) Reducing the harm caused by misplaced nasogastric feeding tubes in adults, children and infants. NPSA/2011/PSA002 http://www.nrls.npsa.nhs.uk/alerts/?entryid45=129640 National Patient Safety Agency (2007) Promoting safer measurement and administration of liquid medicines via oral and other enteral routes NPSA/2007/19 http://www.nrls.npsa.nhs.uk/alerts/?entryid45=59808 National Patient Safety Agency (2005) Reducing the harm caused by misplaced nasogastric feeding tubes NPSA/2005/05 http://www.nrls.npsa.nhs.uk/resources/type/alerts/?entryid45=59798 Manufacturer’s websites Abbott Nutrition home page – access to pump instruction manuals and training Videos http://www.abbottnutritionuk.com/ Corpak Medsystems – access to information about enteral tubes and company guidelines http://corpakmedsystemsuk.com/ Medicina – information about enteral syringes and feeding devices http://www.medicina.co.uk/ back to index
- 23. East Cheshire NHS Trust CNSG 007 Guidelines for Insertion and Management of Nasogastric Tubes Page 23 of 172 Created by Maggie Allen, October 2010. Updated March 2015. APPENDIX 3 ALGORITHM 1 - TO CONFIRM NG POSITION FOLLOWING INSERTION AND PRIOR TO USE No Yes Yes No Yes Yes No NG TUBE ? IN POSITION ASPIRATE OBTAINED? TRY A COMBINATION OF THE FOLLOWING pH 6 OR ABOVE ? TEST ON pH PAPER See box A pH 5.5 OR LESS? ASPIRATE OBTAINED? FLUSH 20-30MLS AIR WITH A SYRINGE THEN ASPIRATE REPEAT 2-3 TIMES ALTER TUBE POSITION SLIGHTLY Aspirate is most commonly obtained when the tube is positioned between 52-60cm (mark at exit from nose) IF UNSUCCESSFUL REPEAT INSERTION OF AIR AS ABOVE ALTER POSITION OF PATIENT - TURN ONTO LEFT SIDE AND REPEAT AS ABOVE CONSIDE R COLOUR OF ASPIRATE Yellow/green stained aspirate is suggestive of bile (higher pH) IF NEW INSERTION - X-RAY (see box C) IF ROUTINE CHECK - REFER TO ALGORITHM 2 FOR INCONCLUSIVE ASPIRATE - ACTION B X-RAY CHECK See box C IF NEW INSERTION - X-RAY (see box C) REFER TO ALGORITHM 2 FOR INCONCLUSIVE ASPIRATE - ACTION C RECENT FEED IF TUBE IS IN THE LUNG REMOVE AND START AGAIN IF IN GI TRACT BUT IN INCORRECT PLACE, REPOSITION AS PER EXPERT CLINCAL GUIDANCE. Box C. X-RAY FOLLOWING INSERTION IS INDICATED FOR THE FOLLOWING HIGH RISK GROUPS: 1. Unconscious with no gag reflex (ICU protocol) 4. Difficult insertion 2. Altered anatomy e.g. known large hiatus hernia 5. Fractured base of skull 3. Testing of aspirate is inconclusive 6. Recent radiotherapy/surgery to head and neck. X-ray should not be used routinely to confirm tube position during subsequent use. If you are unable to confirm position using the above guidelines, see algorithm 2 for checking tube position following no aspirate or inconclusive pH values. When ordering X-rays, please specify ‘to check NG position’ on request form. X-rays must be checked by an appropriately trained clinician/advanced nurse practitioner. The result must be recorded in the patient’s notes. NB. High risk patients requiring X-ray following insertion should have a pH check of aspirate carried out as well, to provide a baseline for subsequent checks. Box A. HOW TO USE pH STRIPS 1. Place a small amount of aspirate onto the pH strip-avoid touching the area to be read. 2. Allow 10 seconds and compare the resulting colour with the colour chart on the pH strip container. Box B. VARIATIONS IN GASTRIC pH MAY BE CAUSED BY: 1. Medication i.e. H2 antagonists and proton pump inhibitors which inhibit or reduce acid production. PH value will be raised. 2. Bile/ Recent feed/Lung placement – less acidic, therefore will show a higher pH value. GIVE FEED, FLUID AND MEDICATION AS PRESCRIBED See box C for whether X-ray is indicated TUBE POSITION CORRECT ON X-RAY? See box C. MEDICATION See box B IF NEW INSERTION WAIT ½ - 1 HOUR AND RETRY IF NO CHANGE X-RAY (see box C) IF ROUTINE CHECK - REFER TO ALGORITHM 2 FOR INCONCLUSIVE ASPIRATE - ACTION D
- 24. East Cheshire NHS Trust CNSG 007 Guidelines for Insertion and Management of Nasogastric Tubes Page 24 of 172 Created by Maggie Allen, October 2010. Updated March 2015. ALGORITHM 2 - TO ASSIST IN CONFIRMING NG POSITION IF NO ASPIRATE OR PH VALUE INCONCLUSIVE NO ASPIRATE INCONCLUSIVE ASPIRATE (Ph GREATER THAN 5.5) - COMBINE THE FOLLOWING WITH TUBE DISPLACEMENT CHECKS. ACTION A. CHECK FOR TUBE DISPLACEMENT ACTION A. ACTION B. No No Yes No ACTION C. No ACTION D. No ACTION B. ACTION C. ACTION E. Yes HAS THE EXTERNAL LENGTH OF THE TUBE CHANGED? Check cm mark at exit from nose and compare with insertion data on monitoring charts/NG care plan. HAS THE PATIENT VOMITED? HAS THERE BEEN AN INCREASE IN THE PATIENT’S RESPIRATORY DISTRESS e.g. breathlessness, strider, cyanosis or wheezing. IS THE NG TUBE VISIBLE IN THE MOUTH? IF NO CHANGE, DOCUMENT RESULTS AND CONTINUE TO USE THE TUBE - if unsure, consult a senior/more experienced member of staff. Document decision and rationale. REPOSITION TUBE OR REMOVE AND REPLACE – repeat confirmation checks as seen in algorithm1 FLUSH A SMALL AMOUNT OF AIR THROUGH THE TUBE TO CLEAR RESIDUAL FEED/FLUID THEN RETRY MEDICATION: IF ON A PPI e.g. LANSOPRAZOLE/OMEPRAZOLE OR H2 ANTAGONIST e.g. RANITIDINE, Look at previous pH readings, if consistently high, treat as normal, if a one off, consider why. Request senior input. CONSIDER DILUTION OF GASTRIC ACID. 1. RECENT FEED/FLUSH: WAIT HALF AN HOUR AND RETRY 2. CONTINUOUS FEEDS: CONSIDER STOPPING THE FEED FOR HALF AN HOUR. CAUTION: If the patient is having insulin infusions for tight glycaemic control . Consult with senior doctor/specialist before stopping the feed. IF REMAIN UNSURE AFTER THE ABOVE, CONSIDER X-RAY. Consult a senior/more experienced member of staff prior to requesting an X-ray. Document decision and rationale. HAS THE MARK AT THE EXIT FROM THE NOSE SLIPPED? CONSIDER THE VOLUME OF ASPIRATE: LARGE VOLUMES SUGGEST GASTRIC PLACEMENT. CAUTION: There have been reported high volumes of aspirates from tubes that have been located in the lungs. Request senior input. CONSIDER THE COLOUR OF ASPIRATE: YELLOW/YELLOWY-GREEN/DARK GREEN ASPIRATE IS SUGGESTIVE OF BILE. CAUTION: Lung aspirates shave been described as the above colours. Look at previous pH readings, if consistently high, treat as normal, if a one off, consider why. Request senior input.
- 25. East Cheshire NHS Trust CNSG 007 Guidelines for Insertion and Management of Nasogastric Tubes Page 25 of 172 Created by Maggie Allen, October 2010. Updated March 2015. APPENDIX 4: FLOW CHART TO GUIDE DECISION MAKING FOR TUBE FEEDING ROUTE back to index PEG/nasal bridle contraindicated or refused by patient If for oral feeding, refer to SALT for safe feeding techniques and to dietetics for maximising calorific value of meals. Consider referral for: - PEG feeding (see Trust PEG guidelines) Start NG feeding if appropriate whilst waiting for PEG insertion. NG tube with nasal bridle (see Trust nasal bridle guidelines) . Enteral tube feeding support required (see indications section 2.0) Confused and pulling out NGT (see flowchart to manage repeated unplanned removal of NG tubes) If for NG feeding organise MDT assessment prior to discharge to plan:- Care requirements in community Who will provide care Training required to minimise risks Agree action plan if NGT comes out Refer to section 15.0 above Consider: - Referral for radiologically inserted gastrostomy (RIG) (see section 12.0 of Trust PEG guidelines) Continuing NG feeding +/- nasal bridle (unless contraindicated or refused by patient) Limited oral feeding with palliative care Risk/benefit assessment required as to best modality for patient plus patient choice where possible If for oral feeding repossible Short term requirementLong term requirement – more than 6 weeks Yes If for palliative care, organise MDT to discuss plan of care and refer to relevant healthcare professionals. Assess for risk and appropriateness of nasogastric tube (NGT) No Refer to specialist/expert practitioner for insertion and management advice Insert NGT as per Trust guidelines HIGH RISK of complication Yes
- 26. East Cheshire NHS Trust CNSG 007 Guidelines for Insertion and Management of Nasogastric Tubes Page 26 of 172 Created by Maggie Allen, October 2010. Updated March 2015. END OF EAST CHESHIRE NHS TRUST CNSG 007 GUIDELINES FOR INSERTION AND MANAGEMENT OF NASOGASTRIC TUBES back to index back to main index
- 27. East Cheshire NHS Trust CNSG 008 Guidelines for Insertion and Management of Nasal Bridles Page 27 of 172 Created by Maggie Allen, October 2010. Updated July 2015. Guideline Title: Guidelines for Insertion and Management of Nasal Bridles Executive Summary: To optimise the care of adult in-patients receiving nutrition via a nasogastric tube under the care of East Cheshire NHS Trust. Supersedes: Version 1.1 Description of Amendment(s): Guidelines reviewed - no major changes This guideline will impact on: All staff caring for adult inpatients under the care of East Cheshire NHS Trust. Financial Implications: Improvements in nutritional care should reduce costs and risks associated with sub-optimal patient nutrition. Guideline Area: Nutrition Document Reference: CNSG 008 Version Number: 1.2 Effective Date: August 2011 Issued By: Departments of Dietetics and Gastroenterology Review Date: June 2017 Author: Maggie Allen GI Nurse Specialist Impact Assessment Date: August 2014 APPROVAL RECORD Committees / Group Date Consultation: Departments of Dietetics and Gastroenterology Clinical Nutrition Steering Group October 2010-August 2011 June 2015 Approved by: Clinical Nutrition Steering Group July 2015 AMENDMENT RECORDS August 2011 Guidelines updated for NPSA/2011/PSA002 alert compliance
- 28. East Cheshire NHS Trust CNSG 008 Guidelines for Insertion and Management of Nasal Bridles Page 28 of 172 Created by Maggie Allen, October 2010. Updated July 2015. GUIDELINES FOR INSERTION AND MANAGEMENT OF NASAL BRIDLES INDEX Back to main index SECTION CONTENTS PAGE 1.0 Introduction 29 2.0 Definition 29 3.0 Indications 29 4.0 Contraindications 29 5.0 Assessment and referral 30 6.0 Consent 30 7.0 Equipment 30 8.0 Procedure 30 9.0 Potential complications 31 10.0 Aftercare 31 11.0 Discharge with a nasal bridle in situ 31 12.0 Displacement within the community 31 13.0 Planned Removal 31 14.0 Disposal 31 15.0 References 32 Appendix 1 Flow chart to manage repeated unplanned removal of a nasogastric tube 33 Appendix 2 Nasal Bridle Fixation device request form 34 Appendix 3 Flow chart to guide management if nasogastric tube or nasal bridle displaced 35 Appendix 4 Links to supporting documents/information Patient information NPSA alerts relating to NG use Manufacturer’s websites 36
- 29. East Cheshire NHS Trust CNSG 008 Guidelines for Insertion and Management of Nasal Bridles Page 29 of 172 Created by Maggie Allen, October 2010. Updated July 2015. The following guidelines should be used in association CNSG 007 Guidelines for the Insertion and Management of Nasogastric Tubes. 1.0 Introduction back to index Nasogastric feeding is the most common method of providing short-term artificial nutritional support in the acute setting. There is a high risk of accidental removal either by the patient or by staff caring for the patient. Unplanned removal impacts in the following ways: - The patient does not meet their nutritional and fluid requirements The patient requires another tube placing Increased incidence of chest x-rays. 2.0 Definition back to index A nasal bridle is the positioning of a tape around the nasal septum to secure a nasogastric tube where it exits the nostril. If required, the bridle can remain in place for the duration of nasogastric feeding. The use of a nasal bridle to secure a nasogastric feeding tube was first described in 1980 and has since been demonstrated to be safe and effective (Donaldson et al 2007). The aim of a nasal bridle is to: - Prevent unplanned removal by patients and staff caring for the patient. Eliminate inappropriate gastrostomy insertion and associated risks. Maintain nutritional intake. Allow time for assessment as to the best method of nutritional support for a patient. 3.0 Indications back to index Patients who require delivery of medication/feed/fluid via the enteral route with the following criteria: - Poor tolerance of the nasogastric tube i.e. pulled out on at least 3 occasions in short succession. Sub optimal nasal fixation tape as a result excessive moisture e.g. patient receiving humidified oxygen therapy (tube displaced on at least 3 occasions as a result of this). Skin irritation caused by adhesive securing tape. Long term nasogastric feeding required if gastrostomy insertion inappropriate. Known difficult insertion procedure involving videofluroscopy or endoscopic insertion 4.0 Contraindications back to index Patients excluded from nasal bridle placement include: Severely agitated patients who are likely to cause damage to their nasal septum due to excessive pulling on the tube. Facial or cranial trauma. Basal skull fracture. Severely deviated, structural deformity, or obstructed nasal septum or passage. Nasotracheal tubes in situ. Advanced dementia (as well as being highly likely to pull on the tube due to confusion, these individuals may not benefit from enteral nutrition support – see CNSG 009 Guidelines for Insertion and Management of Gastrostomy Tubes for further guidance). Thrombolytic therapy for acute stroke or MI in the last 5 days (relative - discuss with consultant) Warfarin therapy (relative - discuss with consultant) Recent radiotherapy to the nose
- 30. East Cheshire NHS Trust CNSG 008 Guidelines for Insertion and Management of Nasal Bridles Page 30 of 172 Created by Maggie Allen, October 2010. Updated July 2015. 5.0 Assessment and Referral back to index If the patient is pulling out a nasogastric tube, try to identify the cause Rule out medical reasons for confusion such as infection, dehydration. The decision to place a nasal bridle should be within an MDT setting The patient should be referred to an appropriately trained doctor or nurse for assessment and insertion of the nasal bridle. See appendix 1 for flowchart for recommended management plan. 6.0 Consent back to index Informed consent must be obtained from the patient prior to the procedure as per Trust policy. The consent must be recorded in the patient’s notes. If the patient lacks capacity for consent, the decision to treat must be made within the patient’s best interests. The goals of the treatment should be clearly identified in the patient’s medical notes. The procedure should also be discussed with the family where appropriate. 7.0 Equipment AMT nasal bridle - kept on ETU/Ward 3/Ward 11 Nasogastric tube insertion equipment (Refer to CNSG 007 Guidelines for the Management of Nasogastric Tubes). 8.0 Procedure back to index The bridle must be inserted by an appropriately trained doctor or nurse. The patient should be prepared as per CNSG 007 Guidelines for the Management of Nasogastric Tubes) and a nasogastric care plan completed. The nasogastric tube must be inserted and the position checked prior to insertion of the bridle. National Patient Safety Agency Alert 19 guidance must be observed when assessing the tube’s position (www.npsa.nhs.uk) Also refer to CNSG 007 Guidelines for the Management of Nasogastric Tubes. Insert bridle following manufacture’s guidelines. Follow link http://www.appliedmedical.net/amtbridle.htm for pictorial guidelines and link http://www.appliedmedical.net/bridleVideo/bridleVideosWindow.htm for a video of the procedure (click on the appropriate tube French size directions for use). When finished, dispose of clinical waste and wash hands as per Trust policy. back to index
- 31. East Cheshire NHS Trust CNSG 008 Guidelines for Insertion and Management of Nasal Bridles Page 31 of 172 Created by Maggie Allen, October 2010. Updated July 2015. 9.0 Potential complications back to index Anterior epistaxis Bleeding may occur during insertion of a nasal bridle device. Any bleeding lasting longer than 15 minutes or greater than 100mls should be discussed with the medical team. Pressure necrosis If the nasal bridle is fastened too tightly or becomes twisted, pressure sores may lead to necrosis of the nasal septum. If a pressure sore develops, the bridle tape should be cut and removed (see section 13.0 below). The area should be checked, cleaned daily and a dressing applied where indicated. The condition of the patient’s nostrils should be recorded daily in the patient’s care plan. Dislodged Nasogastric tubes It is still possible for a tube to become dislodged despite a bridle, either deliberately by the patient or accidentally during vomiting. The tube position must continue to be checked prior to each episode of use as per CNSG 007 Guidelines for the Management of Nasogastric Tubes. 10.0 Aftercare back to index The patient should be monitored as per CNSG 007 Guidelines for the Management of Nasogastric Tubes. In addition, the patient should be monitored closely for signs of nasal trauma as a result of the patient pulling on the tube, or irritation caused by the tape rubbing against the nasal passage. The nasal passage and tape should be cleaned daily. 11.0 Discharge with a nasal bridle in situ If the patient is to be discharged with a bridle in situ the following should be in place: - A written care plan provided for carers. Plan of action if the tube becomes displaced. Support from dietetics to continue with nutritional monitoring. 12.0 Displacement within the community back to index District nurses or out of hours nurses should be contacted to assess whether the patient needs to attend the A&E department. 13.0 Planned removal Cut one side of the tape (usually the side exiting the nostril opposite the nasogastric tube) and pull the nasogastric tube out. The tape will follow with the tube. See video link for a demonstration. http://www.appliedmedical.net/bridleVideo/bridleVideosWindow.htm 14.0 Disposal The tube and bridle should be disposed of as per East Cheshire NHS Trust policy for disposal of clinical waste. back to index
- 32. East Cheshire NHS Trust CNSG 008 Guidelines for Insertion and Management of Nasal Bridles Page 32 of 172 Created by Maggie Allen, October 2010. Updated July 2015. 15.0 References back to index Donaldson, E., Early, T., Sheilds, P (2007) The Nasal Bridle – It’s place within an integrated nutrition service: a prospective audit of one year’s data. Gut (56) Suppl 56 A137 Johnston RD et al. (2008). Outcome of patients fed via a nasogastric tube retained with a bridle loop: do bridle loops reduce the requirement for percutaneous endoscopic gastrostomy insertion and 30-day mortality? Proceedings of the Nutrition Society 67, E116. Lancashire Teaching Hospitals NHS Trust (2006). Safe practice for insertion and management of a nasal bridle to secure nasogastric tubes. National Institute for Clinical Excellence (NICE) (2006) Nutrition Support in Adults: oral supplements, parenteral and enteral feeding. London. http://www.nice.org.uk/nicemedia/live/10978/29981/29981.pdf Russell KL et al. (2006). Bridle fixation of nasogastric tubes – the Addenbrooke’s experience. Proceedings of the Nutrition Society 65, 14A. Popovich MJ et al. (1996). Nasal bridle revisited: An improvement in the technique to prevent unintentional removal of small-bore nasoenteric feeding tubes. Critical Care Medicine 24, 429-431. back to index
- 33. East Cheshire NHS Trust CNSG 008 Guidelines for Insertion and Management of Nasal Bridles Page 33 of 172 Created by Maggie Allen, October 2010. Updated July 2015. APPENDIX 1. back to index FLOW CHART TO MANAGE REPEATED UNPLANNED REMOVAL OF A NASOGASTRIC TUBE back to index back to NG guidelines Patient pulled out NG tube on more than three occasions Is the patient confused?Yes No Establish reason for confusion and treat accordingly Reassess for a nasal bridle. MDT discussion to discuss appropriateness. To include Doctor/nurse/SALT/dietitian Wait 24 hours Identify why the patient is pulling the tube out. If the patient refuses the tube, they should have the risks and consequences explained to them so that they can make an informed choice. Doctor/specialist nurse to discuss the procedure, pros and cons with the patient/relatives and obtain consent. Document consent in medical notes Insert NG tube and check tube position as per Trust guidelines prior to inserting the bridle as per manufacturer’s guidelines http://www.appliedmedical.net/bridleVideo/br idleVideosWindow.htm Monitor for complications. Refer to flow chart to guide management if displacement of nasal bridle/tube. Refer to flow chart to guide decision making making for tube feeding route Nasal bridle to proceed Yes No
- 34. East Cheshire NHS Trust CNSG 008 Guidelines for Insertion and Management of Nasal Bridles Page 34 of 172 Created by Maggie Allen, October 2010. Updated July 2015. APPENDIX 2 Nasal Bridle Fixation Device Request Form To be used alongside the NG care plan document. Please complete all the information requested on this form. Fax the form to x1904, Gastroenterology Department. Patient Details: Name: ……………………………………………………… Hospital No:........................... Date of Birth:…………………….. Ward................................. Consultant................................................................... Is the patient NBM On NG Feed Eating orally Date of last SALT review ............................ Date of last dietetic review....................... Number of NGs pulled out by the patient?................................. Can the patient consent to the bridle Yes/No Has the bridle been discussed with the patient relatives (if appropriate) Yes/No Is the patient receiving or has had recent anticoagulation therapy Yes/No If the patient has any of the following conditions nasal bridle is not appropriate Extreme confusion and likely to pull at the tube Yes/No Known basal skull fractures Yes/No Deviated or perforated nasal septum Yes/No Structural deformity of the nose or nasopharynx Yes/No Advanced dementia Yes/No Recent radiotherapy to the nose or nasopharynx Yes/No Bridle requested by (name/title).................................................................................. Doctor’s signature................................................ Contact number.............................
- 35. East Cheshire NHS Trust CNSG 008 Guidelines for Insertion and Management of Nasal Bridles Page 35 of 172 Created by Maggie Allen, October 2010. Updated July 2015. APPENDIX 3. FLOW CHART TO GUIDE MANAGEMENT IF NASAL BRIDLE AND / OR NASOGASTRIC TUBE DISPLACED *If there is a delay for specialist/trained intervention – continue with NG therapy and monitor carefully for unplanned tube removal. Bolus administration only recommended. **Refer to flow chart to guide decision making making for tube feeding route. back to index NG still in Bridle out Review patient condition and reason for removal Yes Refer to specialist/HCP trained in the procedure for reinsertion of bridle* Check NG tube still in position prior to reinsert bridle as per Trust guidelines and secure to NG tube. If NGT also pulled out, reinsert NG tube and check position as per Trust guidelines, then secure to bridle. No Remove bridle and continue with oral diet. Bridle and NG out NG still required** Bridle still required** Reinsert NG tube as per Trust guidelines and consider whether bridle still required, if not, remove bridle. Remove NGT and continue with oral diet. NG still required** Yes No Review patient condition and reason for removal. NB. There may be damage to nasal septum if bridle removed forcefully. Bridle still required** Yes Reinsert NG tube and check position as per Trust guidelines, then secure to bridle. Yes No NG out Bridle still in No No Yes No
- 36. East Cheshire NHS Trust CNSG 008 Guidelines for Insertion and Management of Nasal Bridles Page 36 of 172 Created by Maggie Allen. October 2010. Updated July 2015. APPENDIX 4 SUPPORTING INFORMATION back to index NPSA alerts relating to Nasogastric feeding National Patient Safety Agency (2012) Harm from flushing of nasogastric tubes before confirmation of placement NPSA/2012/RRR001 22/03/12 http://www.nrls.npsa.nhs.uk/resources/type/alerts/?entryid45=133441 National Patient Safety Agency (2011) Reducing the harm caused by misplaced nasogastric feeding tubes in adults, children and infants. NPSA/2011/PSA002 http://www.nrls.npsa.nhs.uk/alerts/?entryid45=129640 National Patient Safety Agency (2007) Promoting safer measurement and administration of liquid medicines via oral and other enteral routes NPSA/2007/19 http://www.nrls.npsa.nhs.uk/alerts/?entryid45=59808 National Patient Safety Agency (2005) Reducing the harm caused by misplaced nasogastric feeding tubes NPSA/2005/05 http://www.nrls.npsa.nhs.uk/resources/type/alerts/?entryid45=59798 Manufacturer’s websites Applied Medical Technology (AMT ) nasal bridle http://www.appliedmedical.net/amtbridle.htm http://www.appliedmedical.net/bridleVideo/bridleVideosWindow.htm Abbott Nutrition home page – access to pump instruction manuals and training Videos http://www.abbottnutritionuk.com/ Corpak Medsystems – access to information about enteral tubes and company guidelines http://corpakmedsystemsuk.com/ Medicina – information about enteral syringes and feeding devices http://www.medicina.co.uk/ back to index
- 37. East Cheshire NHS Trust CNSG 008 Guidelines for Insertion and Management of Nasal Bridles Page 37 of 172 Created by Maggie Allen. October 2010. Updated July 2015. END OF EAST CHESHIRE NHS TRUST CNSG 008 GUIDELINES FOR INSERTION AND MANAGEMENT OF NASAL BRIDLES back to index back to main index
- 38. East Cheshire NHS Trust CNSG 009 Guidelines for Insertion and Management of Gastrostomy Tubes Page 38 of 172 Created by Maggie Allen. October 2010. Updated July 2015 Guideline Title: Guidelines for Insertion and Management of Gastrostomy Tubes. Executive Summary: To optimise the care of adult in-patients receiving nutrition via a gastrostomy tube under the care of East Cheshire NHS Trust. Supersedes: Version 1.0 Description of Amendment(s): Guidelines reviewed - New guidance: - Stop Clopidogrel 7 days prior to PEG insertion and to omit new anticoagulants dependent on specific anticoagulant and patient’s renal function. Updated advice on optimum positioning of gastrostomy tube. This guideline will impact on: All staff caring for adult inpatients under the care of East Cheshire NHS Trust. Financial Implications: Improvements in nutritional care should reduce costs and risks associated with sub-optimal patient nutrition. Guideline Area: Nutrition Document Reference: CNSG 009 Version Number: 1.1 Effective Date: November 2010 Issued By: Departments of Dietetics and Gastroenterology Review Date: June 2017 Author: Maggie Allen GI Nurse Specialist Impact Assessment Date: August 2014 APPROVAL RECORD Committees / Group Date Consultation: Departments of Dietetics and Gastroenterology Clinical Nutrition Steering Group Infection prevention and control October 2010 June 2015 Approved by: Clinical Nutrition Steering Group July 2015 AMENDMENTS RECORD
- 39. East Cheshire NHS Trust CNSG 009 Guidelines for Insertion and Management of Gastrostomy Tubes Page 39 of 172 Created by Maggie Allen October 2010. Updated July 2015. GUIDELINES FOR INSERTION AND MANAGEMENT OF GASTROSTOMY TUBES INDEX SECTION CONTENTS PAGE 1.0 Definition 41 2.0 Indications 41 3.0 Contraindications 42 3.1 Advanced dementia 42 4.0 Referral 43 5.0 Information giving and informed consent 43 5.1 Capacity and consent 43-4 5.2 Multidisciplinary team 44 6.0 Preparation and Assessment 45-7 6.1 Type of tube 47 7.0 Patient care post gastrostomy insertion 48 7.1 Peri and postoperative complications of PEG insertion 48 7.2 Monitoring 48 7.3 Commencing feed/oral diet 49 7.4 Mouth care 49 7.5 Pain control 49 7.6 Gastrostomy site care 50 7.6.1 Procedure to clean a gastrostomy site 50 7.6.2 Bathing and showering 51 7.6.3 Gastrostomy site dressings 51 7.6.4 Positioning the fixation device 51 7.6.5 Prevention of buried bumper syndrome 51 7.6.6 Sutures 52 8.0 Maintenance of the gastrostomy tube 52 8.1 Flushing 52 8.2 Syringes 52 8.3 General maintenance of the tube 52 9.0 Removal of a gastrostomy tube 53 9.1 Accidental removal 53 9.2 Planned removal 53 9.3 Procedure for traction removal of a Merck Corflo gastrostomy tube 53-4 10.0 Management of balloon gastrostomy tubes 54 10.1 Definition 54 10.2 Low profile gastrostomy tubes – buttons 54 10.3 General management of balloon gastrostomy tubes, buttons and extension sets 54-5 10.3.1 Preparation of an extension set for administering fluids via a low profile device 55 10.3.2 Cleaning an extension set after use and replacement 55 10.4 Checking the balloon volume 56 10.5 Removal of a balloon gastrostomy tube 57 10.6 Discontinuing balloon gastrostomy feeding 58 10.7 Replacement of a balloon gastrostomy tube 58 Back to main index
- 40. East Cheshire NHS Trust CNSG 009 Guidelines for Insertion and Management of Gastrostomy Tubes Page 40 of 172 Created by Maggie Allen October 2010. Updated July 2015. INDEX CONTINUED SECTION CONTENTS PAGE 10.8 Insertion procedure for a balloon gastrostomy tube 58-60 10.9 Insertion of a low profile device 60 10.10 Measurement of a gastrostomy stoma 60 10.11 Complications 60 10.12 Accidental removal of gastrostomy tube 61 10.13 Temporary gastrostomy tubes 62 10.14 Spare tubes 62 11.0 Management of an intestinal tube within a PEG tube for buried bumper 63 11.1 Insertion/replacement of an intestinal tube within a PEG tube 63-4 11.2 Care of an intestinal tube within a PEG tube 64 12.0 Radiologically inserted gastrostomy tubes (RIG) 65 12.1 Referrals 65 12.1 Sutures 65 13.0 Discontinuation of tube feeding 65 14.0 Discharge of patients on enteral feeding 65-6 14.1 Discharge within 72 hours of PEG insertion 65 14.2 Information required for discharge within 72 hours of insertion 66 14.3 Training required prior to discharge 66 14.4 Information and contact details required prior to discharge 66 14.5 Referrals required prior to discharge 66 14.6 Equipment required for discharge 66 Appendix 1 References and bibliography 67 Appendix 2 Linked supporting documents: - Discharge check list Patient information NPSA alerts relating to PEG Manufacturer’s information Care Pathway for Percutaneous Endoscopic Gastrostomy (PEG) Tubes 68 Back to main index
- 41. East Cheshire NHS Trust CNSG 009 Guidelines for Insertion and Management of Gastrostomy Tubes Page 41 of 172 Created by Maggie Allen October 2010. Updated July 2015. 1.0 DEFINITION back to index A gastrostomy tube is the generic term for a feeding tube that is inserted into the stomach either, surgically, endoscopically (PEG) or radiologically (RIG). The gastrostomy tube allows delivery of nutrients, fluid and medication directly into the stomach. Percutaneous Endoscopic Gastrostomy (PEG) is the insertion of a small plastic tube through the abdomen and into the stomach under endoscopic vision. The following guidelines are biased towards this type of procedure as radiological insertion of a gastrostomy (RIG) is not currently undertaken at the Trust. 2.0 INDICATIONS back to index When selecting patients for gastrostomy/PEG insertion the following should be considered: Artificial nutrition is appropriate for the individual Patients require enteral nutritional and hydration support (partial or complete) for more than 6 weeks. The individual has a functional gastrointestinal tract. Nasogastric (NG) tube feeding has not been tolerated or is thought to be unsafe. - The patient has pulled out the NG tube on at least 3 occasions in short succession and use of a nasal bridle is contraindicated. Refer to CNSG 008 guidelines for management of nasal bridles for further information. - The patient demonstrates significant distress during NG insertion. - The patient refuses nasogastric tube insertion. - Altered anatomy e.g. large hiatus hernia, increasing the risk of aspiration. - Basal skull fracture, as the tube may enter the brain if incorrectly positioned (oro-gastric positioning may be appropriate). - Obstructive pathology in oropharynx or oesophagus preventing passage of the tube e.g. stricture, tumour. The patient is fit enough and will benefit from the procedure back to index - Procedure related mortality 0.7-2%. - 30-day mortality rate 2-28% - Complications post PEG 15-70% (NCEPOD 2004 and BSG Guidelines 2006) http://www.bsg.org.uk/images/stories/docs/clinical/guidelines/endoscopy/complicati ons.pdf http://www.ncepod.org.uk/2004report/index.htm High risk groups include individuals with significant co-morbidity, in particular those with aspiration pneumonia prior to PEG insertion. See section 6 below for further information. Tolerance of the gastrostomy tube by patient/partner. - Physical implications – changes to body image, foreign object in body, feel unable undertake activities such as swimming. Psychological implications - changes to body image which may affect the individual and their partner, unable to engage in normal social activity such as eating, regular interference with the body by others accessing the gastrostomy tube to deliver feed and fluids. back to index
- 42. East Cheshire NHS Trust CNSG 009 Guidelines for Insertion and Management of Gastrostomy Tubes Page 42 of 172 Created by Maggie Allen October 2010. Updated July 2015. 3.0 CONTRAINDICATIONS back to index Table 1 Absolute Relative Tense ascites Peritoneal dialysis Total gastric outflow obstruction Morbid obesity Treatment with high dose steroids Previous upper GI surgery Partial gastric outflow obstruction Advanced dementia (see below) Coagulopathy disease/drugs Gastro-oesophageal reflux with risk of aspiration Recurrent aspiration pneumonia due to severe dysphagia following a stoke 3.1 Advanced dementia back to index The following summary illustrates the problems faced in deciding whether a gastrostomy tube is appropriate for an individual with advanced dementia. There is insufficient evidence to suggest that enteral tube feeding is beneficial in patients with advanced dementia. Data are lacking on the adverse effects of this intervention Patients with advanced dementia often develop dysphagia (difficulties swallowing). They also experience changes in appetite and apraxia (difficulty co-coordinating movements) and may have difficulties feeding themselves. Two methods of enteral tube feeding are commonly used: the administration of food and fluids via a nasogastric tube (a tube that is passed through the nose and into the stomach) or via a percutaneous endoscopic gastrostomy (PEG) where a feeding tube is inserted into the stomach and is accessed through a permanent incision in the abdominal wall. The decision to use artificial hydration and nutrition in someone with dementia is often emotive and complex. Relatives and carers may request the intervention because they are concerned that the patient may starve; clinicians may be aware of the risks but feel pressurised by institutional, societal or even legal directives to intervene. We found no conclusive evidence that enteral tube nutrition is effective in terms of prolonging survival, improving quality of life, or leading to better nourishment or decreasing the risk of pressure sores. It may actually increase the risk of developing pneumonia due to inhaling small quantities of the feed and even death. This area is difficult to research but better designed studies are required to provide more robust evidence Sampson EL, Candy B, Jones L. Enteral tube feeding for older people with advanced dementia. Cochrane Database of Systematic Reviews 2009, Issue 2. Art. No.: CD007209. DOI: 10.1002/14651858.CD007209.pub2 Further information and guidance regarding the difficulties in providing nutrition support can be found in: Oral feeding difficulties and dilemmas. A guide to practical care, particularly towards the end of life. Report of a joint RCP/BSG Working Party - January 2010. https://www.rcplondon.ac.uk/sites/default/files/documents/oral-feeding-difficulties-and- dilemmas.pdf back to index
- 43. East Cheshire NHS Trust CNSG 009 Guidelines for Insertion and Management of Gastrostomy Tubes Page 43 of 172 Created by Maggie Allen October 2010. Updated July 2015. 4.0 REFERRAL back to index The patient should be referred to: - Gastroenterologist/Specialist nurse Dietitian Speech and language therapists (where appropriate) Independent mental capacity advocate (IMCA)(If the patient lacks capacity to make an informed decision and does not have any family or friends with whom it is ‘appropriate to consult’ about the decision – see section 5 below for further information) 5.0 INFORMATION GIVING AND INFORMED CONSENT back to index Decision-making and consent may be affected by previous experiences and/or by fear. Time should be spent explaining about gastrostomy feeding to the individual and family. They may find it useful to meet someone else with a gastrostomy tube. Information about support groups should also be offered. Key information to be discussed includes: - Full explanation of the procedure and associated complications (see section 7.1 below). Written information should also be offered (EIDO E09 PEG leaflet, accessible from the Trust front page. Click on Patient information, then EIDO link and log in following instructions. Once logged in, scroll down to Endoscopy and click on PEG, print off as required. Benefits and disadvantages of gastrostomy feeding Aftercare Major impact on lifestyle, for instance if alternative accommodation needs to be considered if the patient needs specialist care post gastrostomy. The patient’s consent should be written where possible on the Trust consent form (Form 1). If this is not possible, verbal consent should be witnessed on the Trust consent form (Form 1). Refer to East Cheshire NHS Trust consent policy for further information regarding the validity of consent. If communication is impaired, every effort should be made to communicate with the individual, including the use of drawings/props where necessary. In some cases repeated sessions to impart information may be necessary. Evidence of these conversations should be documented in the patient’s notes. Liaison with other healthcare professional e.g. speech and language therapists (SALT) may be indicated to maximise communication techniques. 5.1 Capacity and consent back to index Assessment of capacity to make informed decisions should be made prior to PEG insertion. If the individual is thought not to have capacity for informed consent, it is important to have early, sensitive discussions with relatives or individuals close to the patient, to try to determine whether the individual has previously expressed any views on the subject, or if they have a legitimate advanced decision, or have appointed a lasting power of attorney to make decisions for them, as legislated for within the Mental Capacity Act (MCA) 2005. In absence of a valid advanced decision or lasting power of attorney (welfare), the family should be reassured that the decision making is not their responsibility, but that of the clinician (Decision Maker) in charge of their relatives care, to make the decision regarding PEG based on the individual’s best interests. Under these circumstances an additional safeguard has been implemented by the Act which requires clinicians to involve an independent mental capacity advocate (IMCA) for serious medical treatment decisions when: - a best interests decision is required because the doctor has assessed the person as not having the capacity to make the decision themselves. the person does not have family or friends with whom it is ‘appropriate to consult’ about the decision.
- 44. East Cheshire NHS Trust CNSG 009 Guidelines for Insertion and Management of Gastrostomy Tubes Page 44 of 172 Created by Maggie Allen October 2010. Updated July 2015. Serious medical treatment is defined in the Mental Capacity Act 2005 (Independent Mental Capacity Advocates) (General) Regulations 2006 as treatment which involves providing, withdrawing or withholding treatment in circumstances where one or more of the following apply: in a case where a single treatment is being proposed, there is a fine balance between its benefits to the patient and the burdens and risks it is likely to entail for them in a case where there is a choice of treatments, a decision as to which one to use is finely balanced what is proposed would be likely to involve serious consequences for the patient. The MCA Code of Practice states that ‘serious consequences’ may include treatment options which: cause serious and prolonged pain, distress or side effects have potentially major consequences for the patient (for example, major surgery or stopping life-sustaining treatment) have a serious impact on the patient’s future life choices. back to index Patients who have been referred for PEG and lack capacity for decision making and do not have any family or friends with whom it is ‘appropriate to consult’ about the decision, should be referred to an IMCA as they fall within several of the above criteria. The IMCA ensures that the Decision Maker (clinician) considers what the wishes and beliefs of that person would be when deciding what course of action to take. This is done by questioning all the people involved with that person, investigating the medical condition and treatment options and making recommendations based on these findings. This statutory IMCA service is provided by qualified Independent Mental Capacity Advocates. For further information please contact East Cheshire Advocacy on: Tel. 01625 534889 Online. www.ecadvocacy.co.uk Email: admin@ecadvocacy.co.uk East Cheshire Advocacy, 81 Park Lane, Macclesfield, SK11 6TX. If an individual is assessed as lacking capacity to give informed consent, the ‘Form for adults who are unable to consent to investigation or treatment’ (Consent Form Four) should be completed. The form should be signed by the clinician in charge of care, the clinician undertaking the procedure and the patient’s family/carers to indicate that they have been involved in the discussion process. If the family are unable to sign the form, there should be documented evidence in the patient’s medical notes regarding the discussion process. 5.2 Multidisciplinary team (MDT) approach back to index For patients who lack capacity to make an informed choice, there are potentially difficult ethical decisions to be made. Each patient considered for PEG feeding should be assessed on his or her own merits. They may not fall within the above criteria. The decision should be made within an MDT approach and based on the patient’s best interests. The team should consist of healthcare professionals involved with the patient, e.g. speech and language therapist, dietitian, doctor (including GP if appropriate), nurse (ward level and specialist), physiotherapist, occupational therapist, social worker, community carers. Where the situation is particularly complex, or the MDT decision is equivocal, consider referral to the palliative care consultant.
- 45. East Cheshire NHS Trust CNSG 009 Guidelines for Insertion and Management of Gastrostomy Tubes Page 45 of 172 Created by Maggie Allen October 2010. Updated July 2015. 6.0 PREPARATION AND ASSESSMENT PRIOR TO PEG back to index Clinical assessment In addition to assessing for contraindications, the following should be considered: - Table 2 CONDITION RATIONALE Relevant co-morbidity Increases risk of complications during or post PEG insertion. Infection prior to PEG Increases risk of complications during or post PEG insertion. If patient is MRSA positive –follow MRSA Trust policy. In relation to antibiotics/treatment refer to Trust antibiotic policy, contact the IPCT and/or the Microbiologist. Cervical/Neck problems May affect positioning during PEG insertion. Tracheostomy Requires specialist support and suctioning during the procedure. Previous abdominal surgery Altered anatomy and adhesion increases the risk of bowel perforation. Respiratory condition Known aspiration pneumonia or respiratory problems prior to the procedure carries an increased risk of fatality post procedure. Local audit 2001-2004 indicated that 66% of patients diagnosed with aspiration pneumonia prior to PEG insertion, died within 30 days of the procedure. Allergies Ensure the patient is prepared safely for the procedure. Unable to open mouth/ poor dentition Increased risk of damage to teeth during endoscopy. Poor dentition will increase the amount of bacteria in the mouth which if aspirated will result in an increased risk of respiratory infection. Referral to a dentist may be required. Coagulopathy PEG is contra-indicated if INR >1.3 Severely malnourished patients may have a vitamin K deficiency which will need correcting prior to PEG. Anticoagulant therapy PEG is contra-indicated if INR >1.3 Anticoagulants need to be stopped prior to PEG See below. Severely malnourished - risk of re-feeding syndrome Increased risk of electrolyte imbalance once feeding starts. Thrombocytopenia PEG is contra-indicated if platelet count <100 Low platelet count causes increased risk of peri- procedural bleeding. back to index
- 46. East Cheshire NHS Trust CNSG 009 Guidelines for Insertion and Management of Gastrostomy Tubes Page 46 of 172 Created by Maggie Allen October 2010. Updated July 2015. 6.0 PREPARATION continued back to index Preparation Action Bloods FBC If platelet count <100 consider correcting with 1 -2 units of platelets within 4 hours of the procedure. INR If INR > 1.3: Correct and recheck U& Es inc calcium group, phosphate and magnesium and levels Correct any electrolyte disturbances before commencing nutritional support. Re-feeding drugs, if required, should be prescribed according to CNSG Guidelines for Re-feeding management. Review medication Anticoagulants PEG is classified as a high risk procedure with regards to risk of bleeding and anticoagulation therapy. NB. Some anticoagulants need stopping up to 7 days prior to PEG e.g Clopidogrel 7 days, Warfarin 5 days. New anticoagulants - the stoppage time will depend on the particular anticoagulant and the patient’s renal function. Alternative anticoagulation therapy may be required depending on the patient’s medical condition. Check with gastroenterology/haematology team for further advice. Current drug therapy Refer to pharmacist as the patient’s drug formulations may need to be changed. Timing and dosage of drug administration may need to be altered due to altered drug formulation and/or potential interaction with feed, particularly in the drug has a narrow therapeutic index. Refer to CNSG 016 Guidelines for Administration of Medication via Enteral Feeding Tubes. Medication required Prophylactic antibiotics Patients should have a single dose of intravenous Co- amoxiclav 1.2g, just before the procedure. British Society of Gastroenterology (BSG) 2009. Antibiotic prophylaxis in gastrointestinal endoscopy. If penicillin allergic, give a single dose of Gentamicin 3mg/kg (max 300mg), just before the procedure (maximum of 1 hour). If MRSA discuss with microbiologist. MRSA eradication therapy (if known MRSA colonisation or infection) If the patient is MRSA positive contact the IPCT/Microbiologist for advice regarding suppression therapy prior to insertion (as per Trust MRSA policy). If antibiotics are required, they should be prescribed as per Trust antibiotic policy. Analgesia Prescribe prn soluble oral and IM analgesia for pain post PEG insertion (arrange for a take home prescription if for discharge post PEG). Feed Doctor/dietitian to write up feed on prescription chart and feeding regimen. Corsodyl mouthwash (chlorhexidine gluconate 0.2%) To start 48 hours prior to procedure. Aim to reduce bacterial load in mouth, as the tube is pulled though the mouth and into the newly formed stoma. back to index
- 47. East Cheshire NHS Trust CNSG 009 Guidelines for Insertion and Management of Gastrostomy Tubes Page 47 of 172 Created by Maggie Allen October 2010. Updated July 2015. 6.0 PREPARATION continued back to index Preparation Action Weight A baseline and regular weight is required in order to: - accurately assess nutritional and fluid requirements assess weight following PEG insertion (barometer of the patient’s nutritional requirements and monitors for potential fluid overload). Fasting Fasting (mouth and tube) 6 hours prior to procedure. Hygiene Full wash Clean theatre gown Clean sheets. Venous access Must be established before the patient arrives on the Endoscopy Unit (except for outpatients). Mouth Care Regular mouth care required with Corsodyl mouthwash - to reduce risk of stoma infection. The mouth must be clear of dried secretions prior to PEG insertion. There is an increased risk of stoma infection if the mouth is not clean at the time of PEG insertion. If mouth care is difficult, inform specialist nurse. Advise endoscopy staff of loose/broken teeth. Equipment required Pump, giving sets, oral/enteral syringes, recommended feed, sterile water for first flush, tap water for subsequent flushes. Subcutaneous fluids Avoid siting the butterfly cannula in the upper central abdomen as this can result in skin infections or abscesses that may affect PEG insertion. (Insertion of sub cut cannula must be done using aseptic technique). Documentation required The following documents must be sent with the patient to the endoscopy unit at the time of the procedure: Signed consent form Patient notes Nursing Kardex Drug charts Completed PEG pathway (Click for link) 6.1 Type of tube back to index The tube of choice at East Cheshire NHS Trust is a Merck Corflo traction removable tube. It is available in 12Fr, 16Fr and 20Fr sizes. Most patients have a 16Fr tube inserted. Other sizes may be used depending on the patient’s requirements. The most appropriate type of tube and size will be decided at the time of assessment. Greater than 16Fr tubes should be avoided due to increased risk of stoma leakage.
- 48. East Cheshire NHS Trust CNSG 009 Guidelines for Insertion and Management of Gastrostomy Tubes Page 48 of 172 Created by Maggie Allen October 2010. Updated July 2015. 7.0 PATIENT CARE POST PEG INSERTION back to index 7.1 PERI AND POST PROCEDURAL COMPLICATIONS ASSOCIATED WITH PEG Perforation Haemorrhage Sepsis Peritonitis Respiratory depression due to sedation Pulmonary aspiration Peristomal site infection Ischaemic pressure necrosis Gastrocolic fistulae Tube blockage Accidental displacement of the PEG Monitor patient post PEG for development of complications and report promptly. Link to management of suspected peritonitis Link to flow chart for complications post PEG and management 7.2 MONITORING back to index Observations Half hourly for a minimum of 2 hours. o Blood pressure, pulse and temperature o Oxygen saturation and respiratory rate o Wound check o Pain assessment o PEG position unchanged Hourly for a minimum of 2 hours. o As per half hourly assessments 2 - 4 hourly (depending on clinical status). o As per half hourly assessments Discontinue as clinical condition allows Bloods Repeat full profile if at risk of re-feeding syndrome. See CNSG re-feeding guidelines or contact the dietitian. Repeat U& Es. Refer to CNSG Guidelines for Assessment and Monitoring for further guidance. Contact dietitian for information. back to index Bowels Document and monitor bowel movements Consider aperients if constipated NB. Constipation presents serious hazard for a patient following PEG insertion. A build up of pressure within the abdomen may increase the risk of leakage from the stomach into the peritoneal cavity with subsequent peritonitis. There is also an increased risk of vomiting which places the patient at greater risk of aspiration, particularly if they have an unsafe swallow. Weight As requested by dietitian. back to index