Twin pregnancy.pptx
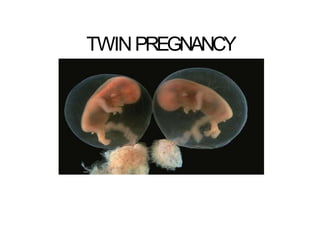
- 2. INTRODUCTION • 1% of all pregnancies • Over 97% of all multiple pregnancies are twin pregnancies (Joseph 1998). • Associated with increased perinatal mortality & morbidity • Results from ovulation & fertilization of > 1 oocyte OR splitting of 1 embryonic mass to form 2 genetically identical fetus • Since 1970, the prevalence of multiple births has been increasing because of more widespread use of ART.
- 3. INCIDENCE Hellin’s law Twin 1 : 80 Triplets 1 : 802 Quadruplets 1:803 Quniplets 1:804 Frequency of twins : highest – black race, lowest – orientals Increase with maternal age and parity Increase with ART
- 4. TERMS Zygosity refers to the type of conception Two thirds of all twins are dizygotic. Chorionicity denotes the type of placentation. *Chorionicity rather than zygosity determines outcome.
- 5. TWINS DIZYGOTIC 2/3 MONOZYGOTIC 1/3 Monochorionic monoamniotic <1% Monochorionic diamniotic -75% Dichorionic diamniotic -25% Dichorionic Diamniotic
- 7. DIZYGOTIC • Fertilization of 2 separate ova
- 8. DIZYGOTIC • incidence of dizygotic twins varieswith –ethnic group - up to 5 times higher in certain parts of Africa and half ashighin parts ofAsia –maternal age - 3 in 1000 births in women younger than 20,14 in 1000 births in women aged 35-40 y –Parity - 2%after four pregnancies –method of conception - 20%withovulation induction.
- 9. MONOZYGOTIC • Also known as identical twins. • 1/3 of twin. • Fertilization of single ovum • Similar sex • Identical in every way including HLA genes • Not genetically determined • Its prevalence 1/250
- 10. THE OUTCOME OF TWINNING PROCESS DEPENDS ON WHEN THE DIVISION OCCUR monochorionic *Division after 13 days Conjoined twin
- 12. ZYGOSITYAND CHORIONICITY • Zygosity - determined by DNAfingerprinting. – require an invasive procedure – amniocentesis, chorionic villus sampling orcordocentesis • Chorionicity - determined by USS(fetal gender,number of placentas and characteristics of the membrane betweenthe two amnioticsacs). – Different-sex twins =dizygotic anddichorionic, – but in 2/3 of twin pregnancies the fetuses same sexand these may be either monozygotic ordizygotic. – Twoseparate placentas=dichorionic – but, iftwo placentas are adjacent to each other and therefore difficult to distinguish betweendichorionic- fused and monochorionic placentas.
- 13. ZYGOSITYAND CHORIONICITY • Thebest way to determinechorionicity ultrasound examination at 10-14 weeksof gestation • Lambda sign-Dichorionic • T-sign - Monochorionic
- 17. DIAGNOSIS OF MULTIPLE PREGNANCY History : h/o IVF, taking ovulation inducing drugs Symptoms Early pregnancy : excessive nausea, vomiting, Abnormal bleeding Mid pregnancy : excessive weight gain, uterus larger than date Late pregnancy : pressure symptoms – dyspnea, dyspepsia Signs : Anemia, edema, high BP, abnormal weight gain Uterus larger than date Multiple fetal poles felt 2 distinct FH heard Ix : confirm by Ultrasound Detect 99% of multiple gestation before 26 weeks Confirms fetal viability Diagnose type Confirm fetal numbers.
- 18. Patientcare • Ultrasound at 10–14 weeks: (a) viability; (b) chorionicity; (c) NT : aneuploidy • Structural anomaly scanat 20–22 weeks. • Serial fetal growth scanse.g24, 28, 32 and then two- to four- weekly. • 34–36 weeks: discussion of mode of delivery and intrapartumcare. • Elective delivery at 37–38 completed weeks.Someby 40weeks • Postnatal advice and support (hospital- andcommunity-based) to include breastfeeding and contraceptive advice Dichorionic twins Monochorionic twins • Ultrasound at 10–14 weeks: (a) viability; (b) chorionicity; (c) NT : aneuploidy/TTTS • Ultrasound surveillance forTTTS and discordant growth: at 16 weeksand then two-weekly. • Structural anomaly scanat 20–22 weeks(including fetal ECHO). • Fetal growth scansat two-weekly intervals until delivery. • 32–34 weeks: discussionof mode of delivery and intrapartumcare. • Elective delivery at 36–37 completed weeks(if uncomplicated). • Postnatal advice and support (hospital- and community-based) to include breastfeeding and contraceptive advice.
- 19. At what age should genetic testing be offered to a mother with dichorionic and monochorionic twins? • All women carrying twin pregnancies should be referred for counselling to a centre for the consideration of invasive testing at age 32. • The counselling must be individualized and the final decision must be taken by the parents since the risk of amniocentesis is uncertain in twin gestation. ―Thechance of a 32 year old woman who carries twins of unknown zygosity having at least one child with Down syndrome is equivalent to the risks of a 35 year old with a singleton pregnancy.‖
- 20. METHODS AVAILABLE FOR GENETIC SCREENING IN TWIN PREGNANCIES • Biochemical screening for aneuploidy is not recommended in twins. • Maternal serum alpha fetoprotein (MS-AFP) is useful for detection of open neural tube and other birth defects. • Evidence is promising that nuchal translucency (NT) screening is useful for identifying twin pregnancies at high risk of aneuploidy. • The fetal loss rates with invasive testing (amniocentesis and chorionic villus sampling (CVS)) in twins are unclear. • Invasive testing should be offered to twins according to the usual standard of care.
- 21. HOSPITAL BEDREST • Randomized controlled trials and a meta- analysis of hospital bedrest in twin pregnancies have shown no reduction in preterm birth or perinatal death. • In uncomplicated twin pregnancies, hospital rest may result in increased risk of very preterm birth and maternal psychosocial stress. • In women with twin pregnancy at high risk for preterm birth because of premature cervical change prior to labour, there is no evidence that hospital bedrest will reduce the rate of preterm birth.
- 22. ACTIVITY RESTRICTION/WORK LEAVE • Restriction of activity level and the recommendation to stop work is commonly prescribed for women with twin pregnancies as a preterm birth prevention strategy. • This prophylactic intervention has only been studied in a few observational trials with historical or geographic controls with conflicting results. There is insufficient evidence to support prophylactic activity restriction or work leave in multiple gestation.
- 23. CERVICAL CERCLAGE Prophylactic cervical cerclage has not been shown to be effective in preventing preterm birth in twin pregnancy in observational or controlled trials. There is moderate evidence against routine prophylactic cervical cerclage in multiple gestation. However, cerclage may be indicated for the treatment of incompetent cervix or other specific circumstances.
- 24. PROPHYLACTIC TOCOLYTIC THERAPY Most randomized controlled trials have failed to show any benefit of prophylactic oral or intravenous tocolytic therapy in multiple gestation. There is moderate evidence against prophylactic tocolysis in the management of multiple gestation, but it may be indicated on other grounds.
- 25. Is there a role for routine clinical cervical assessment in multiple gestation? • Despite the lack of precision, clinical cervical assessment appears to be safe and may be effective in monitoring twin gestations, if transvaginal ultrasound is not available or determined to be too expensive. • However, compared to transvaginal sonography, digital examination is more subjective and less reproducible. There is good evidence that premature cervical change by digital examination predicts preterm birth in twins. Since there are no well designed intervention trials available,the role of sonographic clinical cervical
- 26. Is home uterine activity monitoring useful in predicting preterm birth in twin pregnancy? Although home uterine activity monitoring may be helpful in identifying women at increased risk of preterm labour before advanced cervical dilation occurs, this information has not resulted in reduction in the incidence of preterm labour, advanced cervical dilation at presentation or preterm birth in well-controlled randomized controlled trials. *There is moderate evidence against home uterine activity monitoring in multiple gestation.
- 27. Does the measurement of fetal fibronectin predict preterm birth in twin pregnancy? Data from prospective longitudinal studies suggests that a positive fetal fibronectin test has a very high negative predictive value for the prediction of preterm birth in asymptomatic patients. The positive predictive value for preterm labour and delivery before 37 weeks is 60 percent for patients in preterm labour, 45 percent in asymptomatic high-risk women, and 30 percent in asymptomatic low-risk women. There is good evidence that the presence of cervicovaginal fetal fibronectin in twins predicts preterm birth. Without well designed intervention trials available, there is no basis for incorporating fetal fibronectin screening into routine prenatal management of multiple gestation.
- 28. MORTALITY AND MORBIDITY • Multifetal pregnancies are high-risk pregnancies. • fetal mortality rate for twins is 4 x the fetal mortality rate for single births. • neonatal mortality rate for twins is more than 5 x greater than the neonatal mortality rate for single births. • A high prevalence of low birth weight infants, due to prematurity and intrauterine growth retardation (IUGR) and their associated complications, contribute to this problem.
- 29. Complications of MultiplePregnancy • preterm labor andbirth • pregnancy-inducedhypertension/PE – Women with multiplefetuses are more than three times aslikely to develop high blood pressure ofpregnancy. – Thiscondition often develops earlier and is more severethan pregnancy with onebaby. – It canalso increase the chanceofplacental abruption (early detachment of theplacenta). • anemia – Anemia is more than twice ascommon in multiple pregnancies asina single birth. • birthdefects – Multiple birth babies have about twice the risk of congenital (present at birth) abnormalities including neural tube defects (such asspina bifida), gastrointestinal, and heartabnormalities.
- 32. UNIQUE COMPLICATIONS • Problems related to vascular anastomosis between twins • Single intrauterine demise • Discordant twins • Conjoined twins • Cord entanglement
- 33. 1. VASCULAR ANASTOMOSIS Present only in monochorionic twin placentas. Nearly 100% of monochorionic twin placentas have vascular anastomoses,but there are marked variations in the number ,size, and direction. 2 patterns of vascular anastomosis • twin-to-twin transfusionsyndrome (TTTS) • acardiac twinning or twin reversed arterial perfusion (TRAPS)
- 34. Twin-to-twin transfusion syndrome (TTTS) • Features of TTTSare the result of hypoperfusion of the donor twin and hyperperfusion of the recipient twin. • twin becomes hypovolemic and oliguric oranuric. • Oligohydramnios develops in the amniotic sacof the donortwin. • Profound oligohydramnios can result in the stuck twin phenomenon in which the twin appears in a fixed position against the uterinewall. • Ultrasonography may fail to visualize thefetal bladder becauseof absenturine.
- 36. • Either twin candevelop hydropsfetalis. – Thedonor twin canbecome hydropic becauseof anemia and high-output heart failure. – Therecipient twin canbecome hydropic because of hypervolemia. • Therecipient twin canalso develop hypertension, hypertrophic cardiomegaly, disseminated intravascular coagulation, and hyperbilirubinemia after birth.
- 37. Twin-to-twin transfusion syndrome (TTTS) • SevereTTTShasa60-100%fetal or neonatal mortality rate. • Mild-to-moderate TTTSis frequently associated with prematuredelivery. • Fetal demise of one twin is associated with neurologic sequelae in 25%of survivingtwins. • Themore premature the twins are atbirth, the higher the incidence of postnatal morbidity andmortality
- 38. QUINTERO STAGING
- 39. TWIN REVERSED ARTERIAL PERFUSION SEQUENCE (TRAPS) • 1:35,000pregnancies,1%ofmonochorionic • Largearterio-arterial anastomosis • Perinatalmortality inthepumptwinis 55%,dueto polyhydramniosandhigh-outputcardiacfailure • Anacardiactwinwhichreceivedits bloodsupplyvia alarge arterio-arterialanastomosisfromanormal‘pumpco-twin~>resultin absentorudimentarydevelopmentof theupperbody structures • NotallpregnancieswithTRAPsequencerequire invasivetreatmentand thisappearstobedependent on: i) therelativesizeofthe‘acardiac’twintothepumptwinand ii) thepresenceofanycardiovascularimpairmentinthe‘pump’twin iii) Carefulmonitoringandultrasoundsurveillanceisrequired .
- 41. SUGGESTED TREATMENT IN VASCULAR ANASTOMOSIS • Amniotic septostomy • Laser ablation • Selective fetocide • Serial amnioreduction
- 42. Treatment for established TTTS: The frequency of ultrasound surveillance of fetal health in severe cases of TTTS will depend on the severity and intervention strategy. Therapeutic options: These include: i) no intervention ( survival 0—30%), ii) amnioreduction 64 percent ( survival 64% overall, 74% of at least one twin), iii)laser photocoagulation (55% overall survival—73% of at least one twin), iv)amniotic septostomy, 83 percent survival (12 cases only).
- 44. LASER ABLATION
- 45. 2. SINGLE INTRAUTERINE DEMISE • 2-6% of twins pregnancies • Up to 25% in MC twin pregnancy • Perinatal morbidity and mortality of the surviving co- twin 19% perinatal death 24% having serious longterm sequelae • Morbidity of surviving fetus depend on chorionicity and consequences of prematurity
- 46. SINGLE FETALDEATH • After the single fetal death in a monochorionic pregnancy, the risk to the surviving twin of death or neurological abnormality is of the order of 12% and 18%, respectively. • Damage to MC twins after the death of a co-twin is now thought to be caused by acute haemodynamic changes around the time of death, with the survivor essentially haemorrhaging part of its circulating volume into the circulation of the dying twin. • This may cause transient or persistent hypotension and low perfusion,leading to the risk of ischaemic organ damage, notably but not exclusively, to the brain • Single fetal death in a monochorionic pregnancy should be referred and assessed in a regional fetal medicine centre.
- 47. 3. DISCORDANT FETAL GROWTH • Fetal growth differs slightly in twin gestations and twin specific charts may be used to define the normal growth rate. Precision may also be obtained by using sex and race specific charts. • In clinical practice, however, these differences are small and singleton growth curves may be used. Patterns of fetal growth are more important than absolute measurements. Both must be interpreted in the light of the clinical history, together with all the genetic and environmental factors that may affect fetal growth. The diagnosis of discordance has been based on the following: • AC difference of 20 mm (sensitivity of 80%, specificity 85%, PPV= 62%) • EFW based on bi-parietal diameter (BPD) and AC or AC and femur length (FL) > 20 percent (sensitivity 25-55%) Fetal weight difference = wt. of the larger - wt.of smaller wt.of the larger twin ( >15-25% poor outcome )
- 48. • It has been shown that the risk of fetal death begins to increase progressively when the weight discordance exceeds 25%. • Discordant fetal growth can be due to different genetic growth potentials, structural anomaly of one fetus, or an unfavourable placental implantation. • True discordance is an indicator for an increased risk of IUGR, morbidity, and mortality for the smaller twin. • A risk for aneuploidy, anomaly or viral syndrome affecting only one fetus must also be considered when discordant growth is identified.
- 49. Management US monitoring of growth within a twin pair = mainstay in management . The indication for delivery should take into consideration of the fetal well-being, the gestational age and serial growth velocity
- 50. 4. CONJOINED TWIN Rare complication of monoamniotic twining, with an incidence of around 1: 55 000 pregnancies. Accurate prenatal diagnosis is possible in the first trimester and allows better counseling of the parents regarding the management options. Types : Anterior (thoracopagus) Posterior (pygopagus) Cephalic (craniopagus) Caudal (ischiopagus) van den Brand(1994) ;diagnosis of conjoined twins can frequently be made at mid pregnancy using USG - careful evaluation of the point of connection and organs involved
- 53. 5. CORD ENTANGLEMENT • Cord entanglement occurs in over 70% of MCMA twins and is believed to be the major cause for sudden IUFD • Ultrasound diagnosis of cord entanglement and close fetal surveillance from 24 weeks onward, may help to improve perinatal outcome. • Because of the high perinatal mortality, prophylactic delivery by caesarean section at 32 to 34 weeks is recommended.
- 54. PRESENT A TION • 40%of twins present asvertex/vertex, • 35%as vertex/non-vertex, • remaining 25%of twins present with the leading twin in anon-vertex presentationat birth . • Blickstein 1987; Grisaru 2000
- 55. DELIVERY • If the first twin presents asbreech - -CSas being safer for thebabies. • Although many clinicians choose caesarean section when the first twin presents asa breech,because of concernabout ‘interlocking’, this complication isextremely rare. Cohenet al.47 reported ‘interlocking’ occurring only once in 817 twinpregnancies where the first twin wasbreech and the second cephalic.
- 56. DELIVERY • For twins presenting vertex/vertex, mostclinicians recommend planned VB(ACOG2002; CDSR1996). • However, planned C Smay benefit twins in which thefirst twin is presenting vertex for anumber ofreasons. • Asmany as20%of vertex presenting secondtwins will changepresentation spontaneously after the first twinis delivered (Houlihan 1996). • Asubstantial number of those presenting vertex/vertex will present with serious acute intrapartum problems following the delivery of the first twin (for example, conversion to transverse lie, cord prolapse, prolonged interval to delivery of the secondtwin), which may lead to emergency CS, perinatal death, and neonatalmorbidity.
- 57. MANAGEMENT DURING LABOR Basic Principles The presence of 2 skilled obstetrics attendants for labor and delivery Anesthesiologist available Neonatal care personnel sufficient for resuscitation of the newborns Portable US scanner Reliable IV access CTG with dual monitoring capacity
- 58. INTRAPARTUM MANAGEMENT OF TWIN PREGNANCY 1st stage Good intrapartum care : blood, IV access, continuous FH monitoring, adequate analgesia and LPC. it is also preferable to have an USG in the delivery suite to detect the FH, fetal lie and presentation when needed. Progress of labour should be closely monitored with 2-4 hourly VE. The criteria for diagnosing slow progress are the same as in singletons. In case of inefficient uterine contractions, oxytocin augmentation can be used.
- 59. 2nd stage An experienced obstetrician must be present during the 2nd stage of labour. Following delivery of the first twin, syntometrine must NOT be given as it might facilitate the premature placental separation before the delivery of the second twin. The cord of the first twin should be clamped and divided as usual. After delivery of the 1st twin, the obstetrician should ascertain the lie and presentation of the 2nd twin, using USG if required. Once a Cx presentation is confirmed, the decent of the fetal head is expected with re-establishment of uterine contractions. Oxytocin infusion should be commenced if uterine contractions have failed to resume. Fetal heart rate should be continuously monitored. A twin-to-twin delivery interval of ≤ 30 minutes, after which delivery should be expedited, since the risks of both acidosis and second stage Caesarean section increase with the length of this interval
- 60. If the second twin is in non-vertex presentation, the available options include Assisted vaginal breech delivery or breech extraction, Internal podalic version following by breech extraction, ECV followed by vaginal cephalic delivery, Emergency LSCS
- 61. 3rd stage •increased risks of primary PPH. •delivery of the shoulder of the 2nd twin, active management of the third stage should ensue. •Oxytocin infusion in addition is advised. •The placentas should be examined as a routine to confirm the chorionicity and amnionicity.
- 62. Indications for Caesarean Section Elective First twin non-cephalic Conjoined twin Monoamniotic twin Placenta previa Previous LSCS IUGR in dichorionic twin Congenital abnormality Emergency Fetal distress Cord prolapse of 1st twin Non progress of labor Collision of both twins 2nd twin transverse after delivery of 1st twin
- 63. SPECIALIZED TWIN CLINICS/PREVENTION PROGRAMMES Multi-intervention preterm birth prevention programmes for twin pregnancies have been evaluated in several observational studies with contemporary and/or historical controls. All studies reviewed suggest reduction in preterm birth rate, decreased perinatal mortality, and overall improvement in perinatal outcome. The evidence to support specialized clinics is of insufficient quality to recommend that they be part of routine clinical practice. Further randomized controlled studies are needed to validate the improved outcomes that have been demonstrated in cohort studies.
- 64. THANKYOU