Eficácia do metilfenidato e atomoxetina em crianças PHDA
- 1. Comparative Efficacy of Methylphenidate and Atomoxetine on Emotional and Behavioral Problems in Youths with Attention-Deficit/Hyperactivity Disorder Hsien-Hsueh Shih, MD,1,* Chi-Yung Shang, MD, PhD,1,2,* and Susan Shur-Fen Gau, MD, PhD1–3 Abstract Objective: Methylphenidate and atomoxetine are efficacious in reducing core symptoms of attention-deficit/hyperactivity disorder (ADHD), but little is known about their efficacy in improving emotional/behavioral problems among youths with ADHD. Methods: One hundred sixty drug-naı¨ve youths with DSM-IV-defined ADHD, aged 7–16 years, were recruited and randomly assigned to osmotic-release oral system methylphenidate (OROS-methylphenidate; n = 80) and atomoxetine (n = 80) in a 24- week, open-label, head-to-head clinical trial. The primary efficacy measure was parent-reported Child Behavior Checklist (CBCL), and the secondary efficacy measures included Youth Self Report (YSR) and Strengths and Difficulties Ques- tionnaire (SDQ), which was based on the ratings of parents, teachers, and subjects. Results: For CBCL, both methylphenidate and atomoxetine groups showed significant improvement in all scores at weeks 8 and 24 except Somatic Complaints in the atomoxetine group. For SDQ, both treatment groups showed significant im- provements in the Hyperactive and Conduct subscales for parent ratings, and the Externalizing subscale for teacher ratings at week 24. Methylphenidate was associated with greater improvements in Aggressive Behavior and Somatic Complaints of CBCL and in Conduct subscale of self-reported SDQ at week 24 compared with atomoxetine. Conclusions: Our findings provide evidence to support that both methylphenidate and atomoxetine were effective in im- proving a wide range of emotional/behavioral problems in youths with ADHD after 24 weeks of treatment, with greater improvement in aggressive behavior, somatic complaints, and conduct problems in the methylphenidate group. Keywords: attention-deficit/hyperactivity disorder, atomoxetine, clinical trial, emotional/behavioral problems, methylphenidate Introduction Attention-deficit/hyperactivity disorder (ADHD) is a common childhood mental disorder affecting 4%–13.3% of children and adolescents in western countries (Willcutt 2012) and 7%–9% in Taiwan (Gau et al. 2005). Previous studies indicate the neurological basis for this disorder (Volkow et al. 2005; Shang et al. 2013). ADHD symptoms may last to adolescence and adulthood with long-term social function impairment (Tseng and Gau 2013; Lin et al. 2015). In addition to the ADHD core symptoms, youths with ADHD are at risk of having a wide range of co-occurring psychopathologies, such as emotional dysregulation, disruptive behavior, and social problems (Spencer et al. 2011; Biederman et al. 2012; Steinhausen et al. 2012). These comorbid conditions commonly lead to a negative impact on quality of life, family function, and interpersonal relationship in individuals with ADHD (Lin et al. 2015). Furthermore, ADHD patients with emotion- al/behavioral problems often exhibit a greater number of ADHD symptoms, which correlates with increased severity of this disorder (Biederman et al. 2007). Youths with ADHD and emotional/be- havioral problems display greater levels of psychosocial impair- ment than youths with either ADHD or emotional/behavioral problems alone (Blackman et al. 2005). Accordingly, it is essential to identify these emotional/behavioral profiles of youths with ADHD in the clinical setting. Methylphenidate and atomoxetine are the only two medications approved for treating youth and adults with ADHD in many countries, and Taiwan as well (Ni et al. 2013). Methylphenidate, a 1 Department of Psychiatry, National Taiwan University Hospital, Taipei, Taiwan. 2 Department of Psychiatry, College of Medicine, National Taiwan University, Taipei, Taiwan. 3 Department of Psychology, Graduate Institute of Brain and Mind Sciences, Institute of Clinical Medicine, National Taiwan University, Taipei, Taiwan. *These authors contributed equally to this work as the first authors. Funding: This study was supported by the grant from the National Science Council (NSC 98-2314-B-002-051-MY3, NSC99-2627-B-002-015, NSC100-2627-B-002-014) and the National Health Research Institute (NHRI-EX100-10008PI, NHRI-EX101-10008PI, NHRI-EX106-10404PI), Taiwan. JOURNAL OF CHILD AND ADOLESCENT PSYCHOPHARMACOLOGY Volume XX, Number XX, 2018 ª Mary Ann Liebert, Inc. Pp. 1–11 DOI: 10.1089/cap.2018.0076 1 DownloadedbyWegnerHealthScienceInformationCenter/UniversityofSouthDakotamultisitefromwww.liebertpub.comat11/21/18.Forpersonaluseonly.
- 2. dopamine and noradrenaline reuptake inhibitor, promotes the re- lease of stored dopamine from presynaptic vesicles (Volkow et al. 2005) and is recognized as the first-line treatment for ADHD for decades worldwide. Atomoxetine is a highly specific inhibitor of presynaptic norepinephrine transporter, with little affinity for other neurotransmitter transporters or receptors (Garnock-Jones and Keating 2009). Clinical trials have shown that both methylpheni- date and atomoxetine treatments are associated with clinically meaningful and comparable effectiveness in improving the core symptoms of ADHD across situations (Kratochvil et al. 2002; Shang et al. 2015). In contrast, results for the effectiveness of methylphenidate and atomoxetine in improving emotional/behav- ioral problems in patients with ADHD are mixed. For example, although several studies observed no significant effects on emo- tional control after treatment with methylphenidate (Biederman et al. 2011), others documented the effectiveness of methylpheni- date in improving emotional dysregulation (Kutlu et al. 2017). Some trials showed a significant reduction in anxiety and depres- sion after treatment with methylphenidate in patients with ADHD (Bouffard et al. 2003); others found no change (Kuperman et al. 2001), and still others demonstrated an increase in anxiety and depressive symptoms (Spencer et al. 2005). A clinical trial dem- onstrated that atomoxetine is not superior to placebo in reducing oppositional problems (Bangs et al. 2008), whereas other studies showed positive findings for the efficacy of atomoxetine in im- proving oppositional behaviors (Dittmann et al. 2011). Given the remarkable variability in methods across pharmacological studies on ADHD (Faraone et al. 2006), further clinical trials are required to examine the efficacy of methylphenidate and atomoxetine in the treatment of emotional/behavioral problems in youths with ADHD. Numerous rating scales are available for measuring the emotion- al/behavioral symptoms associated with ADHD in different settings. Compared with narrowband scales, broadband scales such as Children Behavior Checklist (CBCL) and Strength and Difficulties Ques- tionnaire (SDQ) are better for a comprehensive assessment of the emotional/behavioral symptoms associated with ADHD. However, only a few studies have used the CBCL (Wang et al. 2013) and SDQ (Gelade et al. 2016) as outcome measures for treatment studies. For example, a previous report showed no improvement in emotion- al/behavioral symptoms measured by CBCL after treatment with methylphenidate in youths with ADHD (Wang et al. 2013). A clinical trial demonstrated that methylphenidate is associated with significant improvement in the total score of teacher-rated SDQ, but no im- provement on parent-rated SDQ (Gelade et al. 2016). Given that the emotional/behavioral symptoms influence the psychosocial functions and disease course of ADHD, a direct comparative trial is required to identify the therapeutic effect of methylphenidate and atomoxetine on the emotional/behavioral problems in youths with ADHD. The present study aimed to di- rectly compare the effectiveness of methylphenidate and atomox- etine in improving a wide range of emotional/behavioral problems in drug-naı¨ve youths with ADHD in a head-to-head, open-label, 24- week randomized clinical trial. Methods Participants We recruited drug-naı¨ve youths, aged between 7 and 16 years, who met the DSM-IV diagnostic criteria for ADHD, as assessed by the investigator’s clinical evaluation and confirmed using the Chinese version of the Schedule for Affective Disorders and Schizophrenia for School-Age Children–Epidemiological Version (K-SADSE) (Gau et al. 2005). We excluded participants who had comorbid conditions with bipolar disorders, psychosis, any sub- stance abuse, autism spectrum disorders, intellectual disability (Full-Scale Intelligence Quotient score <80), or had serious medi- cal conditions such as cardiovascular disease, history of seizure, or prior electroencephalogram abnormalities related to epilepsy, or had ever used any psychotropic medications before the study. The details have been reported elsewhere (Shang et al. 2015). Study design and procedures This study had been approved by the Research Ethics Committee of the National Taiwan University Hospital, Taiwan (IRB ID, 200812153M; ClinicalTrials.gov number, NCT00916786) before implementation. The potential subjects who met the recruitment criteria received a comprehensive explanation of the purpose and procedure of this study, as well as the reassurance of confidenti- ality. All the participants provided their written informed consent. During the 24-week, open-label, head-to-head randomized clinical trial, participants were assigned to either the osmotic-release oral system (OROS)-methylphenidate or atomoxetine group at a 1:1 ratio according to computer-generated random sequence. Participants were assessed seven times at baseline (visit 1), week 2 (visit 2), week 4 (visit 3), week 8 (visit 4), week 12 (visit 5), week 16 (visit 6), and week 24 (visit 7). At visit 1, participants started taking medication with OROS- methylphenidate (an initial dosage of 18mg per day, administered as a single morning dose) or atomoxetine (an initial dosage of 0.5mg/kg per day, administered as once-daily dose). Drug dosage would be titrated based on treatment response and adverse effects at visits 2–7 (weeks 2–24) depending upon clinical response and adverse effects. The maximal dose was 54 mg daily for OROS-methylphenidate or 1.2mg/kg daily for atomoxetine. Parent-reported CBCL and Youth Self Report (YSR) were gathered at baseline (visit 1), week 8 (visit 4), week 16 (visit 6), and week 24 (visit 7). Parent-, teacher-, and self-reported SDQ were gathered at each visit, from visit 1 through visit 7. Efficacy measure Our primary efficacy measure was parent-reported CBCL, and the secondary outcomes were YSR and SDQ. CBCL and YSR The CBCL is a parental questionnaire used to measure the emotional/behavioral problems in youths aged 4–18, and the YSR is administered to adolescents aged 11–18 to obtain self-reports about their emotional/behavioral problems (Achenbach and Du- menci 2001). Each item is scored 0 if not true, 1 if somewhat or sometimes true, and 2 if very true or often true. Eight emotion- al/behavioral scales were created for both the CBCL and YSR, including Anxious/Depressed symptoms, Attention Problems, Aggressive Behaviors, Delinquent Behaviors, Social Problems, Thought Problems, Somatic Complaints, and Withdrawn. The Chinese versions of CBCL and YSR have been shown to have good validity and reliability (Yang et al. 2001; Shang et al. 2006), and these two scales have been widely used to measure emotional/behavioral problems in Taiwanese youth populations (Chen et al. 2017). Strengths and Difficulties Questionnaire The SDQ, a 25-item screening questionnaire, has been designed to assess a broad area of emotions and behaviors of youths 2 SHIH ET AL. DownloadedbyWegnerHealthScienceInformationCenter/UniversityofSouthDakotamultisitefromwww.liebertpub.comat11/21/18.Forpersonaluseonly.
- 3. (Goodman 1999). Each item is rated on a three-point Likert scale (0 = not true, 1 = somewhat true, and 2 = certainly true). There are three versions of the SDQ for ratings by self, parents, and teachers. Our previous work on the Chinese version of SDQ identified four subscales in the parent version (prosocial, conduct, internalizing, and hyperactive), four subscales in the teacher version (peer/pro- social, externalizing, internalizing, and inattention), and five sub- scales in the self-report (prosocial, conduct, hyperactive, peer problems, and emotion) (Liu et al. 2013). Statistical analyses Baseline demographic characteristics and assessment of emo- tional/behavioral problems were presented in mean scores and SD for continuous variables, and number and corresponding percent- age for categorical variables. The t-scores of CBCL, YSR, and SDQ were used to present the severity of emotional/behavioral problems. The t-score was defined as multiplying the z-scores by 10 and adding 50, with a mean of 50 and a SD of 10. We used the intent-to- treat principle for missing data in the statistical analysis, and the last-observation-carried-forward method was applied to missing data or patient dropout. Hierarchical linear mixed-effects models were employed to address the lack of statistical independence of repeated measurements of the same participants over time. Cohen’s d was used to compute the effect size for the comparisons of scores of CBCL, YSR, and SDQ between week 8 and baseline and be- tween week 24 (last observation) and baseline, with the small, medium, and large effect sizes being d = 0.2 to <0.5, >0.5 to <0.8, and >0.8, respectively. In particular, both intercepts and slope (time) effects in the linear mixed model with time-dependent var- iables were treated as random effects, to account for variations among subjects in baseline values, and slopes for individual tra- jectories of changes in emotional/behavioral problems over visits, in addition to the main treatment and fixed time effects of the two treatment groups. To test the difference in the slope of change between the two treatment groups, the interaction terms between visits · drugs were tested. The alpha value was preselected at the level of p < 0.05. Results Sample description and medication Of the 174 patients screened, 160 were enrolled and randomly assigned to atomoxetine (n = 80) or methylphenidate (n = 80) groups. Among them, 80 patients with atomoxetine and 76 patients with methylphenidate had complete data on CBCL. Given that YSR was only applied to patients aged 11 years or more, 54 patients treated with atomoxetine and 51 patients treated with methylphe- nidate had complete data on YSR (Fig. 1). There were no statisti- cally significant group differences in demographic characteristics and baseline severity of emotional/behavioral problems except that Subjects screened (n=174) Excluded from random assignment (n=14) Entry criteria not met (n=11) Personal reasons (n=3) Subjects provided consent and randomized (n=160) Assigned to OROS-methylphenidate (n=80) Assigned to atomoxetine (n=80) Completed CBCL (n=76) and YSR (n=51) at baseline Completed CBCL (n=80) and YSR (n=54) at Completed CBCL (n=60) and YSR (n=38) at week 8 Completed CBCL (n=68) and YSR (n=45) at week Completed CBCL (n=37) and YSR (n=22) at week 24 Completed CBCL (n=36) and YSR (n=25) at week 24 FIG. 1. Flowchart of the randomization procedure. CBCL, Child Behavior Checklist; YSR, Youth Self Report. MEDICATIONS FOR EMOTIONAL/BEHAVIORAL PROBLEMS 3 DownloadedbyWegnerHealthScienceInformationCenter/UniversityofSouthDakotamultisitefromwww.liebertpub.comat11/21/18.Forpersonaluseonly.
- 4. the methylphenidate group had higher Peer/Prosocial scores of teacher-reported SDQ compared with the atomoxetine group (Table 1). For the OROS-methylphenidate group, the mean administered dose was 20.45 (SD = 6.76) mg/day or 0.64 (SD = 0.19) mg/kg per day at week 2 (visit 2), 24.91 (SD = 9.65) mg/day or 0.75 (SD = 0.24) mg/kg per day at week 4 (visit 3), 26.38 (SD = 11.32) mg/day or 0.79 (SD = 0.28) mg/kg per day at week 8 (visit 4), 27.98 (SD = 11.77) mg/day or 0.84 (SD = 0.3) mg/kg per day at week 12 (visit 5), 27.02 (SD = 11.83) mg/day or 0.81 (SD = 0.32) mg/kg per day at week 16 (visit 6), and 27.83 (SD = 12.44) mg/day or 0.82 (SD = 0.34) mg/kg per day at week 24 (visit 7). For the atomoxetine group, the mean administered dose was 26.09 (SD = 9.07) mg/day or 0.78 (SD = 0.28) mg/kg per day at week 2 (visit 2), 27.94 (SD = 9.74) mg/day or 0.84 (SD = 0.33) mg/kg per day at week 4 (visit 3), 29.37 (SD = 8.23) mg/day or 0.89 (SD = 0.31) mg/kg per day at week 8 (visit 4), 31.39 (SD = 9.12) mg/day or 0.93 (SD = 0.31) mg/kg per day at week 12 (visit 5), 31.68 (SD = 8.76) mg/day or 0.95 (SD = 0.31) mg/kg per day at week 16 (visit 6), and 31.74 (SD = 10.34) mg/day or 0.98 (SD = 0.28) mg/kg per day at week 24 (visit 7). Regarding adverse events, vomiting ( p = 0.017), somnolence ( p < 0.001), and dizziness ( p = 0.009) were reported more often for atomoxetine, while insomnia ( p = 0.035) was re- ported more often for OROS-methylphenidate. The details have been reported elsewhere (Shang et al. 2015). Efficacy on CBCL Both treatment groups showed significant improvements in all the eight scales of CBCL from baseline to week 8 and from baseline to week 24 except Somatic Complaints in the atomoxetine group (Table 2). Compared with the atomoxetine group (Table 2), the Table 1. Demographics and Baseline Emotional/Behavioral (t-Score) Between the Two Treatment Groups Mean (SD) or n (%) Atomoxetine (n = 80) Methylphenidate (n = 76) F/v2 p value Age 9.90 (2.78) 9.70 (2.42) F = 0.24 0.628 Male 70 (87.50) 66 (86.84) v2 = 0.02 0.902 Intelligence quotient (IQ) Full-scale IQ 102.92 (11.50) 105.93 (11.94) F = 2.31 0.131 Performance IQ 103.04 (13.07) 104.99 (14.02) F = 0.72 0.397 Verbal IQ 103.01 (11.33) 106.09 (9.92) F = 2.91 0.091 CBCL Aggressive behavior 62.75 (12.50) 64.98 (13.50) F = 1.09 0.297 Anxious/depressed 60.69 (14.06) 58.31 (14.82) F = 1.07 0.303 Attention problems 68.10 (10.92) 67.07 (11.90) F = 0.32 0.572 Delinquent behavior 59.20 (10.07) 61.83 (14.06) F = 1.78 0.185 Social problems 63.13 (12.25) 62.18 (11.91) F = 0.24 0.621 Somatic complaints 53.39 (12.36) 55.50 (15.04) F = 0.93 0.336 Thought problems 60.88 (11.84) 60.52 (15.66) F = 0.03 0.869 Withdrawn 58.35 (11.02) 57.45 (11.54) F = 0.25 0.621 YSR n = 54 n = 51 Aggressive behavior 61.10 (13.81) 63.56 (16.93) F = 0.67 0.415 Anxious/depressed 61.38 (18.08) 64.14 (19.86) F = 0.55 0.459 Attention problems 65.88 (13.73) 66.29 (13.97) F = 0.02 0.879 Delinquent behavior 60.49 (16.16) 61.51 (17.89) F = 0.09 0.761 Social problems 60.67 (12.93) 61.68 (13.96) F = 0.15 0.701 Somatic complaints 60.01 (18.51) 60.92 (17.46) F = 0.07 0.795 Thought problems 62.43 (16.65) 65.83 (19.09) F = 0.95 0.333 Withdrawn 60.74 (14.97) 59.40 (14.85) F = 0.21 0.646 SDQ—parent report n = 78 n = 76 Internalizing 53.89 (11.66) 53.63 (11.01) F = 0.02 0.883 Prosocial 47.10 (10.42) 48.33 (10.01) F = 0.56 0.456 Hyperactive 51.05 (6.33) 49.55 (6.90) F = 1.98 0.161 Conduct 59.84 (10.95) 61.10 (12.10) F = 0.46 0.497 SDQ—self-report n = 54 n = 51 Emotion 51.96 (10.04) 53.40 (11.01) F = 0.49 0.486 Prosocial 51.10 (12.45) 51.73 (11.89) F = 0.07 0.790 Hyperactive 53.07 (6.53) 51.85 (8.60) F = 0.68 0.412 Conduct 51.30 (10.25) 54.22 (13.97) F = 1.50 0.223 Peer problem 60.82 (10.02) 58.95 (8.23) F = 1.08 0.301 SDQ—teacher report n = 73 n = 68 Peer/prosocial 45.51 (8.91) 49.00 (9.53) F = 5.05 0.026* Externalizing 56.50 (10.18) 58.19 (10.25) F = 0.96 0.328 Internalizing 53.17 (9.45) 55.05 (10.63) F = 1.24 0.268 Inattention 45.37 (8.14) 46.43 (7.96) F = 0.62 0.434 CBCL, Child Behavior Checklist; YSR, Youth Self Report; SDQ, Strengths and Difficulties Questionnaire. *p < 0.05. 4 SHIH ET AL. DownloadedbyWegnerHealthScienceInformationCenter/UniversityofSouthDakotamultisitefromwww.liebertpub.comat11/21/18.Forpersonaluseonly.
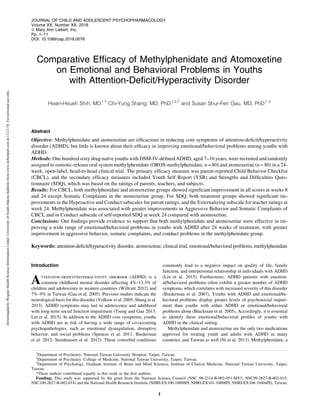
- 6. A B C D E FIG. 2. Improvements in the emotional/behavioral scores of CBCL in youths with ADHD randomly assigned to treatment with either methylphenidate or atomoxetine. (A) Aggressive Behavior; (B) Attention Problems; (C) Delinquent Behavior; (D) Social Problems; (E) Somatic Complaints. For the OROS-methylphenidate group, the mean administered dose was 26.38 (SD = 11.32) mg/day or 0.79 (SD = 0.28) mg/kg per day at visit 4, 27.02 (SD = 11.83) mg/day or 0.81 (SD = 0.32) mg/kg per day at visit 6, and 27.83 (SD = 12.44) mg/day or 0.82 (SD = 0.34) mg/kg per day at visit 7. For the atomoxetine group, the mean administered dose was 29.37 (SD = 8.23) mg/day or 0.89 (SD = 0.31) mg/kg per day at visit 4, 31.68 (SD = 8.76) mg/day or 0.95 (SD = 0.31) mg/kg per day at visit 6, and 31.74 (SD = 10.34) mg/day or 0.98 (SD = 0.28) mg/kg per day at visit 7. Error bars indicate 1 SD in both directions. *p < 0.05; d, Cohen’s d. 6 DownloadedbyWegnerHealthScienceInformationCenter/UniversityofSouthDakotamultisitefromwww.liebertpub.comat11/21/18.Forpersonaluseonly.
- 8. methylphenidate group had greater improvements in Aggressive Behavior ( p = 0.003) and Delinquent Behavior ( p = 0.009) from baseline to week 8, and in Aggressive Behavior ( p = 0.032) and Somatic Complaints ( p = 0.008) from baseline to week 24. In ad- dition, the methylphenidate group had lower scores in Attention Problems (Fig. 2B) at week 8 (Cohen’s d = 0.35) and week 16 (Cohen’s d = 0.55), and Social Problems (Fig. 2D) at week 16 (Cohen’s d = 0.57) compared with the atomoxetine group. There were significant effects of the drug · visit interactions on the Ag- gressive Behavior ( p = 0.013), Delinquent Behavior ( p = 0.041), and Somatic Complaints ( p = 0.003) (Fig. 2A, C, E). There were no effects noted for the interactions of drug · visit on the Anxious/- Depressed, Attention Problems, Social Problems, Thought Pro- blems, and Withdrawn. Efficacy on YSR Both treatment groups showed significant improvements in the YSR scores from baseline to week 8 and from baseline to week 24 except Anxious/Depressed (weeks 8 and 24) and Thought Problems (week 8) in the atomoxetine group, and Delinquent Behavior (week 8), Somatic Complaints (weeks 8 and 24), and Thought Problems (week 8) in the methylphenidate group (Table 2). The analysis of mean changes in the YSR scores (Table 2) revealed no significant differences between the two treatment groups from baseline to week 8 and from baseline to week 24. Efficacy on SDQ From baseline to week 24, both treatment groups showed sig- nificant improvements in the Hyperactive and Conduct subscales for parent ratings and the Externalizing subscale for teacher ratings (Table 3). For the self-report, the Emotion and Conduct problems improved with methylphenidate treatment at week 24, and the Hyperactive problems improved with atomoxetine treatment at week 24. Compared with the atomoxetine group, the methylphe- nidate group had greater improvements in the self-reported Con- duct subscale ( p = 0.041) at week 24. Discussion To our best knowledge, this is the first head-to-head, random- ized, long-term treatment study to prospectively compare the ef- fects of methylphenidate and atomoxetine on a wide range of emotional/behavioral problems in drug-naı¨ve youths with ADHD. We found that both treatments are efficacious in reducing the se- verity of emotional/behavioral problems measured by CBCL, YSR, and SDQ. Compared with atomoxetine, methylphenidate is asso- ciated with greater improvements in Aggressive Behavior and Somatic Complaints of CBCL and in the Conduct subscale of self- reported SDQ from baseline to week 24. In contrast to an obser- vational study showing no effect of short-acting methylphenidate on the behavioral problems measured by CBCL in youths with ADHD (Wang et al. 2013), our randomized clinical trial using OROS-methylphenidate once daily provided strong evidence to support that emotional/behavioral problems are reduced by treat- ment not only with methylphenidate but also with atomoxetine. Our results showed the large effect of treatment with methylphe- nidate in the realm of attention problems (Cohen’s d = 0.7 at week 8 and 0.8 at week 24), consistent with an average effect size of 0.8 in prior reports (Conners 2002). Previous studies have demonstrated the effects of methylphenidate (Conners 2002; Sinzig et al. 2007) and atomoxetine (Schwartz and Correll 2014) on externalizing symptoms associated with ADHD, including aggressive, oppositional, and conduct problems. Meta-analytic reviews in assessing the impact of methylphenidate (Connor et al. 2002) reported a weighted mean ef- fect size of 0.84 for overt and 0.69 for covert aggression-related behaviors in ADHD, consistent with our findings in the Aggressive Behavior subscale of CBCL for methylphenidate (Cohen’s d = 0.6 at week 8 and 0.68 at week 24). In contrast, although atomoxetine is effective in reducing the core symptoms of ADHD, a relatively small effect size of 0.33 was found for disruptive problems (Schwartz and Correll 2014), consistent with our findings in the Aggressive Beha- vior subscale of CBCL for atomoxetine (Cohen’s d = 0.24 at week 8 and 0.37 atweek24). A systemic review reporteda moderate-to-large effect for methylphenidate and a small effect for atomoxetine on oppositional behavior, conduct problems, and aggression in youths withADHD(Pringsheimetal.2015).Animalstudies haveshownthat aggressive behaviors in mice are associated with the altered function of dopamine transporter (Yu et al. 2014). Taken together, converging evidence supports that methylphenidate demonstrates a greater magnitude of treatment effect for aggressive spectrum symptoms in youths with ADHD compared with atomoxetine. Future studies are neededtoexplorethe factorsassociatedwiththedifferentialeffects of methylphenidate and atomoxetine on aggression. Similarly, our findings demonstrated the effectiveness of both methylphenidate and atomoxetine in improving the externalizing problems assessed by a parent- and teacher-rated SDQ at week 24, including Hyperactive, Conduct, and Externalizing subscales. No significant improvement in parent- and self-rated Prosocial subscale was observed after 24-week treatment with methylphenidate or atomoxetine, whereas atomoxetine is associated with improvement in teacher-rated Peer/Prosocial subscale at weeks 8 and 24. Our previous work has shown the effectiveness of atomoxetine in chil- dren with ADHD in improving interactions with peers and teachers (Shang and Gau 2012). The literature documents the importance of teacher ratings on treatment response in youths with ADHD (La- vigne et al. 2012), and a lack of reports from teachers may result in the inadequate assessment of treatment effects (Miller 1999). For internalizing symptoms, our findings showed a similar ef- ficacy of methylphenidate and atomoxetine in reducing Anxious/- Depressed symptoms measured by CBCL in youths with ADHD, with effect sizes ranging from 0.31 to 0.44. Previous studies demonstrated the efficacy of atomoxetine on anxiety symptoms associated with ADHD, with an effect size of 0.4 (Geller et al. 2007). In addition, clinical trials showed that symptoms of anxiety and depression in patients with ADHD improved after treatment with methylphenidate (Mattos et al. 2013). The Somatic Complaints subscale of CBCL, one of the inter- nalizing problems, is intended to assess the physical symptoms with no medical basis, and psychiatric disability may accentuate the incidence of somatic complaints in children with ADHD (Egger et al. 1999). Previous studies showed that parent-rated somatic complaints improved after treatment with methylphenidate (Rap- port et al. 2002) in youths with ADHD, consistent with our findings. Youths with ADHD experience significant distress at home and in school, owing to inherent difficulties with this disorder, and may internalize this distress as physical complaint (Rapport et al. 2002). Further studies are needed to examine whether improved perfor- mance at home and in school associated with methylphenidate treatment corresponds with reductions in parent-rated somatic complaints in youths with ADHD. In our present study, changes in YSR scores also showed sig- nificant improvements in emotional/behavioral problems from baseline to week 24 for both methylphenidate and atomoxetine, 8 SHIH ET AL. DownloadedbyWegnerHealthScienceInformationCenter/UniversityofSouthDakotamultisitefromwww.liebertpub.comat11/21/18.Forpersonaluseonly.
- 9. except the Anxious/Depressed subscale for atomoxetine and the Somatic Complaints subscale for methylphenidate, inconsistent with parent ratings of treatment response measured by CBCL. Although youths are valuable informants about their own emo- tional/behavioral problems (Klimkeit et al. 2006), previous studies analyzing ratings on CBCL and YSR showed better parent–youth agreement for externalizing problems than internalizing problems (Rescorla et al. 2017). For example, youths may report more anx- ious symptoms with higher degrees of intensity than their parents (Weitkamp et al. 2010). Parent–youth discrepancies may arise due to not only contextual variations in emotional/behavioral problems (De Los Reyes et al. 2013) but also parents’ inability to observe youths’ emotional/behavioral problems where they are not present (Achenbach 2011). Further research is needed to identify the spe- cific factors associated with the inconsistent ratings of treatment response for Anxious/Depressed symptoms and Somatic Com- plaints between parents and youths with ADHD. There are several methodological limitations in our study. First, due to a lack of a placebo group, we could not determine whether the improvements in emotional/behavioral problems may be partially at- tributedtotheplaceboormaturityeffect.Inaddition,wewereunableto contrast both baseline and placebo with active drug conditions to dif- ferentiate the drug-unrelated somatic complaints from those due to drug-related side effects. Second, methylphenidate is a controlled drug in Taiwan, which prevents us from conducting a double- blinded, placebo-controlled trial as an investigator-initiated clin- ical trial. The bias derived by an open trial design could be reduced since in Taiwan neither a teacher nor a school nurse distributed medication to students, and thus the teachers were blinded to which medication the subjects were taking. Third, given that the stimu- lant comparator in the present study was OROS-methylphenidate, our findings may not be generalized to other formulations of methylphenidate or Dextro-amphetamine. Fourth, we included the study sample from only one medical center in Taipei. Thus, the study results may not be generalized to broader ethnic Chinese populations with ADHD. Fifth, allowing investigators to adjust dose without using a systematic titration schedule could have led to underdosing in one group or the other; however, doses in the current study were consistent with those in the package informa- tion. Sixth, missing data in the long-term follow-up period may result in insufficient power to detect the differences in efficacy between the two drugs. Conclusions Our findings suggest that information about the emotional/be- havioral profiles, collected from direct caregivers, school teachers, and self-reports, is valuable in monitoring the response to phar- macological treatment in youths with ADHD. Clinical Significance Our findings demonstrate that both methylphenidate and ato- moxetine produce significant reductions in emotional/behavioral problems measured by CBCL, YSR, and SDQ, suggesting that obtaining assessments from multiple informants is crucial in es- tablishing a comprehensive understanding of the pharmacological effects in youths with ADHD. Author Contributions C.Y.S. and S.S.G. contributed to concept and design of the study. H.H.S., C.Y.S., and S.S.G. contributed to data acquisition/analy- sis/interpretation. H.H.S. and C.Y.S. contributed to drafting the article, tables, and figures, which were critically reviewed by S.S.G. All authors read and approved the final version of the article. Acknowledgment The authors express thanks to Ming-Fang Chen, M.S., for as- sistance in data analysis. Disclosures C.Y.S. has conducted clinical trials on behalf of and was on the speakers’ bureau for Janssen-Cilag and Eli Lilly & Co., Taiwan. S.S.G. has conducted clinical trials on behalf of and was on the speakers’ bureau for Janssen-Cilag, Eli Lilly & Co., and Astellas Pharma, Inc., Taiwan. References Achenbach TM: Commentary: Definitely more than measurement error: But how should we understand and deal with informant discrepancies? J Clin Child Adolesc Psychol 40:80–86, 2011. Achenbach TM, Dumenci L: Advances in empirically based assess- ment: Revised cross-informant syndromes and new DSM-oriented scales for the CBCL, YSR, and TRF: Comment on Lengua, Sa- dowksi, Friedrich, and Fischer (2001). J Consult Clin Psychol 69: 699–702, 2001. Bangs ME, Hazell P, Danckaerts M, Hoare P, Coghill DR, Wehmeier PM, Williams DW, Moore RJ, Levine L, Atomoxetine AODDSG: Ato- moxetine for the treatment of attention-deficit/hyperactivity disorder and oppositional defiant disorder. Pediatrics 121:e314–e320, 2008. Biederman J, Spencer TJ, Newcorn JH, Gao H, Milton DR, Feldman PD, Witte MM: Effect of comorbid symptoms of oppositional de- fiant disorder on responses to atomoxetine in children with ADHD: A meta-analysis of controlled clinical trial data. Psychopharma- cology (Berl) 190:31–41, 2007. Biederman J, Mick E, Fried R, Wilner N, Spencer TJ, Faraone SV: Are stimulants effective in the treatment of executive function deficits? Results from a randomized double blind study of OROS- methylphenidate in adults with ADHD. Eur Neuropsychopharmacol 21:508–515, 2011. Biederman J, Petty CR, Day H, Goldin RL, Spencer T, Faraone SV, Surman CBH: Severity of the Aggression/Anxiety-Depression/ Attention (A-A-A) CBCL profile discriminates between different levels of deficits in emotional regulation in youth with ADHD. J Dev Behav Pediatr 33:236–243, 2012. Blackman GL, Ostrander R, Herman KC: Children with ADHD and depression: A multisource, multimethod assessment of clinical, social, and academic functioning. J Atten Disord 8:195–207, 2005. Bouffard R, Hechtman L, Minde K, Iaboni-Kassab F: The efficacy of 2 different dosages of methylphenidate in treating adults with attention- deficit hyperactivity disorder. Can J Psychiatry 48:546–554, 2003. Chen YY, Ho SY, Lee PC, Wu CK, Gau SS: Parent-child dis- crepancies in the report of adolescent emotional and behavioral problems in Taiwan. PLoS One 12:e0178863, 2017. Conners CK: Forty years of methylphenidate treatment in attention- deficit/hyperactivity disorder. J Atten Disord 6 Suppl 1:S17–S30, 2002. Connor DF, Glatt SJ, Lopez ID, Jackson D, Melloni RH, Jr.: Psy- chopharmacology and aggression. I: A meta-analysis of stimulant effects on overt/covert aggression-related behaviors in ADHD. J Am Acad Child Adolesc Psychiatry 41:253–261, 2002. De Los Reyes A, Thomas SA, Goodman KL, Kundey SM: Principles underlying the use of multiple informants’ reports. Annu Rev Clin Psychol 9:123–149, 2013. MEDICATIONS FOR EMOTIONAL/BEHAVIORAL PROBLEMS 9 DownloadedbyWegnerHealthScienceInformationCenter/UniversityofSouthDakotamultisitefromwww.liebertpub.comat11/21/18.Forpersonaluseonly.
- 10. Dittmann RW, Schacht A, Helsberg K, Schneider-Fresenius C, Leh- mann M, Lehmkuhl G, Wehmeier PM: Atomoxetine versus placebo in children and adolescents with attention-deficit/hyperactivity disorder and comorbid oppositional defiant disorder: A double- blind, randomized, multicenter trial in Germany. J Child Adolesc Psychopharmacol 21:97–110, 2011. Egger HL, Costello EJ, Erkanli A, Angold A: Somatic complaints and psychopathology in children and adolescents: Stomach aches, musculoskeletal pains, and headaches. J Am Acad Child Adolesc Psychiatry 38:852–860, 1999. Faraone SV, Biederman J, Spencer TJ, Aleardi M: Comparing the efficacy of medications for ADHD using meta-analysis. Med- GenMed 8:4, 2006. Garnock-Jones KP, Keating GM: Atomoxetine: A review of its use in attention-deficit hyperactivity disorder in children and adolescents. Paediatr Drugs 11:203–226, 2009. Gau SS, Chong MY, Chen TH, Cheng AT: A 3-year panel study of mental disorders among adolescents in Taiwan. Am J Psychiatry 162:1344–1350, 2005. Gelade K, Janssen TW, Bink M, van Mourik R, Maras A, Oosterlaan J: Behavioral effects of neurofeedback compared to stimulants and physical activity in attention-deficit/hyperactivity disorder: A ran- domized controlled trial. J Clin Psychiatry 77:e1270–e1277, 2016. Geller D, Donnelly C, Lopez F, Rubin R, Newcorn J, Sutton V, Bakken R, Paczkowski M, Kelsey D, Sumner C: Atomoxetine treatment for pediatric patients with attention-deficit/hyperactivity disorder with comorbid anxiety disorder. J Am Acad Child Adolesc Psychiatry 46:1119–1127, 2007. Goodman R: The extended version of the Strengths and Difficulties Questionnaire as a guide to child psychiatric caseness and conse- quent burden. J Child Psychol Psychiatry 40:791–799, 1999. Klimkeit E, Graham C, Lee P, Morling M, Russo D, Tonge B: Children should be seen and heard: Self-report of feelings and behaviors in primary-school-age children with ADHD. J Atten Disord 10:181–191, 2006. Kratochvil CJ, Heiligenstein JH, Dittmann R, Spencer TJ, Biederman J, Wernicke J, Newcorn JH, Casat C, Milton D, Michelson D: Atomoxetine and methylphenidate treatment in children with ADHD: A prospective, randomized, open-label trial. J Am Acad Child Adolesc Psychiatry 41:776–784, 2002. Kuperman S, Perry PJ, Gaffney GR, Lund BC, Bever-Stille KA, Arndt S, Holman TL, Moser DJ, Paulsen JS: Bupropion SR vs. methyl- phenidate vs. placebo for attention deficit hyperactivity disorder in adults. Ann Clin Psychiatry 13:129–134, 2001. Kutlu A, Akyol Ardic U, Ercan ES: Effect of methylphenidate on emotional dysregulation in children with attention-deficit/ hyperactivity disorder + oppositional defiant disorder/conduct dis- order. J Clin Psychopharmacol 37:220–225, 2017. Lavigne JV, Dulcan MK, LeBailly SA, Binns HJ: Can parent reports serve as a proxy for teacher ratings in medication management of attention-deficit hyperactivity disorder? J Dev Behav Pediatr 33: 336–342, 2012. Lin YJ, Lo KW, Yang LK, Gau SS: Validation of DSM-5 age-of-onset criterion of attention deficit/hyperactivity disorder (ADHD) in adults: Comparison of life quality, functional impairment, and family function. Res Dev Disabil 47:48–60, 2015. Liu SK, Chien YL, Shang CY, Lin CH, Liu YC, Gau SSF: Psycho- metric properties of the Chinese version of Strength and Difficulties Questionnaire. Compr Psychiatry 54:720–730, 2013. Mattos P, Louza MR, Palmini AL, de Oliveira IR, Rocha FL: A multicenter, open-label trial to evaluate the quality of life in adults with ADHD treated with long-acting methylphenidate (OROS MPH): Concerta Quality of Life (CONQoL) study. J Atten Disord 17:444–448, 2013. Miller A: Appropriateness of psychostimulant prescription to chil- dren: Theoretical and empirical perspectives. Can J Psychiatry 44: 1017–1024, 1999. Ni HC, Shang CY, Gau SS, Lin YJ, Huang HC, Yang LK: A head-to- head randomized clinical trial of methylphenidate and atomoxetine treatment for executive function in adults with attention-deficit hyperactivity disorder. Int J Neuropsychopharmacol 16:1959–1973, 2013. Pringsheim T, Hirsch L, Gardner D, Gorman DA: The pharmaco- logical management of oppositional behaviour, conduct problems, and aggression in children and adolescents with attention-deficit hyperactivity disorder, oppositional defiant disorder, and conduct disorder: A systematic review and meta-analysis. Part 1: psychos- timulants, alpha-2 agonists, and atomoxetine. Can J Psychiatry 60: 42–51, 2015. Rapport MD, Randall R, Moffitt C: Attention-Deficit/Hyperactivity Disorder and methylphenidate: A dose-response analysis and parent-child comparison of somatic complaints. J Atten Disord 6: 15–24, 2002. Rescorla LA, Ewing G, Ivanova MY, Aebi M, Bilenberg N, Dieleman GC, Dopfner M, Kajokiene I, Leung PW, Pluck J, Steinhausen HC, Winkler Metzke C, Zukauskiene R, Verhulst FC: Parent-adolescent cross-informant agreement in clinically referred samples: Find- ings from seven societies. J Clin Child Adolesc Psychol 46:74–87, 2017. Schwartz S, Correll CU: Efficacy and safety of atomoxetine in chil- dren and adolescents with attention-deficit/hyperactivity disorder: Results from a comprehensive meta-analysis and metaregression. J Am Acad Child Adolesc Psychiatry 53:174–187, 2014. Shang CY, Gau SS, Soong WT: Association between childhood sleep problems and perinatal factors, parental mental distress and be- havioral problems. J Sleep Res 15:63–73, 2006. Shang CY, Gau SS: Improving visual memory, attention, and school function with atomoxetine in boys with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 22:353–363, 2012. Shang CY, Wu YH, Gau SS, Tseng WY: Disturbed microstructural integrity of the frontostriatal fiber pathways and executive dys- function in children with attention deficit hyperactivity disorder. Psychol Med 43:1093–1107, 2013. Shang CY, Pan YL, Lin HY, Huang LW, Gau SS: An open-label, randomized trial of methylphenidate and atomoxetine treatment in children with attention-deficit/hyperactivity disorder. J Child Ado- lesc Psychopharmacol 25:566–573, 2015. Sinzig J, Do¨pfner M, Lehmkuhl G: Long-acting methylphenidate has an effect on aggressive behavior in children with attention-deficit/ hyperactivity disorder. J Child Adolesc Psychopharmacol 17:421– 432, 2007. Spencer T, Biederman J, Wilens T, Doyle R, Surman C, Prince J, Mick E, Aleardi M, Herzig K, Faraone S: A large, double-blind, randomized clinical trial of methylphenidate in the treatment of adults with attention-deficit/hyperactivity disorder. Biol Psychiatry 57:456–463, 2005. Spencer TJ, Faraone SV, Surman CB, Petty C, Clarke A, Batchelder H, Wozniak J, Biederman J: Toward defining deficient emotional self-regulation in children with attention-deficit/hyperactivity dis- order using the Child Behavior Checklist: A controlled study. Postgrad Med 123:50–59, 2011. Steinhausen HC, Zulli-Weilenmann N, Brandeis D, Muller UC, Valko L, Drechsler R: The behavioural profile of children with attention- deficit/hyperactivity disorder and of their siblings. Eur Child Adolesc Psychiatry 21:157–164, 2012. Tseng WL, Gau SS: Executive function as a mediator in the link between attention-deficit/hyperactivity disorder and social prob- lems. J Child Psychol Psychiatry 54:996–1004, 2013. 10 SHIH ET AL. DownloadedbyWegnerHealthScienceInformationCenter/UniversityofSouthDakotamultisitefromwww.liebertpub.comat11/21/18.Forpersonaluseonly.
- 11. Volkow ND, Wang GJ, Fowler JS, Ding YS: Imaging the effects of methylphenidate on brain dopamine: New model on its therapeutic actions for attention-deficit/hyperactivity disorder. Biol Psychiatry 57:1410–1415, 2005. Wang LJ, Chen CK, Huang YS: Changes in behaviour symptoms of patients with attention deficit/hyperactivity disorder during treat- ment: Observation from different informants. Psychiatry Invest 10: 1–7, 2013. Weitkamp K, Romer G, Rosenthal S, Wiegand-Grefe S, Daniels J: German Screen for Child Anxiety Related Emotional Disorders (SCARED): Reliability, validity, and cross-informant agreement in a clinical sample. Child Adolesc Psychiatry Ment Health 4:19, 2010. Willcutt EG: The prevalence of DSM-IV attention-deficit/hyperactivity disorder: A meta-analytic review. Neurotherapeutics 9:490–499, 2012. Yang HJ, Chen WJ, Soong WT: Rates and patterns of comorbidity of adolescent behavioral syndromes as reported by parents and teachers in a Taiwanese nonreferred sample. J Am Acad Child Adolesc Psychiatry 40:1045–1052, 2001. Yu Q, Teixeira CM, Mahadevia D, Huang Y, Balsam D, Mann JJ, Gingrich JA, Ansorge MS: Dopamine and serotonin signaling during two sensitive developmental periods differentially impact adult aggressive and affective behaviors in mice. Mol Psychiatry 19:688–698, 2014. Address correspondence to: Chi-Yung Shang, MD, PhD Department of Psychiatry National Taiwan University Hospital No. 7, Chung-Shan South Road Taipei 10002 Taiwan E-mail: cyshang@ntu.edu.tw MEDICATIONS FOR EMOTIONAL/BEHAVIORAL PROBLEMS 11 DownloadedbyWegnerHealthScienceInformationCenter/UniversityofSouthDakotamultisitefromwww.liebertpub.comat11/21/18.Forpersonaluseonly.