More Related Content Similar to ‘Neurodynamics as a therapeutic intervention; the effectiveness and scientific evidence?’ Similar to ‘Neurodynamics as a therapeutic intervention; the effectiveness and scientific evidence?’ (20) More from NVMT-symposium (9) 1. Title
Name
Neurodynamics as a therapeutic
intervention; effectiveness and
scientific evidence
Dr Toby Hall
Specialist Musculoskeletal Physiotherapist
Adjunct Associate Professor (Curtin University)
Snr Teaching Fellow (The University of Western Australia)
Accredited Mulligan Concept Teacher
toby@manualconcepts.com
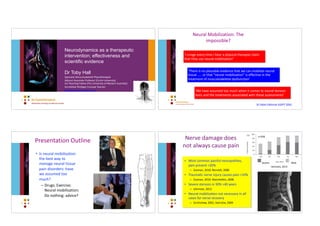
‘I cringe every time I hear a physical therapist claim
that they use neural mobilization’
‘We have assumed too much when it comes to neural tension
tests and the treatments associated with these assessments’
‘There is no plausible evidence that we can mobilize neural
tissue ….. or that "neural mobilization" is effective in the
treatment of musculoskeletal dysfunction’
Neural Mobilization: The
impossible?
Di Fabio Editorial JOSPT 2001
Presentation Outline
• Is neural mobilisation
the best way to
manage neural tissue
pain disorders: have
we assumed too
much?
– Drugs; Exercise;
Neural mobilisation;
Do nothing: advice?
Severe Mod
Nerve damage does
not always cause pain
Ishimoto, 2013
n=938
• Most common painful neuropathies,
pain present <20%
– Zusman, 2010; Bennea, 2006
• Traumacc nerve injury causes pain <10%
– Zusman, 2010; Marchedni, 2006
• Severe stenosis in 30% >40 years
– Ishimoto, 2013
• Neural mobilisacon not necessary in all
cases for nerve recovery
– Scrimshaw, 2001; Svernlov, 2009
3. Exercise reduces features of acute neuropathic pain
• Rat sciacc nerve CCI
– Daily progressive exercise on
treadmill (60 minutes) or
swimming (90 minutes with rests)
– Mechanical & thermal
hyperalgesia improved
– Aaenuated cytokine produccon
(TNF-α & IL-1β)
9
Chen, 2012
Thermal
hyperalgesia
Mechanical
hyperalgesia
Exercise reduces neuropathic pain
• Rat sciacc nerve chronic constriccon or
inflammatory model
– Treadmill daily progressive exercise 30 minutes 7 days
post surgery for 14 days
– Mechanical & thermal hyperalgesia improved
– Aaenuated pain within 3 weeks, sensory
hypersensicvity returned 5 days aher stopping exercise.
Effect of exercise reversed with opioid receptor
antagonist. Same effect if exercise delayed by 4 weeks.
• Exercise upregulates endogenous opioids
10
Stagg, 2011
CC
CCI NMI
Sham NM
Naive
Movement promotes nerve recovery: reduces NP
• Rat sciacc nerve CCI model
– 10 sessions NM under light anaestheczacon 14
days post injury
– Allodynia & hyperalgesia improved
– Significant change in glial cell density & nerve
growth factor expression in the DRG & spinal
cord
11
Santos, Molecular Pain 2011
Mechanical hyperalgesia
Exercise reduces NP post CCI
• Rat sciacc CCI
– Wheel running 6/52 prior to CCI & aher
CCI
– Allodynia improved aher injury
– Prior exercise decreased neuroimmune
signalling in DH & neuron injury.
Suppressed pro-inflammatory and
increased anc-inflammatory mediators
– Significant changes in glial cell density &
NGF expression in the DRG & spinal cord
• Exercise prevents pain, promotes
recovery & relieves pain
12
Grace, Pain 2016
Allodynia
4. Summary
Basic science
• Movement
– Exercise prevents development of NP
– Exercise aids nerve recovery aher injury & reduces NP in
animal models
• Passive limb movement
• Aerobic non-specific exercise: walking, running and swimming
• Neural mobilisacon
13
But…..
14
– Is movement effective in humans?
– Is movement effective for all
nerve disorders?
– Is movement effective for chronic
& acute nerve disorders?
– Is specific nerve movement (NM)
more effective than other forms
of movement/exercise?
What is the evidence in humans?
• Limited evidence
– SR of RCT’s for neural mobilization
– 20 trials identified; generally small scale
– Evidence NM more effective minimal treatment (pain &
disability), but no better than other treatments.
• Su, 2016
• SR identified 6 studies of NM for CTS
– NM better than no treatment: weak effect size
• McKeon, 2008
• Cochrane review found no benefit for NM
• Page, 2012
• European guidelines for management of CTS do not include
physiotherapy!
• Huisstede, 2014
15
Neural gliding exercise
• Limited & poor quality evidence for the effeccveness of
neural gliding exercises in CTS
16
Effectiveness of Nerve Gliding Exercises
on Carpal Tunnel Syndrome: A
Systematic Review
Ruth Ballestero-Pérez, PhD,a
Gustavo Plaza-Manzano, PhD,b
Alicia Urraca-Gesto, PT,c
Flor Romo-Romo, PT,c
María de los Ángeles Atín-Arratibel, MD,a
Daniel Pecos-Martín, PhD,d
Tomás Gallego-Izquierdo, PhD,d
and Natalia Romero-Franco, PhDe
ABSTRACT
Objective: The objective of this study was to review the literature regarding the effectiveness of neural gliding
exercises for the management of carpal tunnel syndrome (CTS).
Methods: A computer-based search was completed through May 2014 in PubMed, Physiotherapy Evidence Database
(PEDro), Web of Knowledge, Cochrane Plus, and CINAHL. The following key words were included: nerve tissue,
gliding, exercises, carpal tunnel syndrome, neural mobilization, and neurodynamic mobilization. Thirteen clinical
trials met the inclusion/exclusion criteria, which were: nerve gliding exercise management of participants aged
18 years or older; clinical or electrophysiological diagnostics of CTS; no prior surgical treatment; and absence of
systemic diseases, degenerative joint diseases, musculoskeletal affectations in upper limbs or spine, or pregnancy. All
studies were independently appraised using the PEDro scale.
Results: The majority of studies reported improvements in pain, pressure pain threshold, and function of CTS patients
after nerve gliding, combined or not with additional therapies. When comparing nerve gliding with other therapies, 2
studies reported better results from standard care and 1 from use of a wrist splint, whereas 3 studies reported greater
and earlier pain relief and function after nerve gliding in comparison with conservative techniques, such as ultrasound
and wrist splint. However, 6 of the 13 studies had a quality of 5 of 11 or less according to the PEDro scale.
Conclusion: Limited evidence is available on the effectiveness of neural gliding. Standard conservative care seems to
be the most appropriate option for pain relief, although neural gliding might be a complementary option to accelerate
recovery of function. More high-quality research is still necessary to determine its effectiveness and the subgroups of
patients who may respond better to this treatment. (J Manipulative Physiol Ther 2017;40:50-59)
Key Indexing Terms: Carpal Tunnel Syndrome; Nerve Tissue; Stress, Mechanical; Exercise Therapy; Movement
Effectiveness of Nerve Gliding Exercises
on Carpal Tunnel Syndrome: A
Systematic Review
Ruth Ballestero-Pérez, PhD,a
Gustavo Plaza-Manzano, PhD,b
Alicia Urraca-Gesto, PT,c
Flor Romo-Romo, PT,c
María de los Ángeles Atín-Arratibel, MD,a
Daniel Pecos-Martín, PhD,d
Tomás Gallego-Izquierdo, PhD,d
and Natalia Romero-Franco, PhDe
ABSTRACT
Objective: The objective of this study was to review the literature regarding the effectiveness of neural gliding
exercises for the management of carpal tunnel syndrome (CTS).
Methods: A computer-based search was completed through May 2014 in PubMed, Physiotherapy Evidence Database
(PEDro), Web of Knowledge, Cochrane Plus, and CINAHL. The following key words were included: nerve tissue,
gliding, exercises, carpal tunnel syndrome, neural mobilization, and neurodynamic mobilization. Thirteen clinical
trials met the inclusion/exclusion criteria, which were: nerve gliding exercise management of participants aged
18 years or older; clinical or electrophysiological diagnostics of CTS; no prior surgical treatment; and absence of
systemic diseases, degenerative joint diseases, musculoskeletal affectations in upper limbs or spine, or pregnancy. All
studies were independently appraised using the PEDro scale.
Results: The majority of studies reported improvements in pain, pressure pain threshold, and function of CTS patients
after nerve gliding, combined or not with additional therapies. When comparing nerve gliding with other therapies, 2
studies reported better results from standard care and 1 from use of a wrist splint, whereas 3 studies reported greater
and earlier pain relief and function after nerve gliding in comparison with conservative techniques, such as ultrasound
and wrist splint. However, 6 of the 13 studies had a quality of 5 of 11 or less according to the PEDro scale.
Conclusion: Limited evidence is available on the effectiveness of neural gliding. Standard conservative care seems to
be the most appropriate option for pain relief, although neural gliding might be a complementary option to accelerate
recovery of function. More high-quality research is still necessary to determine its effectiveness and the subgroups of
patients who may respond better to this treatment. (J Manipulative Physiol Ther 2017;40:50-59)
Key Indexing Terms: Carpal Tunnel Syndrome; Nerve Tissue; Stress, Mechanical; Exercise Therapy; Movement
Effectiveness of Nerve Gliding Exercises
on Carpal Tunnel Syndrome: A
Systematic Review
Ruth Ballestero-Pérez, PhD,a
Gustavo Plaza-Manzano, PhD,b
Alicia Urraca-Gesto, PT,c
Flor Romo-Romo, PT,c
María de los Ángeles Atín-Arratibel, MD,a
Daniel Pecos-Martín, PhD,d
Tomás Gallego-Izquierdo, PhD,d
and Natalia Romero-Franco, PhDe
ABSTRACT
Objective: The objective of this study was to review the literature regarding the effectiveness of neural gliding
exercises for the management of carpal tunnel syndrome (CTS).
Methods: A computer-based search was completed through May 2014 in PubMed, Physiotherapy Evidence Database
(PEDro), Web of Knowledge, Cochrane Plus, and CINAHL. The following key words were included: nerve tissue,
gliding, exercises, carpal tunnel syndrome, neural mobilization, and neurodynamic mobilization. Thirteen clinical
trials met the inclusion/exclusion criteria, which were: nerve gliding exercise management of participants aged
18 years or older; clinical or electrophysiological diagnostics of CTS; no prior surgical treatment; and absence of
systemic diseases, degenerative joint diseases, musculoskeletal affectations in upper limbs or spine, or pregnancy. All
studies were independently appraised using the PEDro scale.
Results: The majority of studies reported improvements in pain, pressure pain threshold, and function of CTS patients
after nerve gliding, combined or not with additional therapies. When comparing nerve gliding with other therapies, 2
studies reported better results from standard care and 1 from use of a wrist splint, whereas 3 studies reported greater
and earlier pain relief and function after nerve gliding in comparison with conservative techniques, such as ultrasound
and wrist splint. However, 6 of the 13 studies had a quality of 5 of 11 or less according to the PEDro scale.
Conclusion: Limited evidence is available on the effectiveness of neural gliding. Standard conservative care seems to
be the most appropriate option for pain relief, although neural gliding might be a complementary option to accelerate
recovery of function. More high-quality research is still necessary to determine its effectiveness and the subgroups of
patients who may respond better to this treatment. (J Manipulative Physiol Ther 2017;40:50-59)
Key Indexing Terms: Carpal Tunnel Syndrome; Nerve Tissue; Stress, Mechanical; Exercise Therapy; Movement
INTRODUCTION
Carpal tunnel syndrome (CTS) is the result of an
irritation, compression, or stretching of the median nerve
as it passes through the carpal tunnel in the wrist. Symptoms
range from pain (mainly nightly)1
and paresthesia to thenar
eminence muscle atrophy2-6
This syndrome represents the
most prevalent neural injury in the general population
(1-4%)7-9
and workers at risk (15-20%)10-12
(those requiring
a
Departamento de Medicina Física y Rehabilitación, Universidad
Complutense de Madrid, Madrid, Spain.
b
Departamento de Medicina Física y Rehabilitación, Facultad
de Medicina, Universidad Complutense de Madrid; Instituto de
Investigación Sanitaria del Hospital Clínico San Carlos (IdISSC),
Madrid, Spain.
c
Departamento de Rehabilitación y Fisioterapia, Hospital
Universitario Fundación Alcorcón, Madrid, Spain.
d
Departamento de Enfermería y Fisioterapia, Universidad de
Alcalá, Madrid, Spain.
e
Department of Nursing and Physiotherapy, University of the
5. Why? Do other factors predict pain
in CTS?
• n=54 CTS confirmed by nerve conduccon tests
– Not electrophysiological tescng
• Not extent of nerve compression
– Not age, sex or other demographic variables
– Illness behaviour predict pain
• Depression & catastrophizacon account for 39% of variance in pain
• Nunez, 2010
• n= 82 post surgical recovery from CTS
– Dissacsfaccon and perceived disability predicted by depression and poor
coping skills & less degree by nerve damage
• Lozano Calderon, 2008
Screen for psychosocial issues
Why? Do other factors predict pain in CTS?
• Case control series of 68 patients with CTS & 138
healthy controls
– Matched for age & gender & stratified for
BMI
– Side laying sleeping position strongly
associated with presence of CTS
• McCabe, 2011
• Sleep quality most important predictor of
recovery neck disorders
• Kovacs, 2016
Screen for sleep position & quality
Compressive neuropathy
< sliding
Central sensiczacon
Sleep issues
Axonal mechanosensicvity
Musculoskeletal pain
> transverse sliding
Nerve swelling
Not all with CTS are suited to neural mobilisacon:
wash-out effect 2017
[ RESEARCH REPORT ]
Cnearly
injuries
in the ge
ported to
Individua
been ide
likely to
asymptom
in a mass
dividual a
STUDY DESIGN: Randomized parallel-group
trial.
BACKGROUND: Carpal tunnel syndrome (CTS)
is a common pain condition that can be managed
surgically or conservatively.
OBJECTIVE: To compare the effectiveness of
manual therapy versus surgery for improving self-
reported function, cervical range of motion, and
pinch-tip grip force in women with CTS.
METHODS: In this randomized clinical trial, 100
women with CTS were randomly allocated to either
a manual therapy (n = 50) or a surgery (n = 50)
group. The primary outcome was self-rated hand
function, assessed with the Boston Carpal Tunnel
Questionnaire. Secondary outcomes included
active cervical range of motion, pinch-tip grip
force, and the symptom severity subscale of the
Boston Carpal Tunnel Questionnaire. Patients were
assessed at baseline and 1, 3, 6, and 12 months
after the last treatment by an assessor unaware
of group assignment. Analysis was by intention to
treat, with mixed analyses of covariance adjusted
1 month for self-reported function (mean change,
–0.8; 95% confidence interval [CI]: –1.1, –0.5)
and pinch-tip grip force on the symptomatic side
(thumb-index finger: mean change, 2.0; 95% CI:
1.1, 2.9 and thumb-little finger: mean change, 1.0;
95% CI: 0.5, 1.5). Improvements in self-reported
function and pinch grip force were similar between
the groups at 3, 6, and 12 months. Both groups
reported improvements in symptom severity that
were not significantly different at all follow-up
periods. No significant changes were observed in
pinch-tip grip force on the less symptomatic side
and in cervical range of motion in either group.
CONCLUSION: Manual therapy and surgery had
similar effectiveness for improving self-reported
function, symptom severity, and pinch-tip grip
force on the symptomatic hand in women with
CTS. Neither manual therapy nor surgery resulted
in changes in cervical range of motion.
LEVEL OF EVIDENCE: Therapy, level 1b. Pro-
spectively registered September 3, 2014 at www.
clinicaltrials.gov (NCT02233660). J Orthop Sports
CÉSAR FERNÁNDEZ-DE-LAS-PEÑAS, PT, PhD, DMSc1
• JOSHUA CLELAND, PT, PhD, OCS, FAAOMPT2-4
•
STELLA FUENSALIDA-NOVO, PT1
• JUAN A. PAREJA, MD, PhD5
• CRISTINA ALONSO-BL
The Effectiveness of Manual T
Versus Surgery on Self-reported
Cervical Range of Motion, and P
Force in Carpal Tunnel Synd
A Randomized Clinical Tr
ournalofOrthopaedic&SportsPhysicalTherapy®
ownloadedfromwww.jospt.orgatCurtinUniofTechnologyonMarch7,2017.Forpersonaluseonly.Nootheruseswithoutpermission.
opyright©2017JournalofOrthopaedic&SportsPhysicalTherapy®.Allrightsreserved.
[ RESEARCH REPORT ]
C
arpal tunnel synd
(CTS), a pain con
associated with rep
movements, accoun
nearly 50% of all work-r
injuries.31
The prevalence o
in the general population has b
ported to range between 6% and
Individuals diagnosed with CT
been identified as significantly
likely to miss more work day
asymptomatic individuals, which
in a massive economic burden to
dividual and society.2
The management of CTS can b
conservative or surgical. Conse
management is often chosen as t
approach when symptoms are m
STUDY DESIGN: Randomized parallel-group
trial.
BACKGROUND: Carpal tunnel syndrome (CTS)
is a common pain condition that can be managed
surgically or conservatively.
OBJECTIVE: To compare the effectiveness of
manual therapy versus surgery for improving self-
reported function, cervical range of motion, and
pinch-tip grip force in women with CTS.
METHODS: In this randomized clinical trial, 100
women with CTS were randomly allocated to either
a manual therapy (n = 50) or a surgery (n = 50)
group. The primary outcome was self-rated hand
function, assessed with the Boston Carpal Tunnel
Questionnaire. Secondary outcomes included
active cervical range of motion, pinch-tip grip
force, and the symptom severity subscale of the
Boston Carpal Tunnel Questionnaire. Patients were
assessed at baseline and 1, 3, 6, and 12 months
after the last treatment by an assessor unaware
of group assignment. Analysis was by intention to
treat, with mixed analyses of covariance adjusted
for baseline scores.
RESULTS: At 12 months, 94 women completed
the follow-up. Analyses showed statistically sig-
nificant differences in favor of manual therapy at
1 month for self-reported function (mean change,
–0.8; 95% confidence interval [CI]: –1.1, –0.5)
and pinch-tip grip force on the symptomatic side
(thumb-index finger: mean change, 2.0; 95% CI:
1.1, 2.9 and thumb-little finger: mean change, 1.0;
95% CI: 0.5, 1.5). Improvements in self-reported
function and pinch grip force were similar between
the groups at 3, 6, and 12 months. Both groups
reported improvements in symptom severity that
were not significantly different at all follow-up
periods. No significant changes were observed in
pinch-tip grip force on the less symptomatic side
and in cervical range of motion in either group.
CONCLUSION: Manual therapy and surgery had
similar effectiveness for improving self-reported
function, symptom severity, and pinch-tip grip
force on the symptomatic hand in women with
CTS. Neither manual therapy nor surgery resulted
in changes in cervical range of motion.
LEVEL OF EVIDENCE: Therapy, level 1b. Pro-
spectively registered September 3, 2014 at www.
clinicaltrials.gov (NCT02233660). J Orthop Sports
Phys Ther 2017;47(3):151-161. Epub 3 Feb 2017.
doi:10.2519/jospt.2017.7090
KEY WORDS: carpal tunnel syndrome, cervical
spine, force, manual therapy, neck, surgery
CÉSAR FERNÁNDEZ-DE-LAS-PEÑAS, PT, PhD, DMSc1
• JOSHUA CLELAND, PT, PhD, OCS, FAAOMPT2-4
• MARÍA PALACIOS-CEÑA,
STELLA FUENSALIDA-NOVO, PT1
• JUAN A. PAREJA, MD, PhD5
• CRISTINA ALONSO-BLANCO, PT, PhD1
The Effectiveness of Manual Therapy
Versus Surgery on Self-reported Function
Cervical Range of Motion, and Pinch Gri
Force in Carpal Tunnel Syndrome:
A Randomized Clinical Trial
JournalofOrthopaedic&SportsPhysicalTherapy®
Downloadedfromwww.jospt.orgatCurtinUniofTechnologyonMarch7,2017.Forpersonaluseonly.Nootheruseswithoutpermission.
Copyright©2017JournalofOrthopaedic&SportsPhysicalTherapy®.Allrightsreserved.
Mulcmodal manual
therapy effeccve in CTS
6. Neck/arm pain
• RCT 60 Pacents with neck/arm pain
– Randomized to neural mobs + neural ex +
advise (n=40) or control (n=20, stay accve)
– 4 treatment session over 2 weeks
– 4 week follow-up
– GRC, NDI, pain, PSFS
– NNT 2.7 to 4
– Neural mobilizacon provides immediate,
clinically relevant benefits beyond advice
to stay accve
• Nee, Coppieters 2012
• Healthy people
– Increases flexibility
• LBP
– Improves pain & disability
c
CIPER - Universidade de Lisboa, Faculdade de Motricidade Humana, Lisbon, Portugal
d
Escola Superior de Saúde, Instituto Politecnico de Setúbal, Portugal
e
Laboratory “Movement, Interactions, Performance” (EA 4334), University of Nantes, UFR STAPS, Nantes, France
a r t i c l e i n f o
Article history:
Received 18 March 2016
Received in revised form
10 November 2016
Accepted 19 November 2016
Keywords:
Neurodynamics
Peripheral nerves
Slump
Flexibility
Pain
Disability
a b s t r a c t
Background: Neural mobilization (NM) is widely used to assess and treat several neuromuscular disor-
ders. However, information regarding the NM effects targeting the lower body quadrant is scarce.
Objectives: To determine the effects of NM techniques targeting the lower body quadrant in healthy and
low back pain (LBP) populations.
Design: Systematic review with meta-analysis.
Method: Randomized controlled trials were included if any form of NM was applied to the lower body
quadrant. Pain, disability, and lower limb flexibility were the main outcomes. PEDro scale was used to
assess methodological quality.
Results: Forty-five studies were selected for full-text analysis, and ten were included in the meta-
analysis, involving 502 participants. Overall, studies presented fair to good quality, with a mean PEDro
score of 6.3 (from 4 to 8). Five studies used healthy participants, and five targeted people with LBP. A
moderate effect size (g ¼ 0.73, 95% CI: 0.48e0.98) was determined, favoring the use of NM to increase
flexibility in healthy adults. Larger effect sizes were found for the effect of NM in pain reduction (g ¼ 0.82,
95% CI 0.56e1.08) and disability improvement (g ¼ 1.59, 95% CI: 1.14e2.03), in people with LBP.
Conclusion: Evidence suggests that there are positive effects from the application of NM to the lower
body quadrant. Specifically, NM shows moderate effects on flexibility in healthy participants, and large
effects on pain and disability in people with LBP. Nevertheless, more studies with high methodological
quality are necessary to support these conclusions.
© 2016 Elsevier Ltd. All rights reserved.
1. Introduction
Neural mobilization (NM) techniques are widely used to eval-
uate, and improve, the mechanical and neurophysiological integrity
of the peripheral nerves (Shacklock, 1995) in clinical populations
(Butler, 2000). These techniques include combinations of joint
movements that promote either neural tensioning (i.e. through
displacement of the nerve endings in opposite directions) or sliding
(i.e. through displacement of nerve endings in the same direction
(Coppieters et al., 2009). Several studies have successfully used NM
to improve flexibility, in both healthy (Herrington and Lee, 2006)
and clinical populations (Coppieters et al., 2003), and also to induce
different amounts of neural excursion (Coppieters et al., 2015). This
is particularly relevant because it has been reported that nerve
properties (e.g. cross-sectional area) are altered in certain periph-
eral neuropathies (Lee and Dauphinee, 2005), and in upper limb
nerve entrapment syndromes (Hough et al., 2007; Kantarci et al.,
2013). These changes in the nerve properties may be associated
with a compromised nerve function (Li and Shi, 2007; Rickett et al.,
2010). In addition, it has also been shown that people with pe-
ripheral neuropathy have a higher lower body quadrant mecha-
nosensitivity (Boyd et al., 2010). Consequently, the NM techniques
are used as treatment for different neuromuscular disorders.
* Corresponding author. Faculdade de Motricidade Humana, Estrada da Costa,
1499-002, Cruz Quebrada - Dafundo, Universidade de Lisboa, Portugal.
E-mail addresses: netogtiago@gmail.com (T. Neto), sfreitas@fmh.ulisboa.pt
(S.R. Freitas).
http://dx.doi.org/10.1016/j.msksp.2016.11.014
2468-7812/© 2016 Elsevier Ltd. All rights reserved.
12 Research
3 Neurodynamic treatment did not improve pain and disability at two weeks in
4 patients with chronic nerve-related leg pain: a randomised trial
5 Giovanni E Ferreira a
, Fa´bio F Stieven b
, Francisco X Araujo c
, Matheus Wiebusch c
,
6 Carolina G Rosa c
, Rodrigo Della Me´a Plentz d
, Marcelo F Silva d
7 a
Master’s Program in Rehabilitation Sciences, Universidade Federal de Cieˆncias da Sau´de de Porto Alegre; b
Doctoral Program in Health Sciences, Universidade Federal de Cieˆncias da
8 Sau´de de Porto Alegre; c
Universidade Federal de Cieˆncias da Sau´de de Porto Alegre; d
Graduate Program in Rehabilitation Sciences, Universidade Federal de Cieˆncias da Sau´de de Porto
9 Alegre, Porto Alegre, Brazil
Journal of Physiotherapy xxx (2016) xxx–xxx
K E Y W O R D S
Low back pain
Sciatica
Manual therapy
Neurodynamic treatment
Slump test
A B S T R A C T
Question: In people with nerve-related leg pain, does adding neurodynamic treatment to advice to
remain active improve leg pain, disability, low back pain, function, global perceived effect and location of
symptoms?. Design: Randomised trial with concealed allocation and intention-to-treat analysis.
Participants: Sixty participants with nerve-related leg pain recruited from the community.
Interventions: The experimental group received four sessions of neurodynamic treatment. Both
groups received advice to remain active. Outcome measures: Leg pain and low back pain (0 none to
10 worst), Oswestry Disability Index (0 none to 100 worst), Patient-Specific Functional Scale (0 unable to
perform to 30 able to perform), global perceived effect (–5 to 5) and location of symptoms were
measured at 2 and 4 weeks after randomisation. Continuous outcomes were analysed by linear mixed
models. Location of symptoms was assessed by relative risk (95% CI). Results: At 2 weeks, the
experimental group did not have significantly greater improvement that the control group in leg pain
(MD –1.1, 95% CI –2.3 to 0.1) or disability (MD –3.3, 95% CI –9.6 to 2.9). At 4 weeks, the experimental
group experienced a significantly greater reduction in leg pain (MD –2.4, 95% CI –3.6 to –1.2) and low
back pain (MD –1.5, 95% CI –2.8 to –0.2). The experimental group also improved significantly more in
function at 2 weeks (MD 5.2, 95% CI 2.2 to 8.2) and 4 weeks (MD 4.7, 95% CI 1.7 to 7.8), as well as global
perceived effect at 2 weeks (MD 2.5, 95% CI 1.6 to 3.5) and 4 weeks (MD 2.9, 95% CI 1.9 to 3.9). No
significant between-group differences occurred in disability at 4 weeks and location of symptoms.
Conclusion: Adding neurodynamic treatment to advice to remain active did not improve leg pain and
disability at 2 weeks. Trial registration: NCT01954199. [Ferreira GE, Stieven FF, Araujo FX, Wiebusch
M, Rosa CG, Della Me´a Plentz R, et al. (2016) Neurodynamic treatment did not improve pain and
disability at two weeks in patients with chronic nerve-related leg pain: a randomised trial. Journal
of Physiotherapy XX: XX-XX]
ß 2016 Australian Physiotherapy Association. Published by Elsevier B.V. This is an open access article
under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
G Model
JPHYS 275 1–6
Journal of
PHYSIOTHERAPY
journal homepage: www.elsevier.com/locate/jphys
2016
Research
urodynamic treatment did not improve pain and disability at two weeks in
patients with chronic nerve-related leg pain: a randomised trial
Giovanni E Ferreira a
, Fa´bio F Stieven b
, Francisco X Araujo c
, Matheus Wiebusch c
,
Carolina G Rosa c
, Rodrigo Della Me´a Plentz d
, Marcelo F Silva d
Program in Rehabilitation Sciences, Universidade Federal de Cieˆncias da Sau´de de Porto Alegre; b
Doctoral Program in Health Sciences, Universidade Federal de Cieˆncias da
Porto Alegre; c
Universidade Federal de Cieˆncias da Sau´de de Porto Alegre; d
Graduate Program in Rehabilitation Sciences, Universidade Federal de Cieˆncias da Sau´de de Porto
Alegre, Porto Alegre, Brazil
uction
back pain is a highly prevalent and disabling condition that
nts the major cause of years lived with disability in both
ped and developing countries.1
Among the wide array of
presentations, the prevalence of radiating leg pain can be
27treatment.4
Despite the high risk of bias of several included studies,
28as well as moderate-to-high levels of between-study heterogene-
29ity, this network meta-analysis provided evidence that commonly
30used conservative interventions were not capable of altering the
31natural history of leg pain. Therefore, other conservative treatment
32strategies should be investigated in this population as a research
Journal of Physiotherapy xxx (2016) xxx–xxx
W O R D S
k pain
herapy
namic treatment
st
A B S T R A C T
Question: In people with nerve-related leg pain, does adding neurodynamic treatment to advice to
remain active improve leg pain, disability, low back pain, function, global perceived effect and location of
symptoms?. Design: Randomised trial with concealed allocation and intention-to-treat analysis.
Participants: Sixty participants with nerve-related leg pain recruited from the community.
Interventions: The experimental group received four sessions of neurodynamic treatment. Both
groups received advice to remain active. Outcome measures: Leg pain and low back pain (0 none to
10 worst), Oswestry Disability Index (0 none to 100 worst), Patient-Specific Functional Scale (0 unable to
perform to 30 able to perform), global perceived effect (–5 to 5) and location of symptoms were
measured at 2 and 4 weeks after randomisation. Continuous outcomes were analysed by linear mixed
models. Location of symptoms was assessed by relative risk (95% CI). Results: At 2 weeks, the
experimental group did not have significantly greater improvement that the control group in leg pain
(MD –1.1, 95% CI –2.3 to 0.1) or disability (MD –3.3, 95% CI –9.6 to 2.9). At 4 weeks, the experimental
group experienced a significantly greater reduction in leg pain (MD –2.4, 95% CI –3.6 to –1.2) and low
back pain (MD –1.5, 95% CI –2.8 to –0.2). The experimental group also improved significantly more in
function at 2 weeks (MD 5.2, 95% CI 2.2 to 8.2) and 4 weeks (MD 4.7, 95% CI 1.7 to 7.8), as well as global
perceived effect at 2 weeks (MD 2.5, 95% CI 1.6 to 3.5) and 4 weeks (MD 2.9, 95% CI 1.9 to 3.9). No
significant between-group differences occurred in disability at 4 weeks and location of symptoms.
Conclusion: Adding neurodynamic treatment to advice to remain active did not improve leg pain and
disability at 2 weeks. Trial registration: NCT01954199. [Ferreira GE, Stieven FF, Araujo FX, Wiebusch
M, Rosa CG, Della Me´a Plentz R, et al. (2016) Neurodynamic treatment did not improve pain and
disability at two weeks in patients with chronic nerve-related leg pain: a randomised trial. Journal
of Physiotherapy XX: XX-XX]
ß 2016 Australian Physiotherapy Association. Published by Elsevier B.V. This is an open access article
under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
275 1–6
Journal of
PHYSIOTHERAPY
journal homepage: www.elsevier.com/locate/jphys
Conclusion: NM not recommended for the treatment of chronic nerve-
related leg pain!!!!!!!
sample size = 60
4 sessions NM
Summary
Evidence of effect in humans with and without
pain. Pacent seleccon may be a factor, not all
neural disorders suitable?
7. Sub-groups of neural disorders
• Some pacents respond well others not - Why ?
– Sub-groups?
• Schafer, 2008
Compressive neuropathy
sliding
Central sensiczacon
Other
Axonal mechanosensicvity
Musculoskeletal
transverse sliding
Nerve swelling
Neural sub-group classificaEon based on mechanisms
Trauma, compression, or chemical
irritaEon of nerve/nerve roots
Neuropathic
pain sensory
hypersensiEvity
InflammaEon
Peripheral nerve
sensiEsaEon
NegaEve featuresPosiEve features
“Neuropathic”
Compressive
neuropathy
Musculoskeletal
pain
DeafferentaEon, loss of inhibiEon,
facilitaEon etc
AMS or nervi nervorum
sensiEzaEon
If none
Convergence
Axonal damage
Neuropathic Mixed
Inflammatory
Mechanism?
Hall, 2011
Classification of Neural Pain
• Syndrome based classification
Peripheral neural pain
DN, PHN, MS, radiculopathy, CTS, CUTS
• Mechanism based classification
Aß
C
Dorsal root
ganglion
Dorsal horn
midline
Woolf, 1999
Central mechanism
Peripheral mechanism
Classification by syndrome
• Does not explain pain
• Does not help treatment
– Patients with similar
diagnoses have diverse
symptoms
– Resolution of the
pathology does not always
improve the disorder
9. Treatment - PNS
• Responders to neural mobilization
– Positive LANSS, age, large ROM deficits on median
nerve neurodynamic tests predict 10% chance of
recovery
– Negative LANSS, age, small ROM deficits predicts
90% chance of recovery
• Nee, Coppieters et al 2013
Original Research Article
Cervical Lateral Glide Neural Mobilization Is
Effective in Treating Cervicobrachial Pain: A
Randomized Waiting List Controlled Clinical
Trial
David Rodrıguez-Sanz, PhD, PT, DP,* Ce´sar
Calvo-Lobo, PhD, PT,†
Francisco Unda-Solano,
MSc, PT,* Irene Sanz-Corbalan, PhD, DP,‡
Carlos Romero-Morales, PhD, PT,* and
Daniel Lopez-Lopez, PhD, DP§
*Faculty of Health, Exercise and Sport, Department of
Physical Therapy and Podiatry, Physical Therapy
Health Sciences Research group, Universidad
Europea de Madrid, Villaviciosa de Odon, Madrid,
Spain; †
Department of Physical Therapy, School of
Health Sciences, University of Leon, Ponferrada,
Leon, Spain; ‡
Podiatry, Nursing and Physical Therapy
Department, Universidad Complutense de Madrid,
Madrid, Spain; §
Research, Health and Podiatry Unit,
Department of Health Sciences, Faculty of Nursing
and Podiatry, Universidade da Coru~na, Coru~na, Spain
Correspondence to: Ce´sar Calvo Lobo, PhD, MSc, PT
Nursing and Physical Therapy Department, Faculty of
Health Sciences, University of Leon, Av. Astorga, s/n,
24401 Ponferrada, Leon, Spain (e-mail: cecalvo19@
hotmail.com). Tel: 912-115-268, ext. 5268.
Funding sources: None.
Conflicts of interest: All authors have no conflicts of
interest to report. None of the authors of the manu-
script received any remuneration. Further, the authors
have not received any reimbursement or honorarium
in any other manner. The authors are not affiliated in
any manner.
Ethics committee board approval review of study
protocol: The “Centro Policlinico Valencia” Research
Ethics Committe approved the study (CE0072015).
Public trial registry: Registered at Clinical Trials
NCT02595294.
Trial registration: NCT02595294.
Abstract
Background. Cervicobrachial pain (CP) is a high-
incidence and prevalent condition. Cervical lateral
glide (CLG) is a firstline treatment of CP. There is a cur-
rent lack of enough high-quality randomized controlled
double-blind clinical trials that measure the effective-
ness of neural tissue mobilization techniques such as
the CLG and its specific effect over CP.
Objectives. The aim of the present study was to as-
sess the effect of CLG neural mobilization in treat-
ing subjects who suffer from CP, compared with the
complete absence of treatment.
Study Design. This investigation was a single-
center, blinded, parallel randomized controlled clin-
ical trial (RCT).
Setting. One hundred forty-seven individuals were
screened in a medical center from July to November
2015. Fifty-eight participants were diagnosed with CP.
Methods. Participants were recruited and randomly
assigned into two groups of 29 subjects. The inter-
vention group received CLG treatment, and the
control group (CG) was assigned to a six-week
waiting list to receive treatment. Randomization
was carried out by concealed computer software
randomized printed cards. The primary outcome
was pain intensity, reported through the Numeric
Rating Scale for Pain (NRSP). Secondary outcomes
were physical function involving the affected upper
limb using the Quick DASH scale and ipsilateral
cervical rotation (ICR) using a CROM device.
Assessments were made at baseline and one hour
after treatment.
Results. The CLG group NRSP mean value was sig-
nificantly (P 0.0001) superior to those obtained by
the CG. Subjects treated with CLG reported an
VC 2017 American Academy of Pain Medicine. All rights reserved. For permissions, please e-mail: journals.permissions@oup.com 1
Pain Medicine 2017; 00: 1–12
doi: 10.1093/pm/pnx011
Original Research Article
Cervical Lateral Glide Neural Mobilization Is
Effective in Treating Cervicobrachial Pain: A
Randomized Waiting List Controlled Clinical
Trial
David Rodrıguez-Sanz, PhD, PT, DP,* Ce´sar
Calvo-Lobo, PhD, PT,†
Francisco Unda-Solano,
MSc, PT,* Irene Sanz-Corbalan, PhD, DP,‡
Carlos Romero-Morales, PhD, PT,* and
Daniel Lopez-Lopez, PhD, DP§
*Faculty of Health, Exercise and Sport, Department of
Physical Therapy and Podiatry, Physical Therapy
Health Sciences Research group, Universidad
Europea de Madrid, Villaviciosa de Odon, Madrid,
Spain; †
Department of Physical Therapy, School of
Health Sciences, University of Leon, Ponferrada,
Leon, Spain; ‡
Podiatry, Nursing and Physical Therapy
Department, Universidad Complutense de Madrid,
Madrid, Spain; §
Research, Health and Podiatry Unit,
Department of Health Sciences, Faculty of Nursing
and Podiatry, Universidade da Coru~na, Coru~na, Spain
Correspondence to: Ce´sar Calvo Lobo, PhD, MSc, PT
Nursing and Physical Therapy Department, Faculty of
Health Sciences, University of Leon, Av. Astorga, s/n,
24401 Ponferrada, Leon, Spain (e-mail: cecalvo19@
hotmail.com). Tel: 912-115-268, ext. 5268.
Funding sources: None.
Conflicts of interest: All authors have no conflicts of
interest to report. None of the authors of the manu-
script received any remuneration. Further, the authors
have not received any reimbursement or honorarium
in any other manner. The authors are not affiliated in
any manner.
Ethics committee board approval review of study
protocol: The “Centro Policlinico Valencia” Research
Ethics Committe approved the study (CE0072015).
Public trial registry: Registered at Clinical Trials
NCT02595294.
Trial registration: NCT02595294.
Abstract
Background. Cervicobrachial pain (CP) is a high-
incidence and prevalent condition. Cervical lateral
glide (CLG) is a firstline treatment of CP. There is a cur-
rent lack of enough high-quality randomized controlled
double-blind clinical trials that measure the effective-
ness of neural tissue mobilization techniques such as
the CLG and its specific effect over CP.
Objectives. The aim of the present study was to as-
sess the effect of CLG neural mobilization in treat-
ing subjects who suffer from CP, compared with the
complete absence of treatment.
Study Design. This investigation was a single-
center, blinded, parallel randomized controlled clin-
ical trial (RCT).
Setting. One hundred forty-seven individuals were
screened in a medical center from July to November
2015. Fifty-eight participants were diagnosed with CP.
Methods. Participants were recruited and randomly
assigned into two groups of 29 subjects. The inter-
vention group received CLG treatment, and the
control group (CG) was assigned to a six-week
waiting list to receive treatment. Randomization
was carried out by concealed computer software
randomized printed cards. The primary outcome
was pain intensity, reported through the Numeric
Rating Scale for Pain (NRSP). Secondary outcomes
were physical function involving the affected upper
limb using the Quick DASH scale and ipsilateral
cervical rotation (ICR) using a CROM device.
Assessments were made at baseline and one hour
after treatment.
Results. The CLG group NRSP mean value was sig-
nificantly (P 0.0001) superior to those obtained by
the CG. Subjects treated with CLG reported an
VC 2017 American Academy of Pain Medicine. All rights reserved. For permissions, please e-mail: journals.permissions@oup.com 1
Pain Medicine 2017; 00: 1–12
doi: 10.1093/pm/pnx011
Original Research Article
Cervical Lateral Glide Neural Mobilization Is
Effective in Treating Cervicobrachial Pain: A
Randomized Waiting List Controlled Clinical
Trial
David Rodrıguez-Sanz, PhD, PT, DP,* Ce´sar
Calvo-Lobo, PhD, PT,†
Francisco Unda-Solano,
MSc, PT,* Irene Sanz-Corbalan, PhD, DP,‡
Carlos Romero-Morales, PhD, PT,* and
Daniel Lopez-Lopez, PhD, DP§
*Faculty of Health, Exercise and Sport, Department of
Physical Therapy and Podiatry, Physical Therapy
Health Sciences Research group, Universidad
Europea de Madrid, Villaviciosa de Odon, Madrid,
Spain; †
Department of Physical Therapy, School of
Health Sciences, University of Leon, Ponferrada,
Leon, Spain; ‡
Podiatry, Nursing and Physical Therapy
Department, Universidad Complutense de Madrid,
Madrid, Spain; §
Research, Health and Podiatry Unit,
Department of Health Sciences, Faculty of Nursing
and Podiatry, Universidade da Coru~na, Coru~na, Spain
Correspondence to: Ce´sar Calvo Lobo, PhD, MSc, PT
Nursing and Physical Therapy Department, Faculty of
Health Sciences, University of Leon, Av. Astorga, s/n,
24401 Ponferrada, Leon, Spain (e-mail: cecalvo19@
hotmail.com). Tel: 912-115-268, ext. 5268.
Funding sources: None.
Conflicts of interest: All authors have no conflicts of
interest to report. None of the authors of the manu-
script received any remuneration. Further, the authors
have not received any reimbursement or honorarium
in any other manner. The authors are not affiliated in
any manner.
Ethics committee board approval review of study
protocol: The “Centro Policlinico Valencia” Research
Ethics Committe approved the study (CE0072015).
Public trial registry: Registered at Clinical Trials
NCT02595294.
Abstract
Background. Cervicobrachial pain (CP) is a high-
incidence and prevalent condition. Cervical lateral
glide (CLG) is a firstline treatment of CP. There is a cur-
rent lack of enough high-quality randomized controlled
double-blind clinical trials that measure the effective-
ness of neural tissue mobilization techniques such as
the CLG and its specific effect over CP.
Objectives. The aim of the present study was to as-
sess the effect of CLG neural mobilization in treat-
ing subjects who suffer from CP, compared with the
complete absence of treatment.
Study Design. This investigation was a single-
center, blinded, parallel randomized controlled clin-
ical trial (RCT).
Setting. One hundred forty-seven individuals were
screened in a medical center from July to November
2015. Fifty-eight participants were diagnosed with CP.
Methods. Participants were recruited and randomly
assigned into two groups of 29 subjects. The inter-
vention group received CLG treatment, and the
control group (CG) was assigned to a six-week
waiting list to receive treatment. Randomization
was carried out by concealed computer software
randomized printed cards. The primary outcome
was pain intensity, reported through the Numeric
Rating Scale for Pain (NRSP). Secondary outcomes
were physical function involving the affected upper
limb using the Quick DASH scale and ipsilateral
cervical rotation (ICR) using a CROM device.
Assessments were made at baseline and one hour
after treatment.
Results. The CLG group NRSP mean value was sig-
nificantly (P 0.0001) superior to those obtained by
Pain Medicine 2017; 00: 1–12
doi: 10.1093/pm/pnx011
Open Journal of Therapy and Rehabilitation, 2016, 4, 132-145
Published Online August 2016 in SciRes. http://www.scirp.org/journal/ojtr
http://dx.doi.org/10.4236/ojtr.2016.43012
How to cite this paper: Salt, E., Kelly, S. and Soundy, A. (2016) Randomised Controlled Trial for the Efficacy of Cervical Lat-
eral Glide Mobilisation in the Management of Cervicobrachial Pain. Open Journal of Therapy and Rehabilitation, 4, 132-145.
http://dx.doi.org/10.4236/ojtr.2016.43012
Randomised Controlled Trial for the Efficacy
of Cervical Lateral Glide Mobilisation in the
Management of Cervicobrachial Pain
Emma Salt1*, Sue Kelly2, Andrew Soundy2
1
Physiotherapy Department, Queen’s Hospital Foundation Trust, Burton on Trent, UK
2
School of Sport, Exercise and Rehabilitation Sciences, The University of Birmingham, Birmingham, UK
Received 26 May 2016; accepted 31 July 2016; published 3 August 2016
Copyright © 2016 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/
Abstract
Objectives: To investigate the long-term efficacy of lateral glide mobilisation for patients with
chronic Cervicobrachial Pain (CP). Methods: A randomised controlled trial which involved ninety-
nine participants with chronic CP. Participants were randomised to receive either the lateral glide
with self-management (n = 49) or self-management alone (n = 50). Four assessments were made
(at baseline and 6, 26 and 52 weeks post intervention). The primary outcome measure was the
Visual Analogue Scale (VAS) for pain. Patient perceived recovery used the Global Rating of Change
score (GROC). Functional outcomes included the Neck and Upper Limb Index score (NULI) and the
Short-From 36 (SF36). Costs and reported number of harmful effects in response to intervention
were evaluated. An intention to treat approach was followed for data analysis. Results: No statis-
tically significant between-group differences were found for pain (using VAS) in the short-term at
six weeks (p = 0.52; 95% CI −14.72 to 7.44) or long-term at one year (p = 0.37; 95% CI −17.76 to
6.61) post-intervention. The VAS outcomes correlated well with GROC scores (p 0.001). There
was a statistically significant difference in NULI scores favouring self-management alone (p =
0.03), but no between-group differences for SF36 (p = 0.07). The cost of providing lateral glide and
self-management was twice that of providing self-management alone. Minor harm was reported in
both groups, with 11% more harm being associated with the lateral glide. Conclusion: In patients
with chronic CP, the addition of a lateral-glide mobilization to a self-management program did not
produce improved outcomes and resulted in higher health-care costs.
Keywords
Cervical Radiculopathy, Physiotherapy, Manual Therapy
*
Corresponding author.
http://dx.doi.org/10.4236/ojtr.2016.43012
How to cite this paper: Salt, E., Kelly, S. and Soundy, A. (2016) Randomised Controlled Trial for the Efficacy of Cervical Lat-
eral Glide Mobilisation in the Management of Cervicobrachial Pain. Open Journal of Therapy and Rehabilitation, 4, 132-145.
http://dx.doi.org/10.4236/ojtr.2016.43012
Randomised Controlled Trial for the Efficacy
of Cervical Lateral Glide Mobilisation in the
Management of Cervicobrachial Pain
Emma Salt1*, Sue Kelly2, Andrew Soundy2
1
Physiotherapy Department, Queen’s Hospital Foundation Trust, Burton on Trent, UK
2
School of Sport, Exercise and Rehabilitation Sciences, The University of Birmingham, Birmingham, UK
Received 26 May 2016; accepted 31 July 2016; published 3 August 2016
Copyright © 2016 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/
Abstract
Objectives: To investigate the long-term efficacy of lateral glide mobilisation for patients with
chronic Cervicobrachial Pain (CP). Methods: A randomised controlled trial which involved ninety-
nine participants with chronic CP. Participants were randomised to receive either the lateral glide
with self-management (n = 49) or self-management alone (n = 50). Four assessments were made
(at baseline and 6, 26 and 52 weeks post intervention). The primary outcome measure was the
Visual Analogue Scale (VAS) for pain. Patient perceived recovery used the Global Rating of Change
score (GROC). Functional outcomes included the Neck and Upper Limb Index score (NULI) and the
Short-From 36 (SF36). Costs and reported number of harmful effects in response to intervention
were evaluated. An intention to treat approach was followed for data analysis. Results: No statis-
tically significant between-group differences were found for pain (using VAS) in the short-term at
six weeks (p = 0.52; 95% CI −14.72 to 7.44) or long-term at one year (p = 0.37; 95% CI −17.76 to
6.61) post-intervention. The VAS outcomes correlated well with GROC scores (p 0.001). There
was a statistically significant difference in NULI scores favouring self-management alone (p =
0.03), but no between-group differences for SF36 (p = 0.07). The cost of providing lateral glide and
self-management was twice that of providing self-management alone. Minor harm was reported in
both groups, with 11% more harm being associated with the lateral glide. Conclusion: In patients
with chronic CP, the addition of a lateral-glide mobilization to a self-management program did not
produce improved outcomes and resulted in higher health-care costs.
Keywords
Cervical Radiculopathy, Physiotherapy, Manual Therapy
*
Corresponding author.
Open Journal of Therapy and Rehabilitation, 2016, 4, 132-145
Published Online August 2016 in SciRes. http://www.scirp.org/journal/ojtr
http://dx.doi.org/10.4236/ojtr.2016.43012
Randomised Controlled Trial for the Efficac
of Cervical Lateral Glide Mobilisation in the
Management of Cervicobrachial Pain
Emma Salt1*, Sue Kelly2, Andrew Soundy2
1
Physiotherapy Department, Queen’s Hospital Foundation Trust, Burton on Trent, UK
2
School of Sport, Exercise and Rehabilitation Sciences, The University of Birmingham, Birmingham, UK
Received 26 May 2016; accepted 31 July 2016; published 3 August 2016
Copyright © 2016 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/
Abstract
Objectives: To investigate the long-term efficacy of lateral glide mobilisation for patients w
chronic Cervicobrachial Pain (CP). Methods: A randomised controlled trial which involved nin
nine participants with chronic CP. Participants were randomised to receive either the lateral g
with self-management (n = 49) or self-management alone (n = 50). Four assessments were m
(at baseline and 6, 26 and 52 weeks post intervention). The primary outcome measure was
Visual Analogue Scale (VAS) for pain. Patient perceived recovery used the Global Rating of Cha
score (GROC). Functional outcomes included the Neck and Upper Limb Index score (NULI) and
Short-From 36 (SF36). Costs and reported number of harmful effects in response to intervent
were evaluated. An intention to treat approach was followed for data analysis. Results: No sta
tically significant between-group differences were found for pain (using VAS) in the short-term
six weeks (p = 0.52; 95% CI −14.72 to 7.44) or long-term at one year (p = 0.37; 95% CI −17.7
6.61) post-intervention. The VAS outcomes correlated well with GROC scores (p 0.001). Th
was a statistically significant difference in NULI scores favouring self-management alone (
0.03), but no between-group differences for SF36 (p = 0.07). The cost of providing lateral glide
self-management was twice that of providing self-management alone. Minor harm was reporte
both groups, with 11% more harm being associated with the lateral glide. Conclusion: In patie
with chronic CP, the addition of a lateral-glide mobilization to a self-management program did
produce improved outcomes and resulted in higher health-care costs.
Keywords
Open Journal of Therapy and Rehabilitation, 2016, 4, 132-145
Published Online August 2016 in SciRes. http://www.scirp.org/journal/ojtr
http://dx.doi.org/10.4236/ojtr.2016.43012
How to cite this paper: Salt, E., Kelly, S. and Soundy, A. (2016) Randomised Controlled Trial for the Efficacy of Cervical Lat-
eral Glide Mobilisation in the Management of Cervicobrachial Pain. Open Journal of Therapy and Rehabilitation, 4, 132-145.
http://dx.doi.org/10.4236/ojtr.2016.43012
Randomised Controlled Trial for the Efficacy
of Cervical Lateral Glide Mobilisation in the
Management of Cervicobrachial Pain
Emma Salt1*, Sue Kelly2, Andrew Soundy2
1
Physiotherapy Department, Queen’s Hospital Foundation Trust, Burton on Trent, UK
2
School of Sport, Exercise and Rehabilitation Sciences, The University of Birmingham, Birmingham, UK
Received 26 May 2016; accepted 31 July 2016; published 3 August 2016
Copyright © 2016 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/
Abstract
Objectives: To investigate the long-term efficacy of lateral glide mobilisation for patients with
chronic Cervicobrachial Pain (CP). Methods: A randomised controlled trial which involved ninety-
nine participants with chronic CP. Participants were randomised to receive either the lateral glide
with self-management (n = 49) or self-management alone (n = 50). Four assessments were made
(at baseline and 6, 26 and 52 weeks post intervention). The primary outcome measure was the
Visual Analogue Scale (VAS) for pain. Patient perceived recovery used the Global Rating of Change
score (GROC). Functional outcomes included the Neck and Upper Limb Index score (NULI) and the
Short-From 36 (SF36). Costs and reported number of harmful effects in response to intervention
were evaluated. An intention to treat approach was followed for data analysis. Results: No statis-
tically significant between-group differences were found for pain (using VAS) in the short-term at
six weeks (p = 0.52; 95% CI −14.72 to 7.44) or long-term at one year (p = 0.37; 95% CI −17.76 to
6.61) post-intervention. The VAS outcomes correlated well with GROC scores (p 0.001). There
was a statistically significant difference in NULI scores favouring self-management alone (p =
0.03), but no between-group differences for SF36 (p = 0.07). The cost of providing lateral glide and
self-management was twice that of providing self-management alone. Minor harm was reported in
both groups, with 11% more harm being associated with the lateral glide. Conclusion: In patients
with chronic CP, the addition of a lateral-glide mobilization to a self-management program did not
produce improved outcomes and resulted in higher health-care costs.
Keywords
Cervical Radiculopathy, Physiotherapy, Manual Therapy
*
Corresponding author.
• Issues:
– C5/6 only
– CBP, not specific PNS
– Did not target neural
cssue
– Did not progress
– Did not eliminate
+ve LANSS
– Max 6 Rx sessions
over 6/52!
– 3 x 60 seconds
How to cite this paper: Salt, E., Kelly, S. and Soundy, A. (2016) Randomised Controlled Trial for the Efficacy of Cervical Lat-
eral Glide Mobilisation in the Management of Cervicobrachial Pain. Open Journal of Therapy and Rehabilitation, 4, 132-145.
http://dx.doi.org/10.4236/ojtr.2016.43012
of Cervical Lateral Glide Mobilisation in the
Management of Cervicobrachial Pain
Emma Salt1*, Sue Kelly2, Andrew Soundy2
1
Physiotherapy Department, Queen’s Hospital Foundation Trust, Burton on Trent, UK
2
School of Sport, Exercise and Rehabilitation Sciences, The University of Birmingham, Birmingham, UK
Received 26 May 2016; accepted 31 July 2016; published 3 August 2016
Copyright © 2016 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/
Abstract
Objectives: To investigate the long-term efficacy of lateral glide mobilisation for patients with
chronic Cervicobrachial Pain (CP). Methods: A randomised controlled trial which involved ninety-
nine participants with chronic CP. Participants were randomised to receive either the lateral glide
with self-management (n = 49) or self-management alone (n = 50). Four assessments were made
(at baseline and 6, 26 and 52 weeks post intervention). The primary outcome measure was the
Visual Analogue Scale (VAS) for pain. Patient perceived recovery used the Global Rating of Change
score (GROC). Functional outcomes included the Neck and Upper Limb Index score (NULI) and the
Short-From 36 (SF36). Costs and reported number of harmful effects in response to intervention
were evaluated. An intention to treat approach was followed for data analysis. Results: No statis-
tically significant between-group differences were found for pain (using VAS) in the short-term at
six weeks (p = 0.52; 95% CI −14.72 to 7.44) or long-term at one year (p = 0.37; 95% CI −17.76 to
6.61) post-intervention. The VAS outcomes correlated well with GROC scores (p 0.001). There
was a statistically significant difference in NULI scores favouring self-management alone (p =
0.03), but no between-group differences for SF36 (p = 0.07). The cost of providing lateral glide and
self-management was twice that of providing self-management alone. Minor harm was reported in
both groups, with 11% more harm being associated with the lateral glide. Conclusion: In patients
with chronic CP, the addition of a lateral-glide mobilization to a self-management program did not
produce improved outcomes and resulted in higher health-care costs.
Keywords
Cervical Radiculopathy, Physiotherapy, Manual Therapy
*
Corresponding author.
Summary
Neural mobilisacon is likely to be more
effeccve for PNS, with a negacve LANSS
Slider or tensioner?
• Inflammacon blocks axoplasmic
transport
• C fiber axonal mechanical
sensicvity distal to
inflammacon
– 1 week maximum sensicvity
(18% of axons)
– 4 weeks (12%) 8 weeks (2%)
• Important for treatment?
Dilley, 2008b
Dilley, 2008
10. Relevance to intervencon?
• How to resolve axonal mechanical sensitivity?
– “Tensioners”
• Raise intraneural pressure reduce
axoplasmic flow
• Increased nerve conduction failure, Sodium
channel block (CTS)
• Gianneschi, 2015
• 3% change in length triggers ectopic impulse
generation
– “Sliders”
• Minimal change in length intraneural
pressure but greater excursion of the nerve
• promotes de-sensitization
What about compressive neuropathy?
Song, 2007
Equivalent in Humans
• Case series
– lumbar spinal stenosis n=57
– Distraction manipulation
neural mobilization + exercise
– Mean 13 treatments (2-50)
– Clinically meaningful
improvement in pain
disability after treatment and
long-term follow-up
• Murphy, 2006