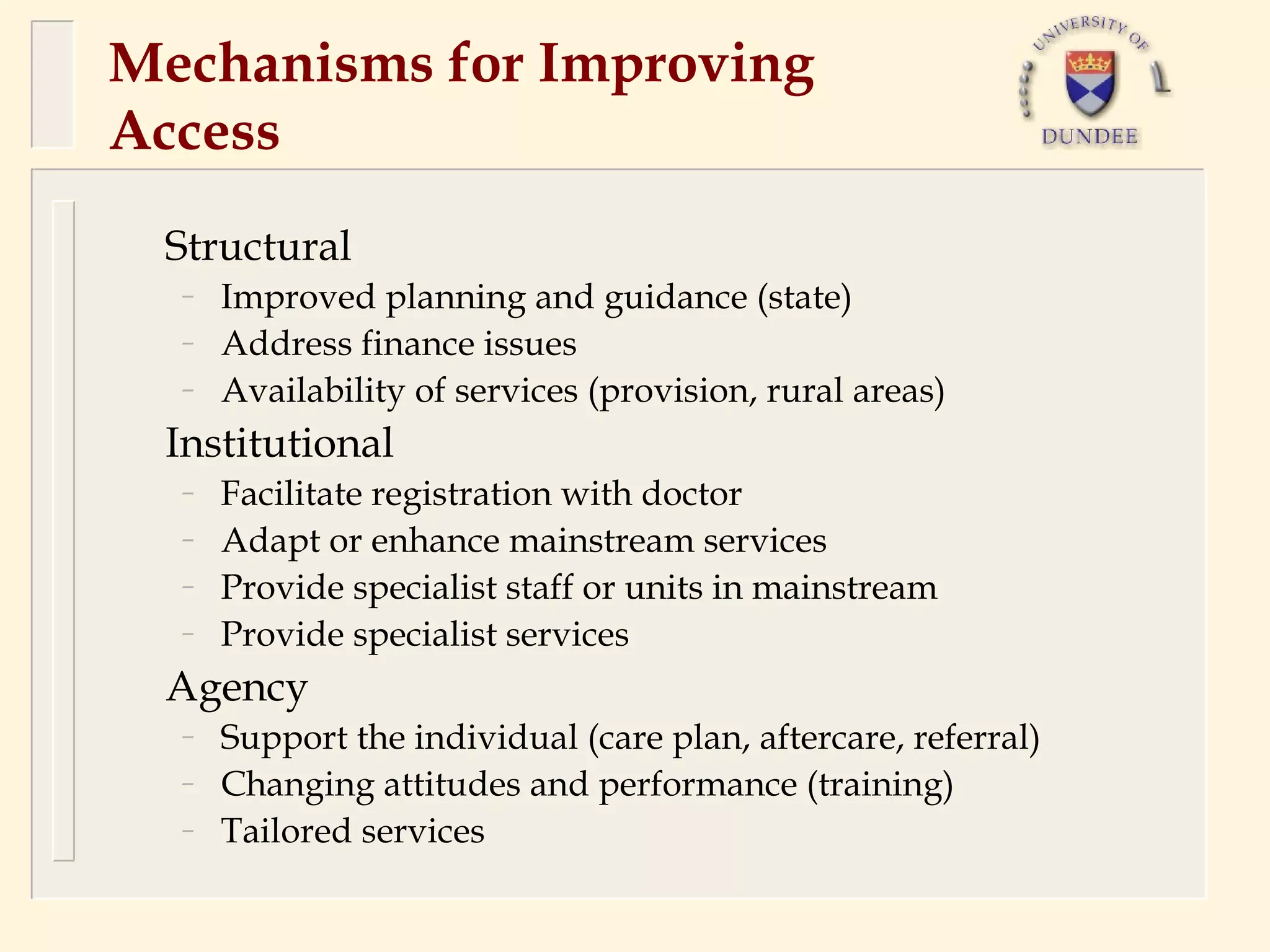
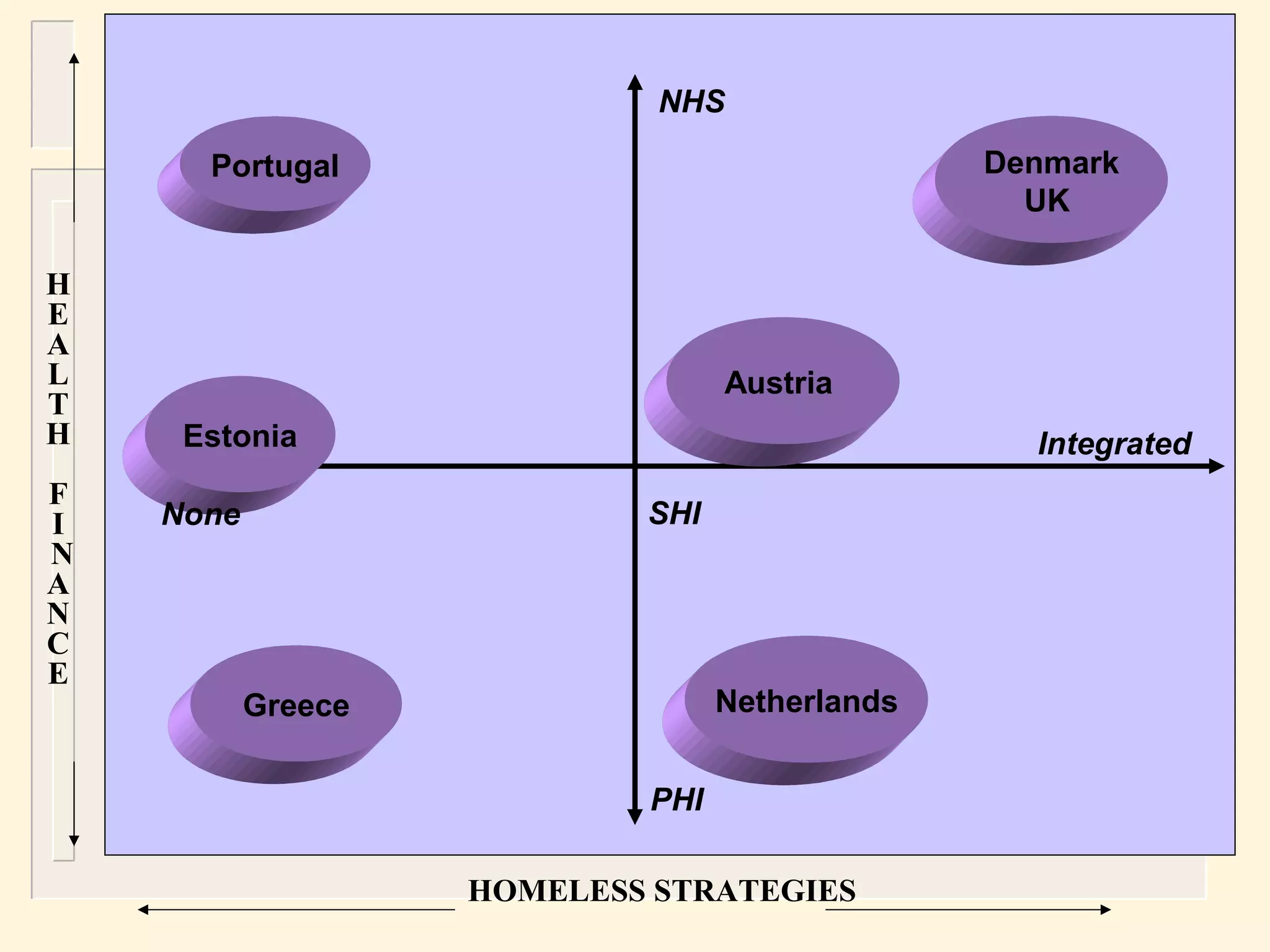
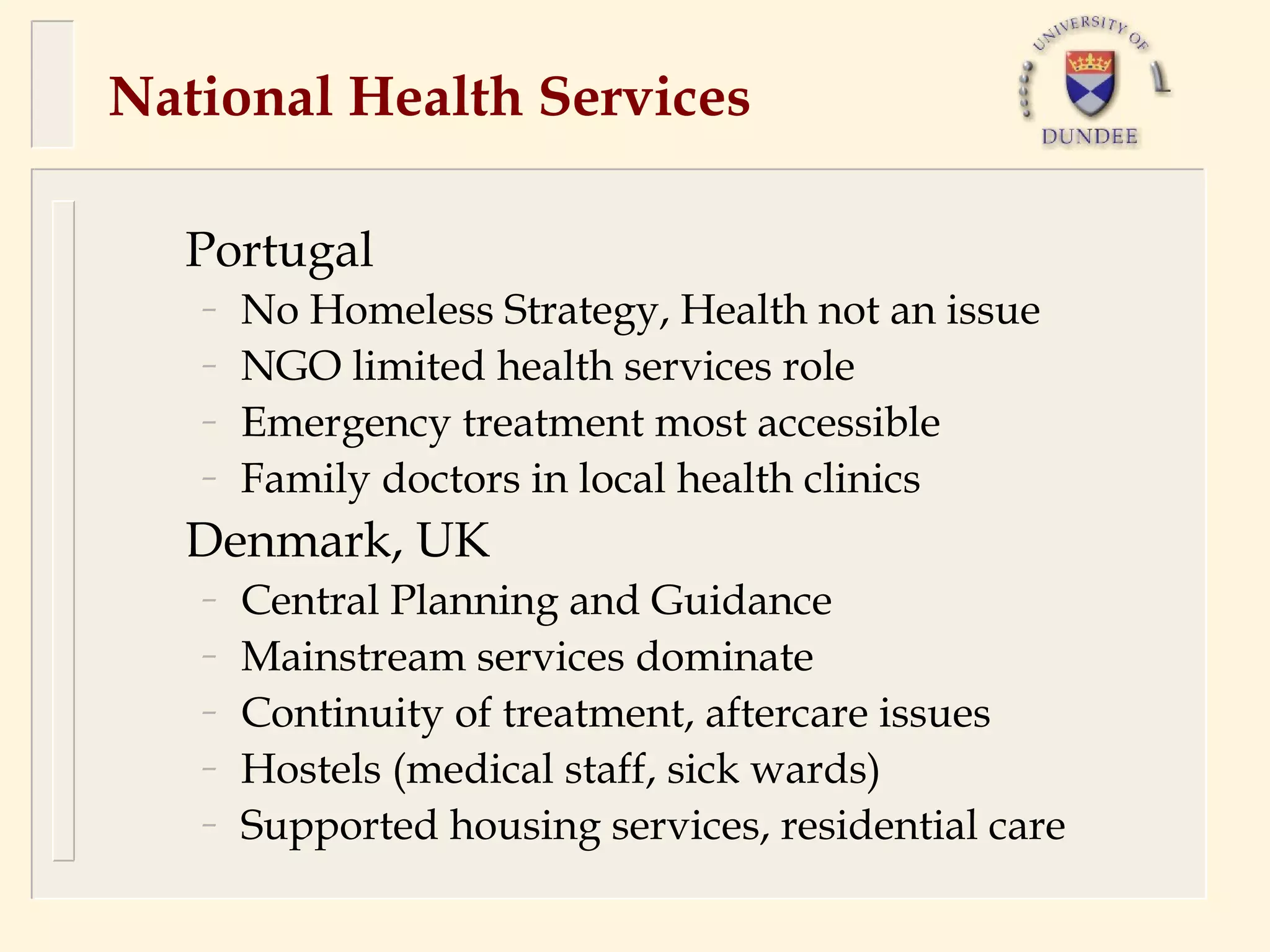
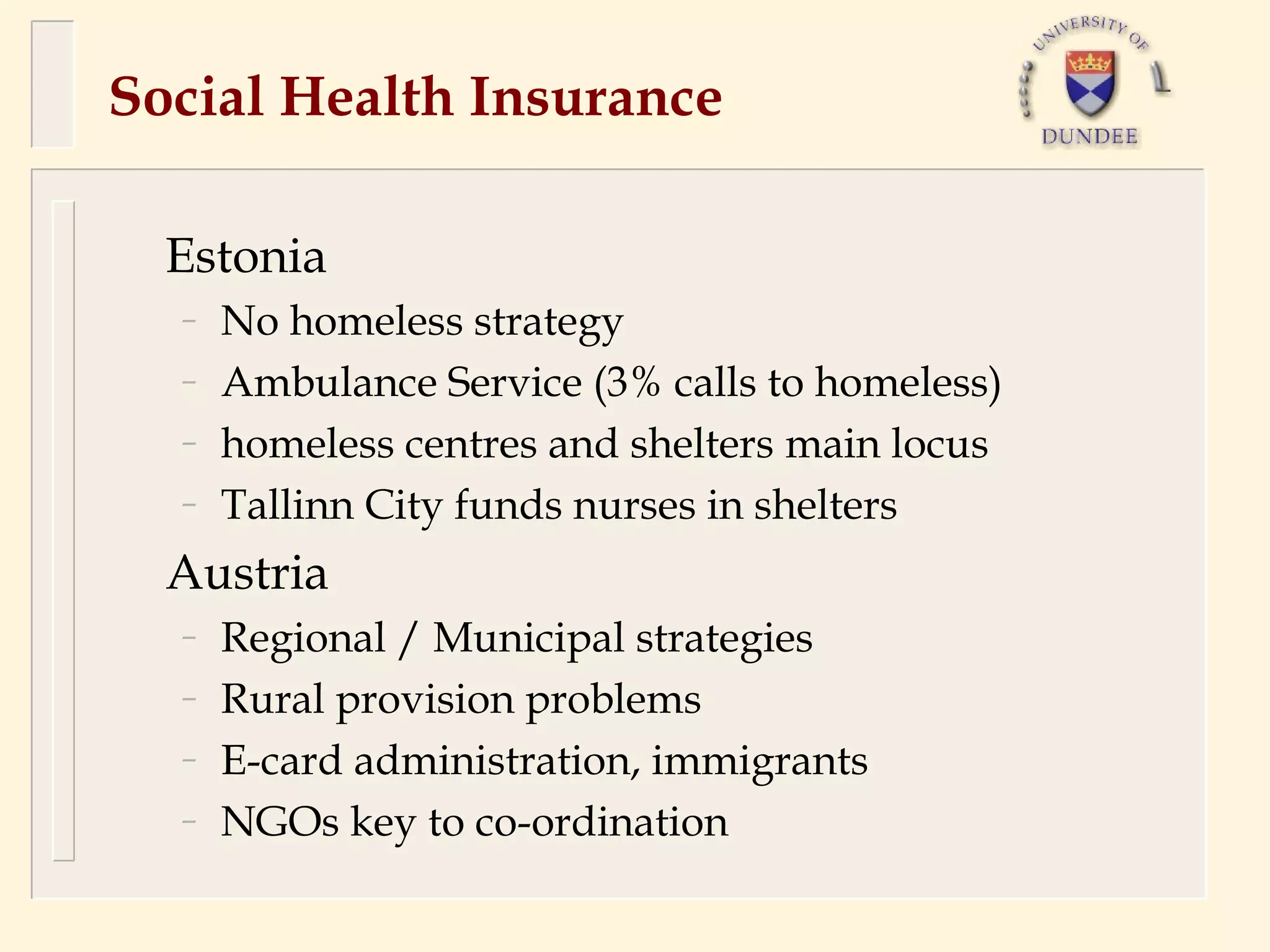
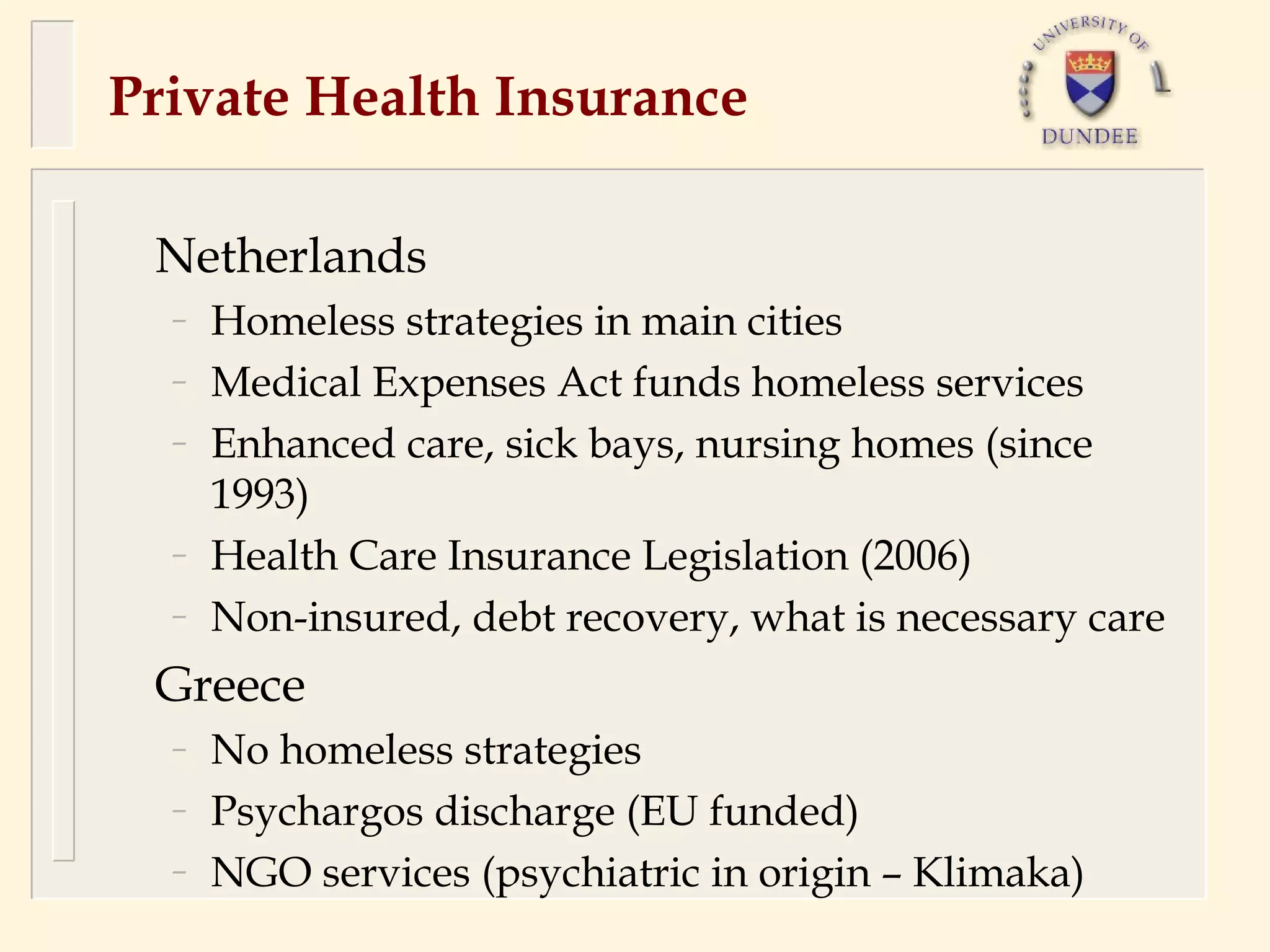
The document discusses access barriers to health services for homeless individuals across Europe, highlighting various health needs and challenges, such as mental health issues and substance abuse. It examines factors contributing to homelessness, including structural poverty and institutional experiences, as well as identifying policy responses aimed at enhancing service accessibility and support. A comparative analysis of health service strategies in different European countries reveals varied approaches and challenges faced by homeless populations in accessing healthcare.