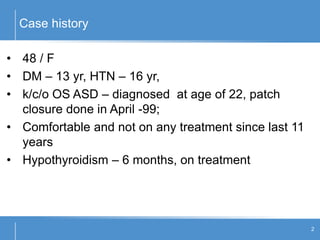
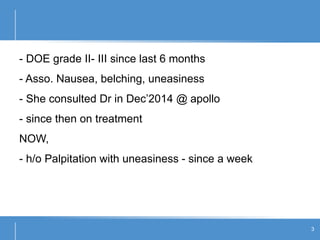
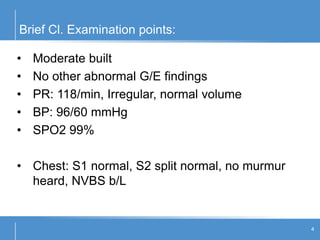
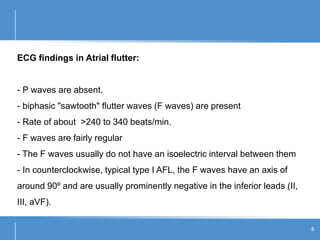
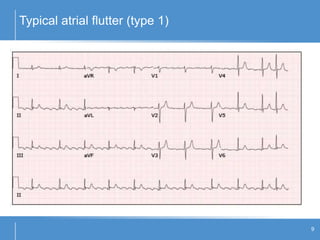
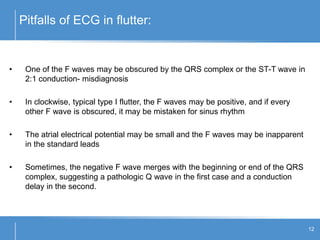
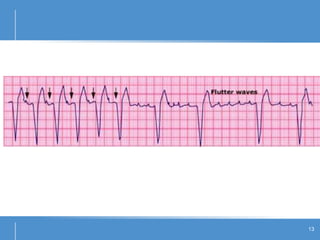
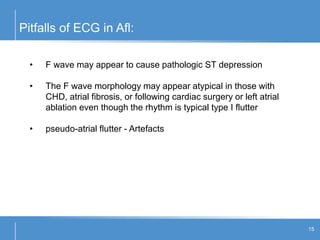
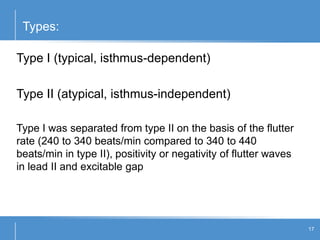
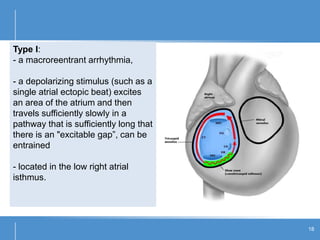
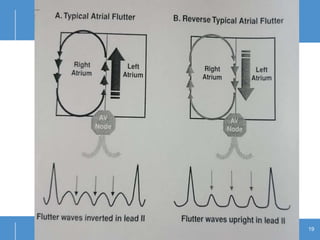
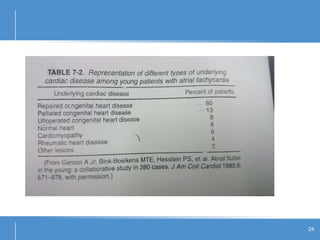
Atrial flutter (AFL) is an uncommon arrhythmia characterized by rapid, regular atrial depolarizations, primarily classified into type I (typical) and type II (atypical) based on flutter rates and formation locations. The diagnosis involves ECG analysis to detect flutter waves and potential pitfalls leading to misdiagnosis, while treatment focuses on restoring normal sinus rhythm through cardioversion, rate control, and ablation strategies. Prognosis varies, with recurrence rates being high and maintaining sinus rhythm often challenging due to structural heart changes and underlying conditions.