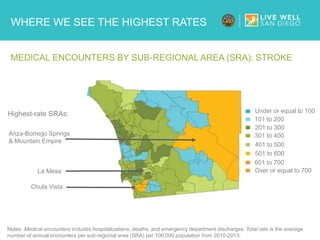
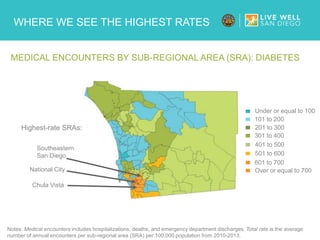
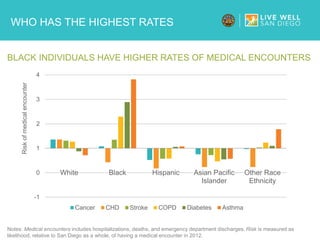
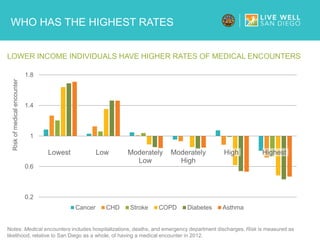
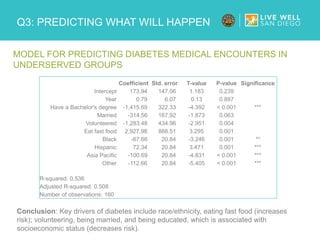
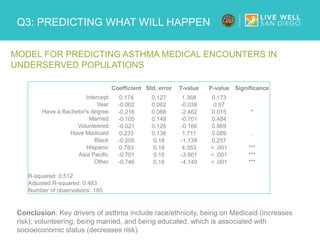
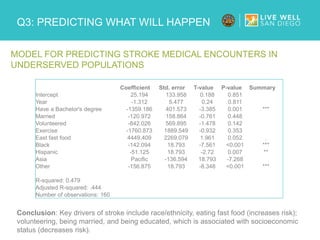
This document presents an analysis from MBA students at the UCSD Rady School of Management, focusing on health disparities in San Diego, particularly looking at medical encounter rates across various demographics and sub-regions. It identifies significant trends and predictors of disease incidence, emphasizing the importance of factors like race, income, education, and lifestyle behaviors in underserved communities. The report concludes with recommendations for addressing these disparities through improved health behaviors and socioeconomic support.