CHRONIC KIDNEY DISEASE.docx
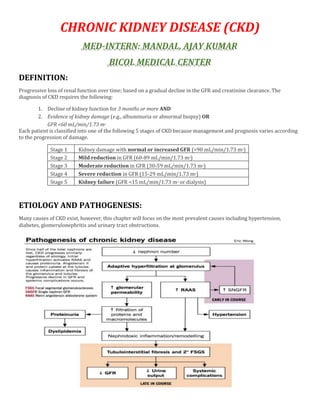
- 1. CHRONIC KIDNEY DISEASE (CKD) MED-INTERN: MANDAL, AJAY KUMAR BICOL MEDICAL CENTER DEFINITION: Progressive loss of renal function over time; based on a gradual decline in the GFR and creatinine clearance. The diagnosis of CKD requires the following: 1. Decline of kidney function for 3 months or more AND 2. Evidence of kidney damage (e.g., albuminuria or abnormal biopsy) OR GFR <60 mL/min/1.73 m2 Each patient is classified into one of the following 5 stages of CKD because management and prognosis varies according to the progression of damage. Stage 1 Kidney damage with normal or increased GFR (>90 mL/min/1.73 m2) Stage 2 Mild reduction in GFR (60-89 mL/min/1.73 m2) Stage 3 Moderate reduction in GFR (30-59 mL/min/1.73 m2) Stage 4 Severe reduction in GFR (15-29 mL/min/1.73 m2) Stage 5 Kidney failure (GFR <15 mL/min/1.73 m2 or dialysis) ETIOLOGY AND PATHOGENESIS: Many causes of CKD exist, however, this chapter will focus on the most prevalent causes including hypertension, diabetes, glomerulonephritis and urinary tract obstructions.
- 2. HYPERTENSION Glomerular and vascular changes: o Elevated systemic blood pressures cause a hypertrophic response leading to intimal thickening of the large and the small vasculature. o The mechanisms are compensatory at first, but later lead to glomerular damage Global sclerosis – ischemic injury to the nephrons causes death Focal segmental sclerosis – glomerular enlargement for compensation of the loss of nephrons in other areas of the kidney. Interstitial nephritis: o The vascular and glomerular disease lead to tubular atrophy and an intense chronic interstitial nephritis The intense chronic interstitial nephritis is thought be secondary to immunologic processes against ischemia-mediated antigen changes on the tubular epithelial cell surface. Chronically these changes lead to tubular and glomerular loss causing nephrons loss. o With the death of some nephrons, less are available to maintain the GFR. o Gradual decline in the GFR is noticed as the nephrons continue to die. DIABETES –DIABETIC NEPHROPATHY: Majority of the literature in the area is applied to the diabetic nephropathy patients based on data hypothesized from the findings in animal models. Chronic hyperglycemia thought to be the primary cause of diabetic nephropathy. o Unlike other tissues of the body, transmembrane glucose transporters (GLUT) receptors do not facilitate intracellular glucose transport in the kidneys. o This effect is mediated via a number of mechanisms including: (i) glomerular hyperfiltration, (ii) direct effects of hyperglycemia, and (iii) advanced glycosylation end products (AGE), and (iv) cytokine secretion. Glomerular hyperfiltration: o Glomerular hyperfiltration is mediated mainly via dilatation the afferent arteriole leading to a rise in the GFR and the renal blood flow. o This dilatation of the afferent arteriole is mediated by a number of mechanisms in diabetic nephropathy: Hyperglycemia and high insulin-like growth factor-1 (IGF-1) concentrations (observed in diabetic patients) – both are hypothesized to cause a rise in the GFR increasing renal flow Hyperfiltration of glucose leads to augmented sodium-glucose transport in the proximal convoluted tubule causing enhanced sodium transport Cause expansion of blood volume which leads to a rise in GFR The rise in proximal reabsorption also leads to a reduced distal fluid delivery which activates the tubule-glomerular feedback with the renin-angiotensin system which works to raise the GFR as well. Hyperglycemia and AGE: o Hyperglycemia and AGE directly induce mesangial matrix production, cellular expansion and apoptosis.
- 3. o The two have also been shown to increase basement membrane permeability to albumin. Cytokines: o Elevations in vascular endothelial growth factor (VEGF), transforming growth factor beta (TFG- β), and profibrotic proteins increase damage to the nephrons at different levels; specific mechanisms are unclear.
- 4. GLOMERULONEPHRITIS Glomerular injury takes place via inflammatory as well as non-inflammatory mechanisms in different types of glomerulonephritides. Non-inflammatory injury: o Common examples of this include the podocytopathies; minimal change nephrotic syndrome/focal segmental glomerulosclerosis (MCNS/FSGS) and membranous nephropathy(MN) A dramatic rise in the glomerular permeability without any evidence of inflammation on light microscopy. Several cytokines such as IL-13 and members of the complement system C3, C5b-9 lead to glomerular basement membrane thickening, as well as podocyte damage, apoptosis, detachment and excretion in the urine. This induces glomerular sclerosis. Inflammatory injury: o Common examples include post-streptococcal glomerulonephritis (GN), membranoproliferative GN, Henoch-Schönlein purpura (HSP), systemic lupus erythematosus (SLE), some forms of rapidly progressive glomerulonephritis (RPGN), IgA nephropathy, hemolytic uremic syndrome (HUS) and various vasculitides. o This inflammatory injury has been found to be mediated by a number of mechanisms: Some members of the complement system such as C5a have been implicated in inflammatory injury via inducing antibody deposition and activation and recruitment of polymorphonuclear cells (PMNs); neutrophil, macrophage/monocyte, platelets and T-cells. These cells produce oxidants and proteases that cause fibrin deposition, capillary wall damage and produce proteinuria. Unlike podocyte targeting in non-inflammatory injury, disorders in which glomerular endothelial and mesangial cells are principally involved exhibit a more dramatic response to immune injury. This response is usually characterized by cell proliferation and phenotype change, as well as readily visible structural changes in the renal biopsy. Post-Renal CKD: See Urology. PATHOPHYSIOLOGY Patients with stages 1-3 ([GFR] >30 mL/min) of CKD are generally asymptomatic; water/electrolyte imbalances or endocrine/metabolic derangements are not clinically evident. These disturbances manifest clinically in CKD stages 4-5 (GFR < 30 mL/min). Sign/lab finding Symptoms Mechanism Generalized edema Swelling Water retention due to a loss of GFR leading to sodium and fluid retention. Fluid moves into the extravascular space, due to increased hydrostatic pressure, causing pitting edema in the lower extremity (fluid movement could also be due to hypoalbuminemia, in some diseases, leading to a low oncotic pressure).
- 5. Pulmonary crackles Shortness of breath Fluid accumulation causes pulmonary edema and loss of air space causing ventilation-perfusion mismatch. This leaves less area for oxygen diffusion form the blood vessels. Anemia Fatigue, reduced exercise capacity, and pallor Erythropoietin (EPO), the major erythropoiesis stimulator, is released from the kidneys; with renal failure, there is loss of EPO release. Weight loss Loss of lean body mass Protein-energy malnutrition due to metabolic acidosis. Loss of kidney function results in impaired H+ secretion from the body. Hyperkalemia Malaise, palpitations Inability of the kidneys to secrete potassium in the urine leads to life threatening arrhythmias. Mechanisms of renal osteodystrophy Hyperphosphatemia Damaged kidneys fail to excrete phosphate. Also secondary to high parathyroid hormone levels. Hypocalcemia Thought to be secondary to low Vitamin D3 levels. In early stages of CKD, low levels of calcitriol are due to hyperphosphatemia (negative feedback). In the later stages of CKD, low levels are hypothesized to be due to decreased synthesis of 1α-hydroxylase (enzyme that converts calcifediol to calcitriol in the kidneys). Secondary and tertiary hyperparathyroidism To compensate for the low calcium due to low Vitamin D levels, the parathyroid glands increase the parathyroid hormone secretion. This leads to a high bone turnover, always attempting to normalize the low calcium levels in the blood. Over time, this becomes maladaptive leading to extraosseous calcification, and parathyroid hyperplasia develops (tertiary hyperparathyroidism). Complications of uremia Urea and other toxins accumulate in the blood and cause life threatening issues. Ecchymosis, GI bleeding Increased tendency to bleed and ecchymosis Uremia-induced platelet dysfunction Pericardial friction rub Chest pain, malaise Uremic pericarditis Headaches, confusion, coma Uremic encephalopathy; adverse effects of urea on the CNS. Mechanisms unclear.
- 6. TREATMENT: Cardiovascular disease (CVD)is the leading cause of death in patients with CKD. o Reducing risk factors for development of CVD is beneficial. E.g. treatment of hyperlipidemia, lifestyle and dietary changes Tight blood pressure control: o Reducing damage due to the end organ effects of hypertension on the kidney as well as the heart. o Angiotensin-converting enzyme inhibitors (ACEI) and angiotensin II receptor blockers(ARBs) block the effects of angiotensin II on (i) sodium and fluid retention, (ii) vasoconstriction, (iii) stimulating ADH release, (iv) stimulating aldosterone release, and (v) inducing a sympathetic response. ACEIs and ARBs also slow down progression of proteinuria in patients with diabetic CKD. Diabetes management: o Tight glucose management slows the progression of vascular and heart disease. Avoidance of IV contrast, NSAIDs, and nephrotoxic drugs: o These agents can potentially induce an acute kidney injury (AKI) on the underlying kidney disease and therefore exacerbate the baseline CKD. Diet: o Mixed evidence exists whether dietary protein restriction is beneficial in slowing disease progression. o Proteins affect the renal hemodynamics, raising the GFR, in hypothesized 2 ways. Hormonal effects – proteins cause secretion of glucagon, IGF-1 and kinins, all of which have been shown to raise the GFR. Tubuloglomerular effects – high amino acid (AA) filtration leads to increased AA and hence the sodium uptake in the proximal convoluted tubule. A decreased sodium delivery to the distal convoluted tubule leads to the rennin-angiotensin system
- 7. activation via the macula densa and these work to raise the GFR (mechanisms above) o Controlling hyperphosphatemia: Protein restriction also limits phosphorus consumption. Hyperphosphatemia plays a major role in the progression of renal osteodystrophy. Phosphate binders are used to reduce phosphate absorption through the GI tract.
