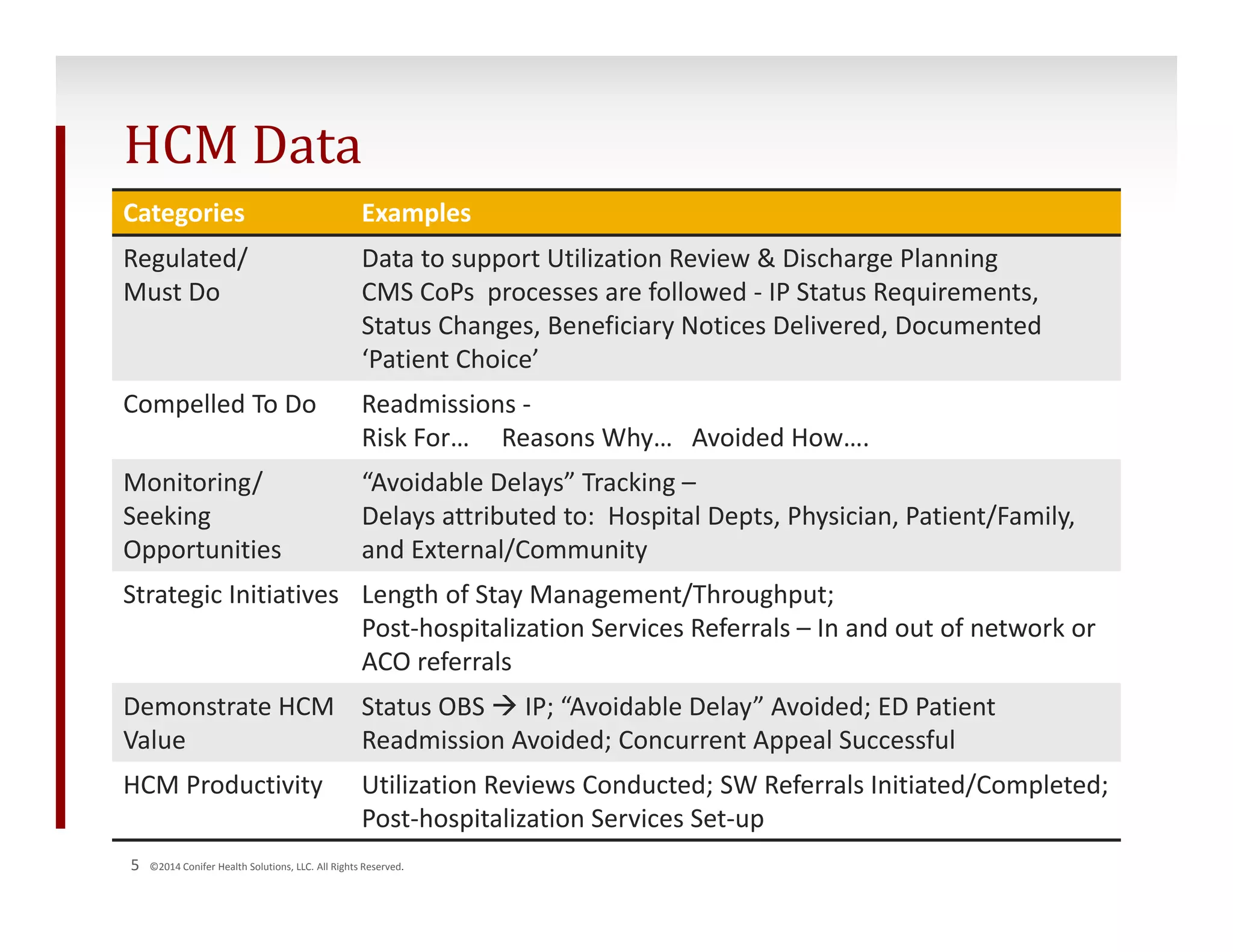
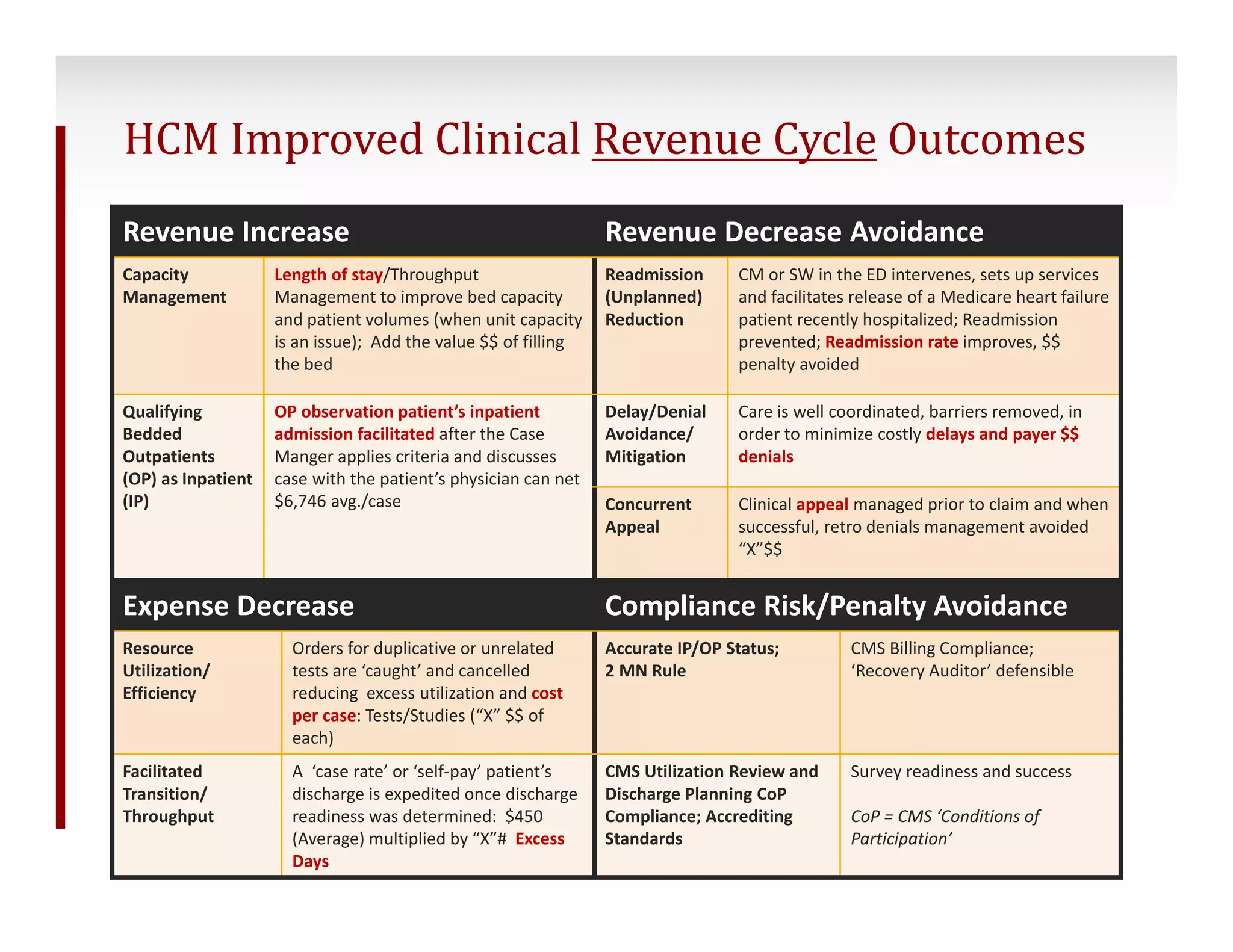
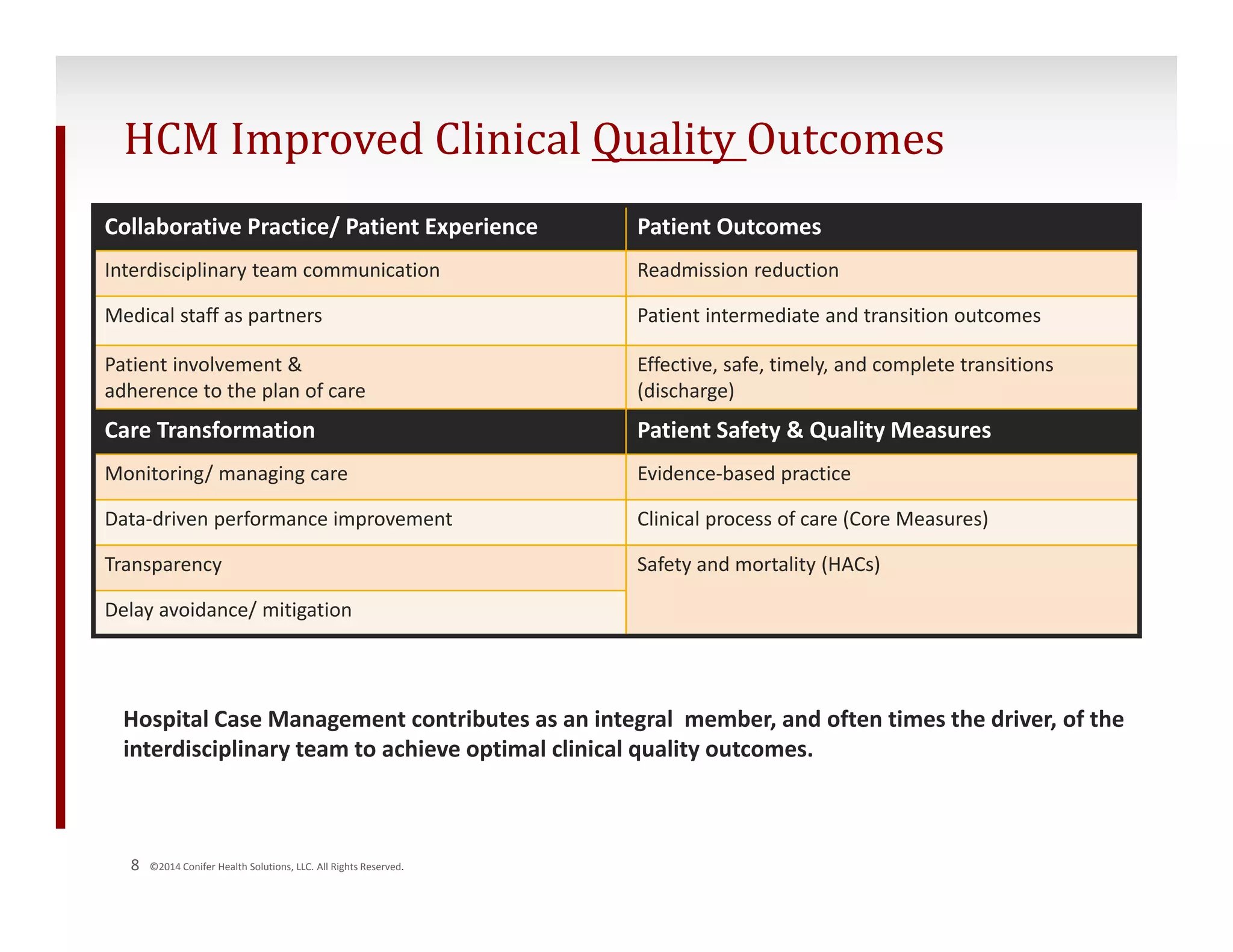
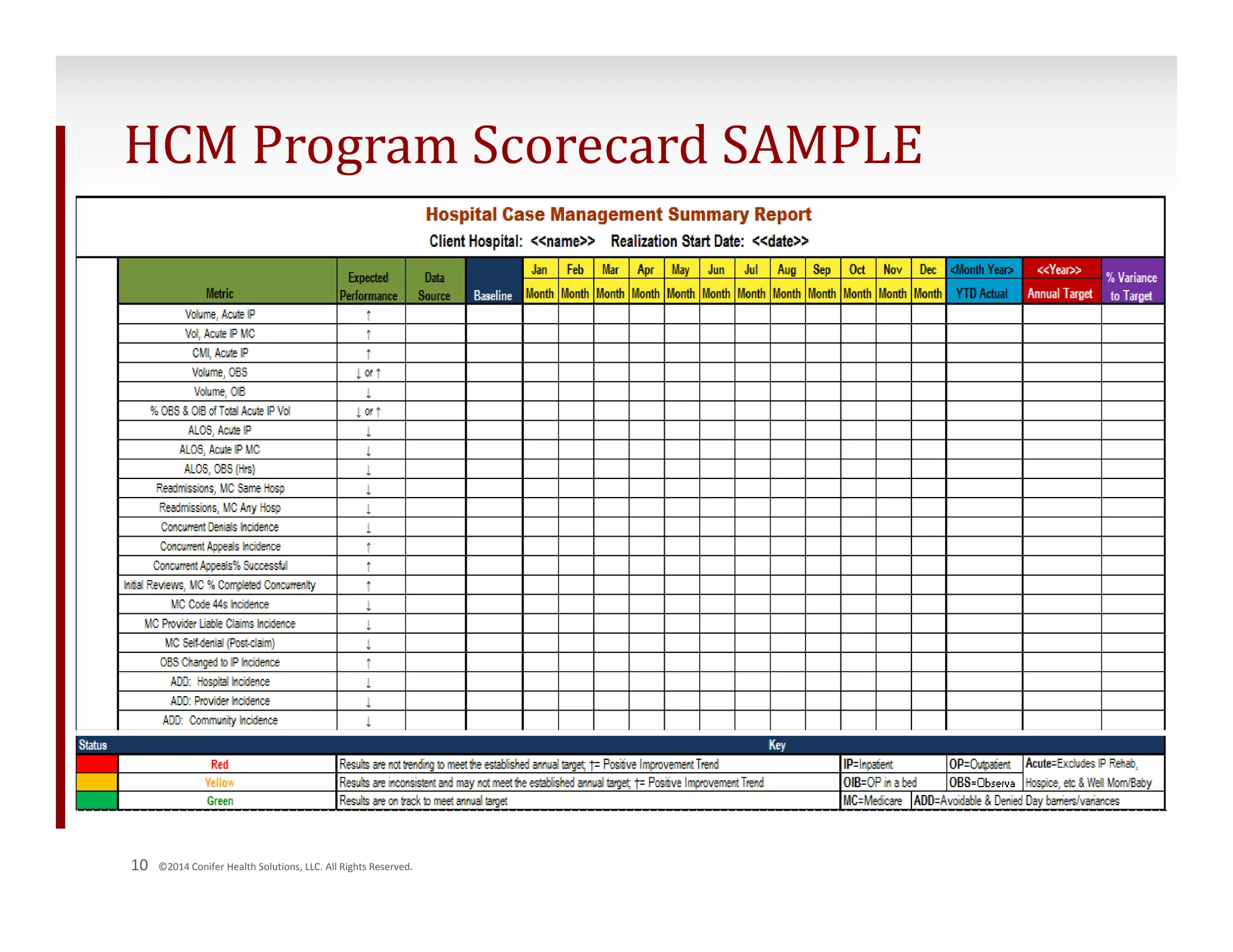
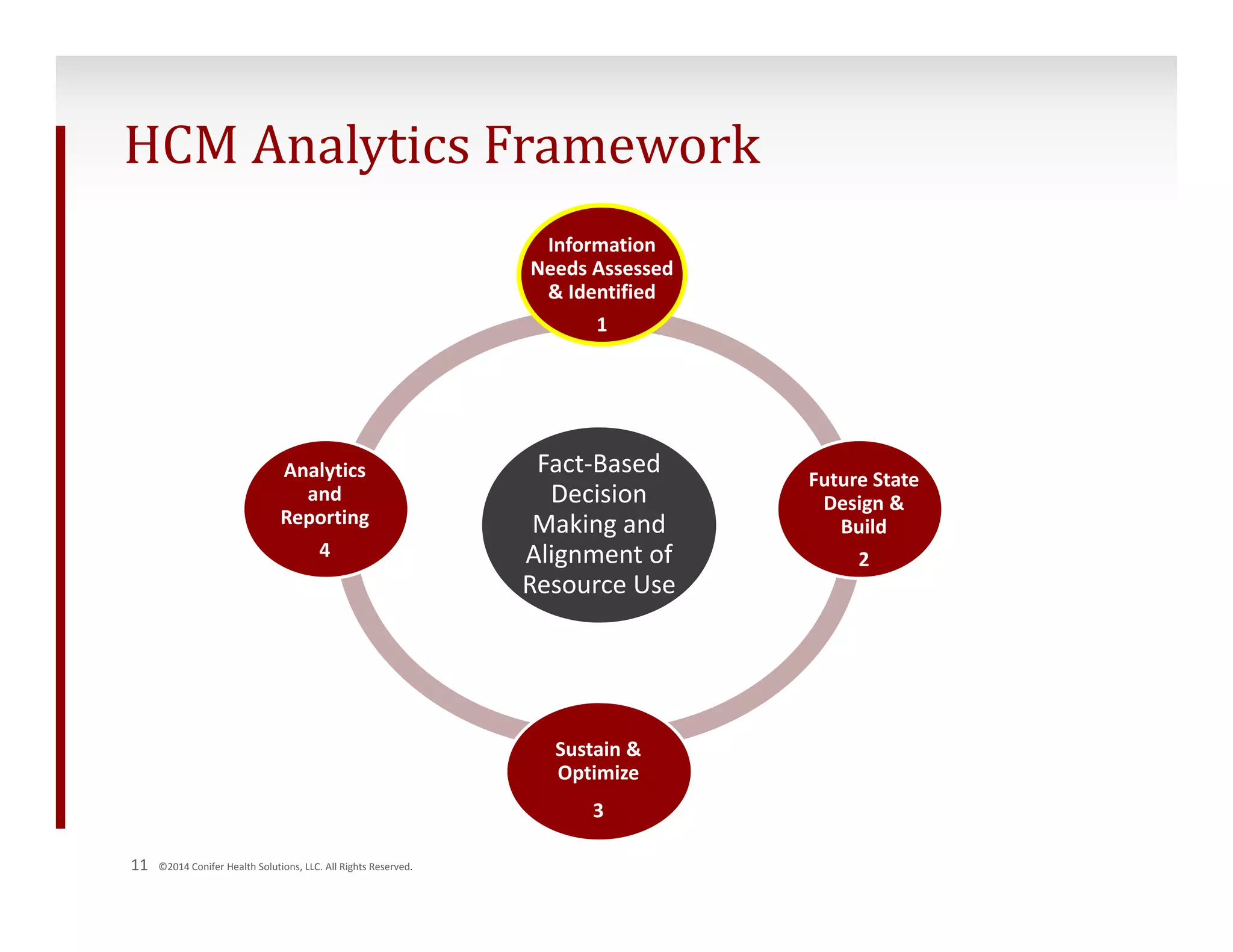
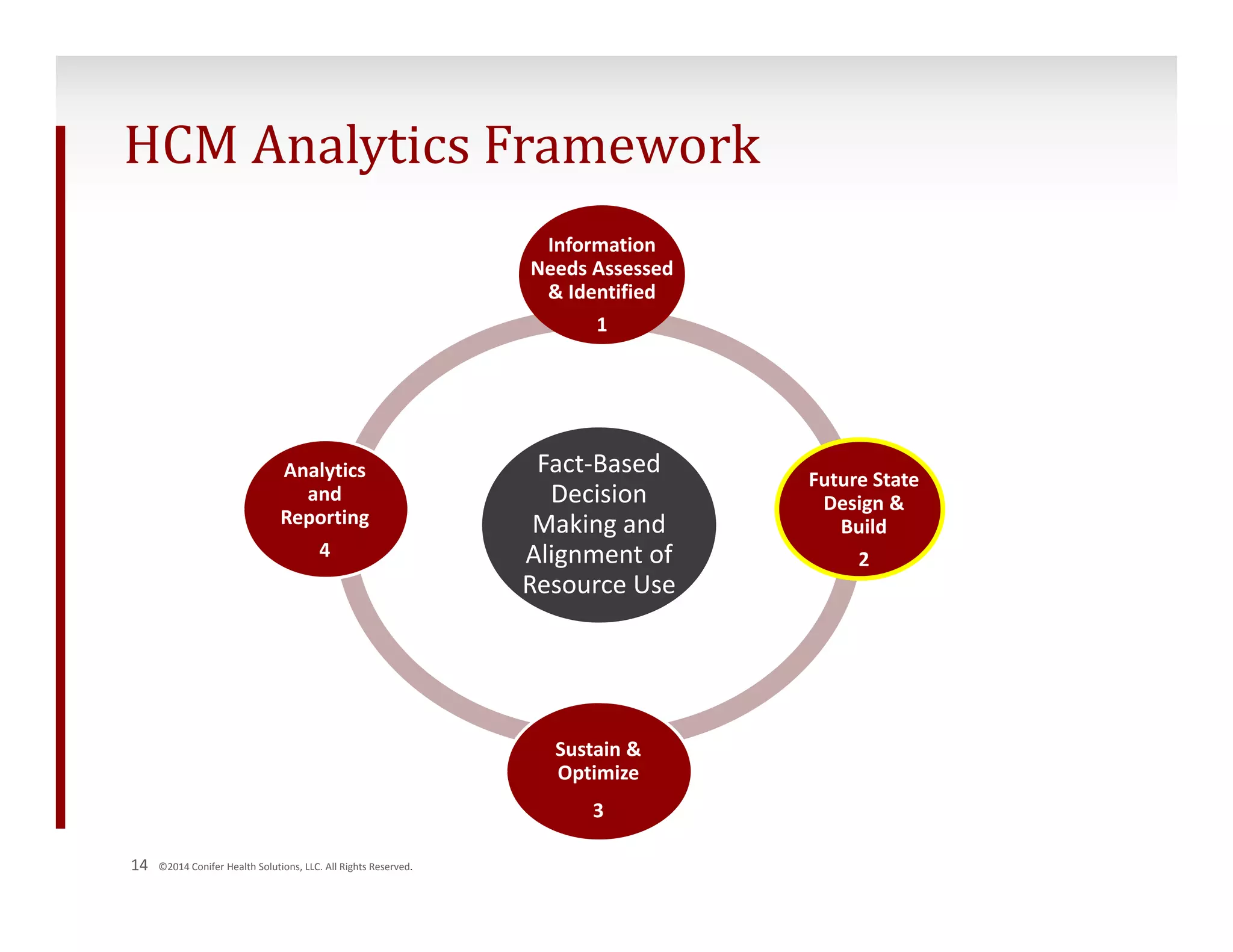
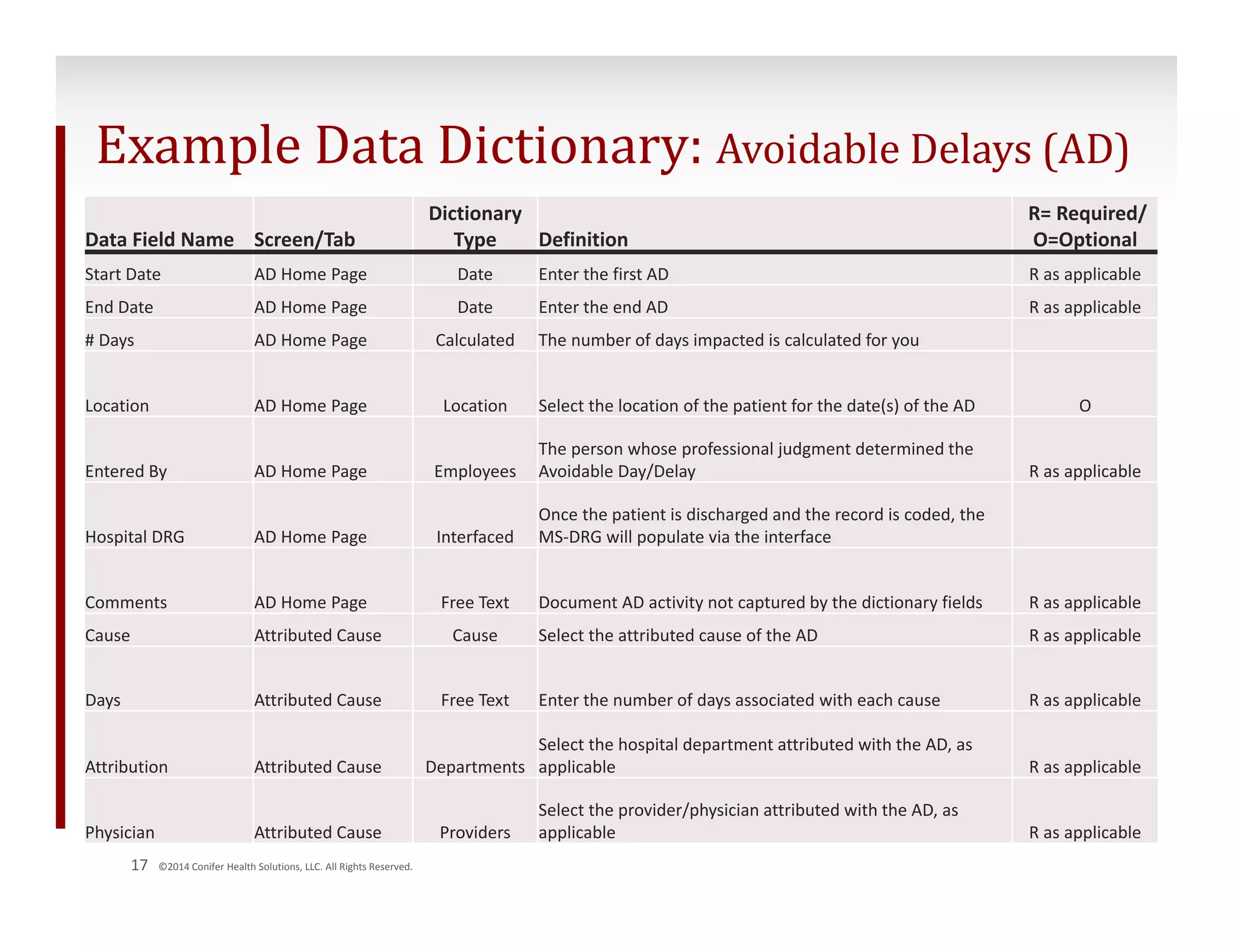
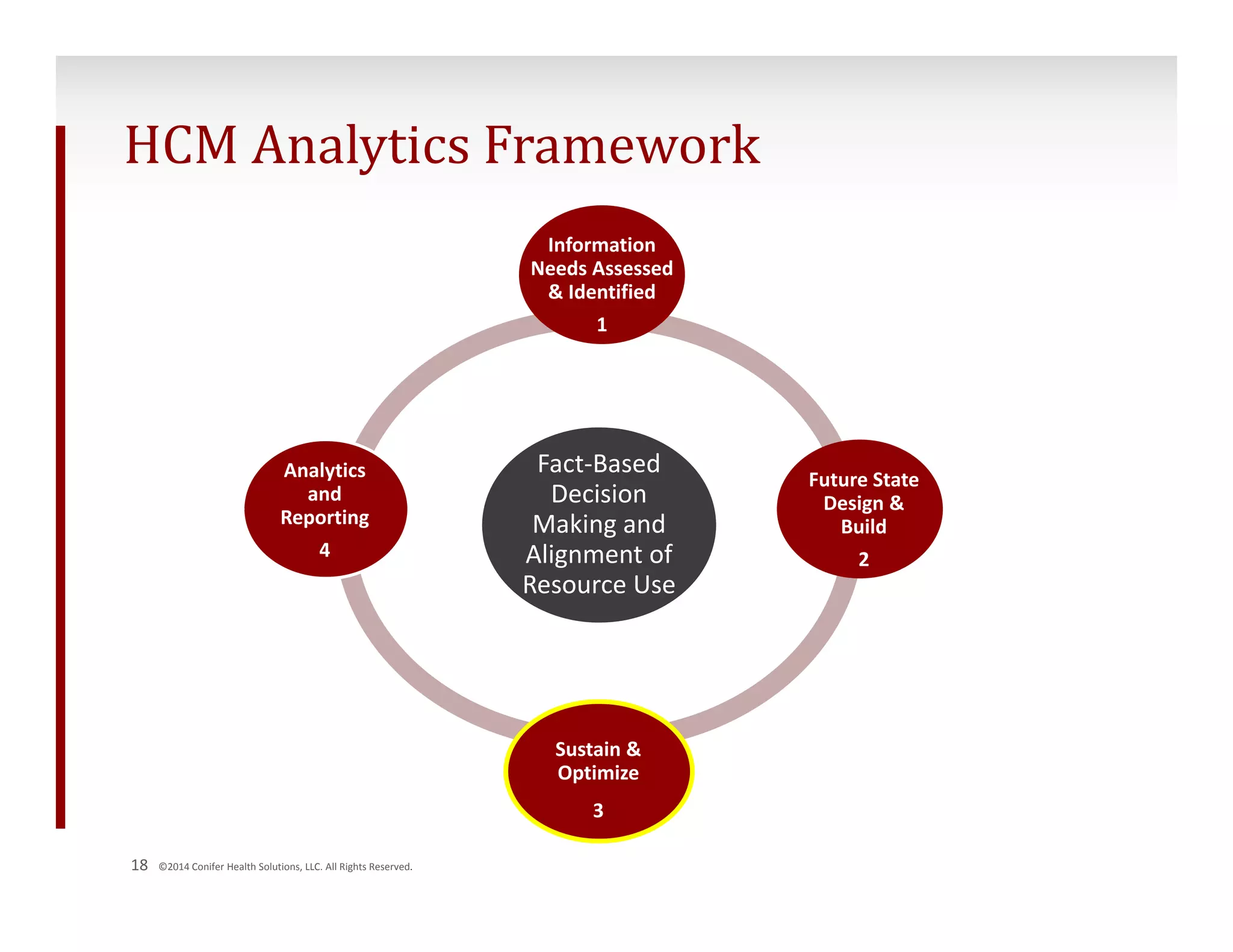
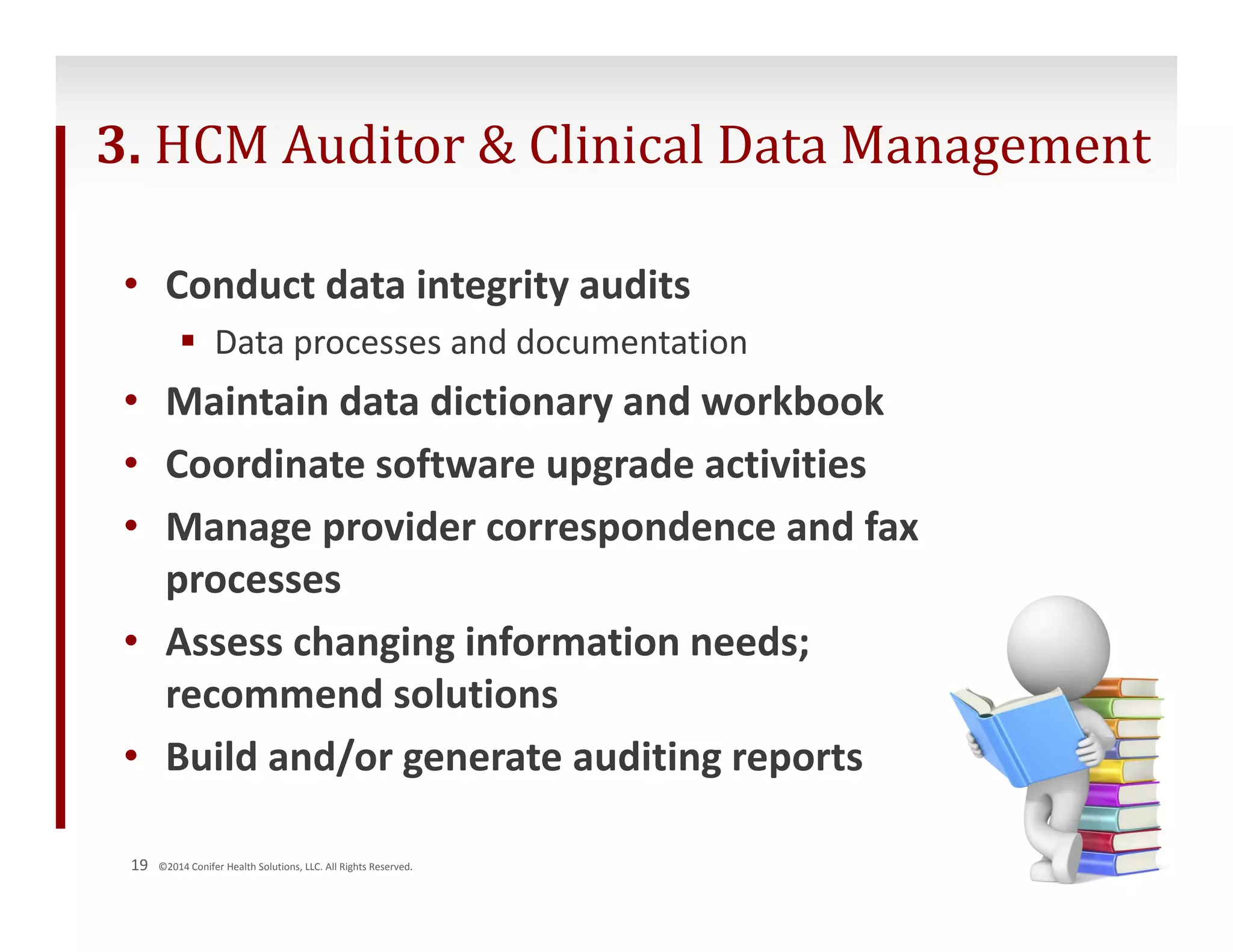
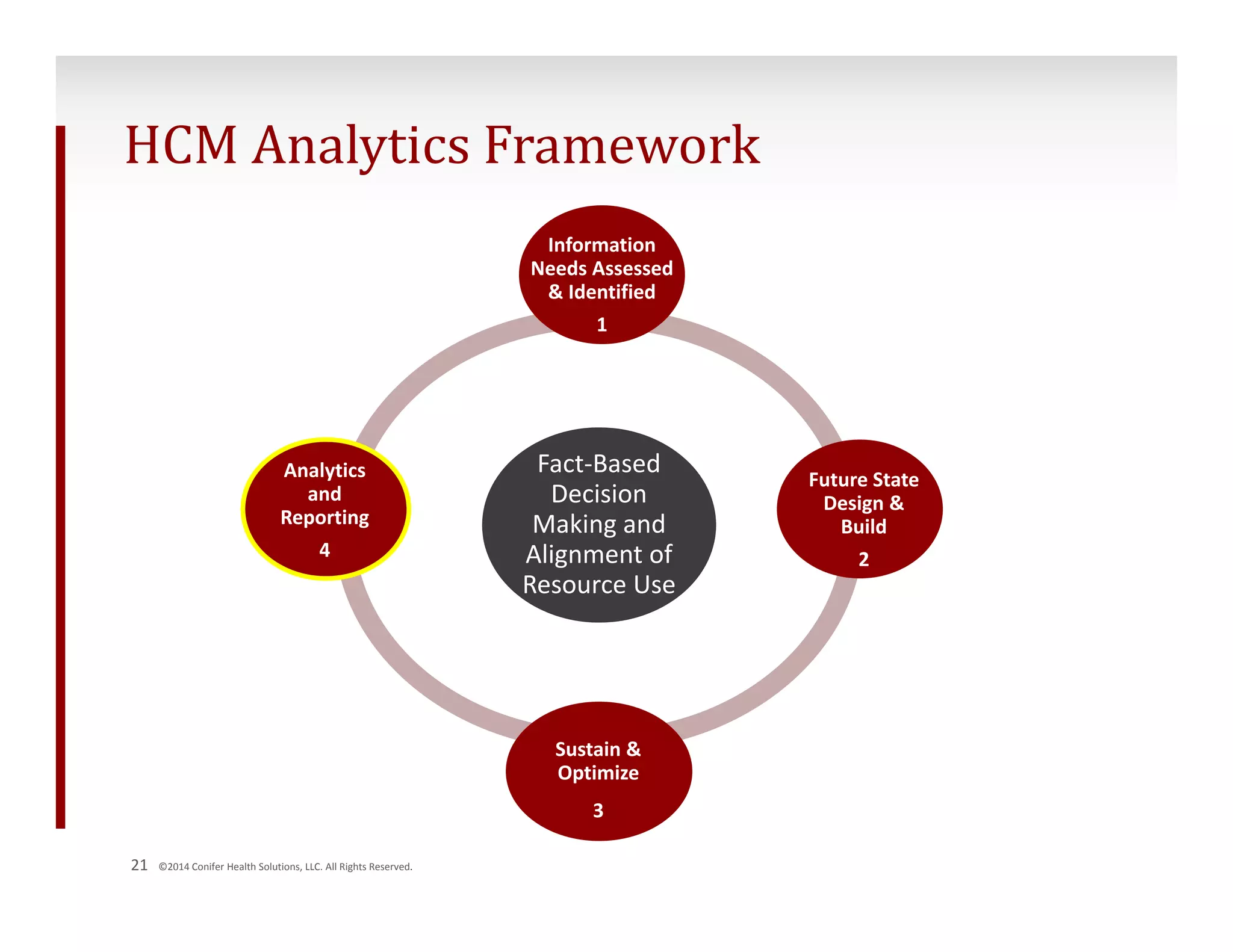
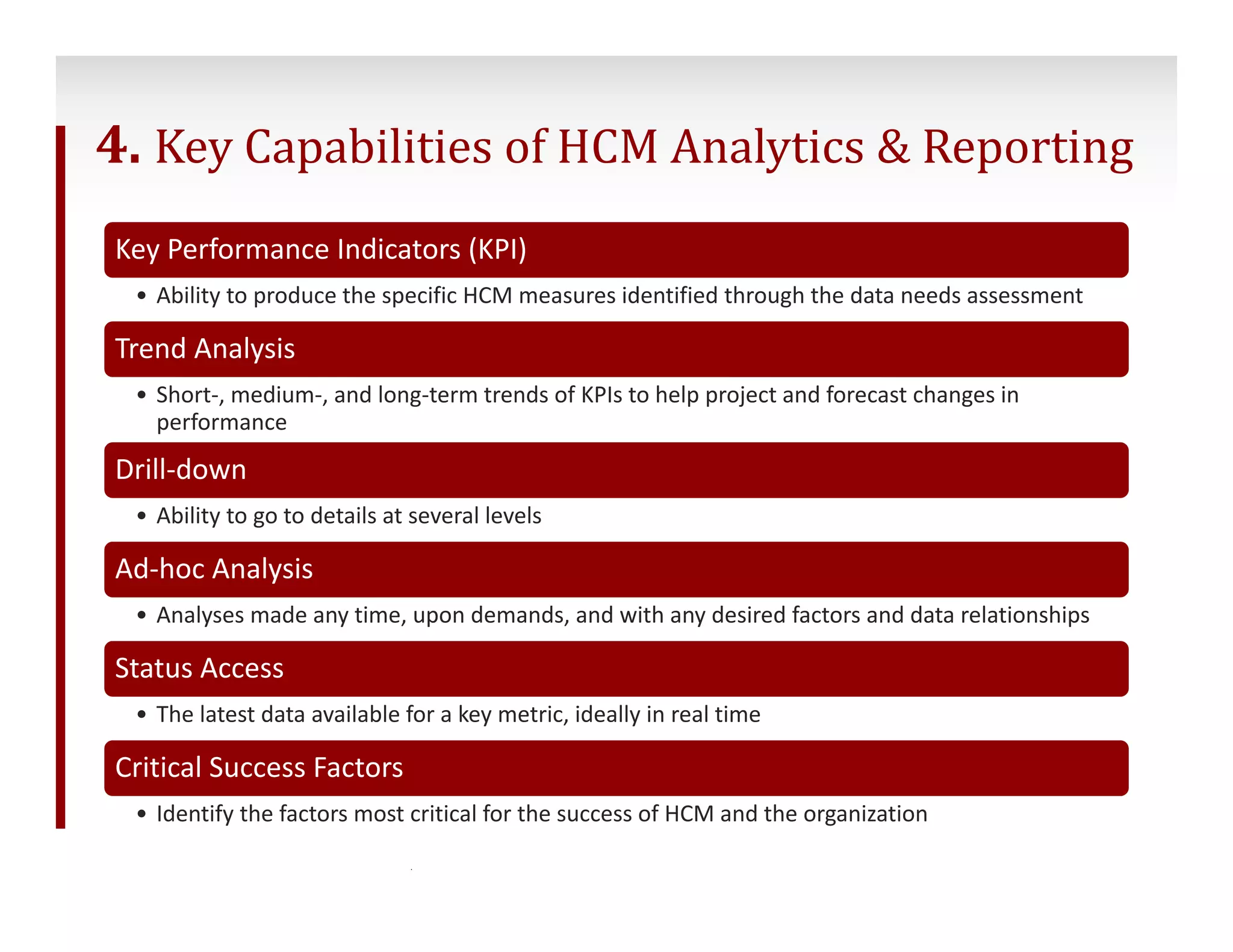
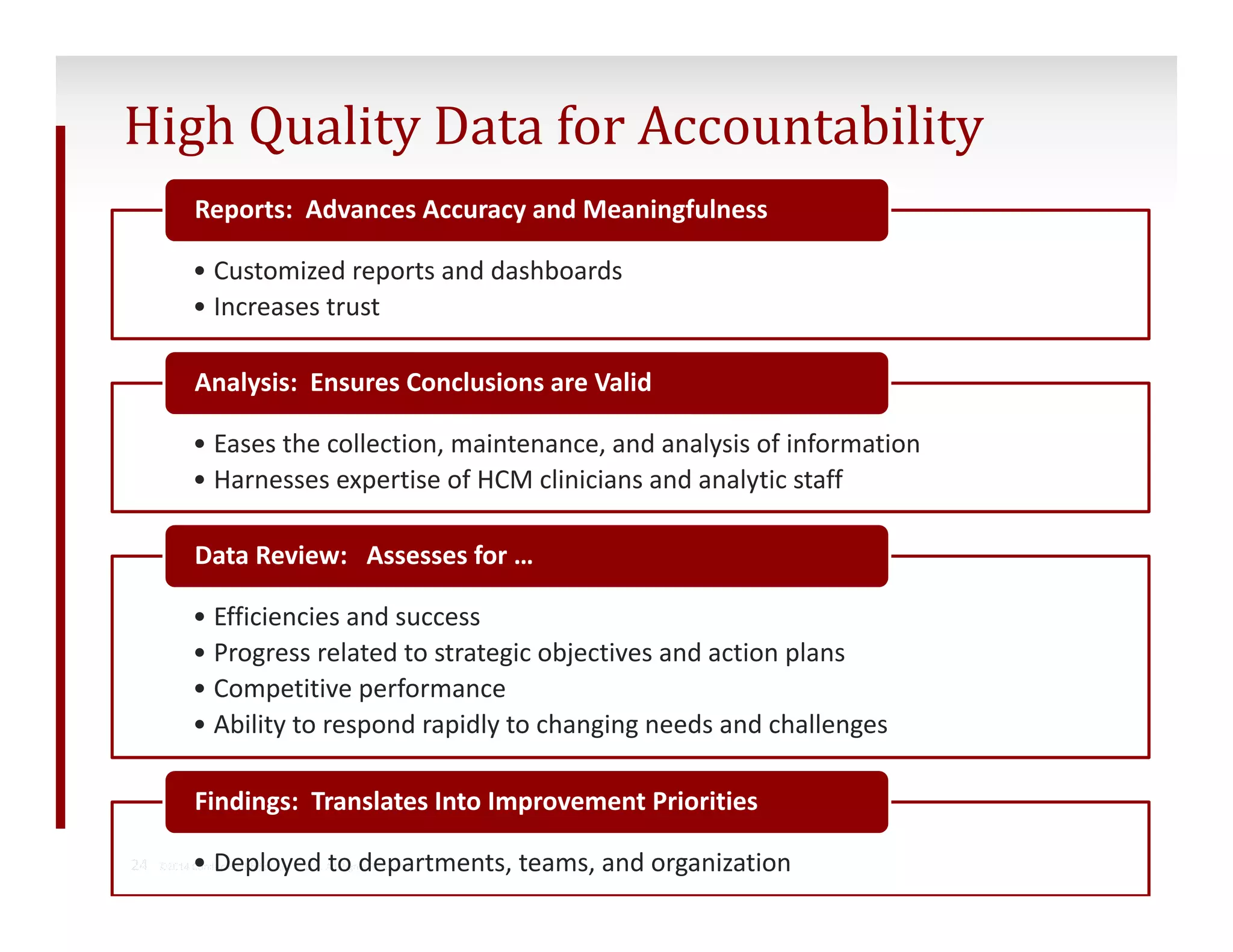
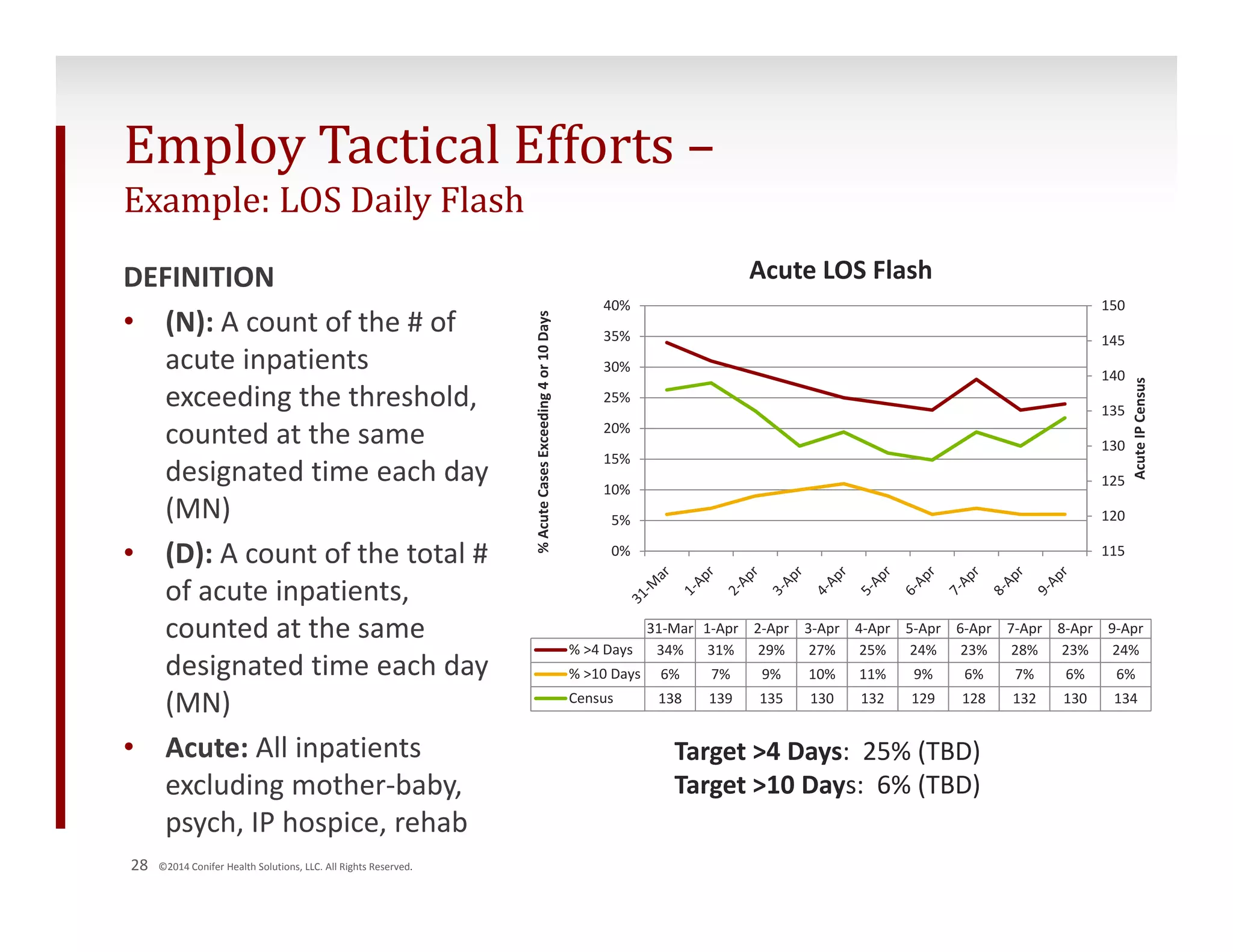
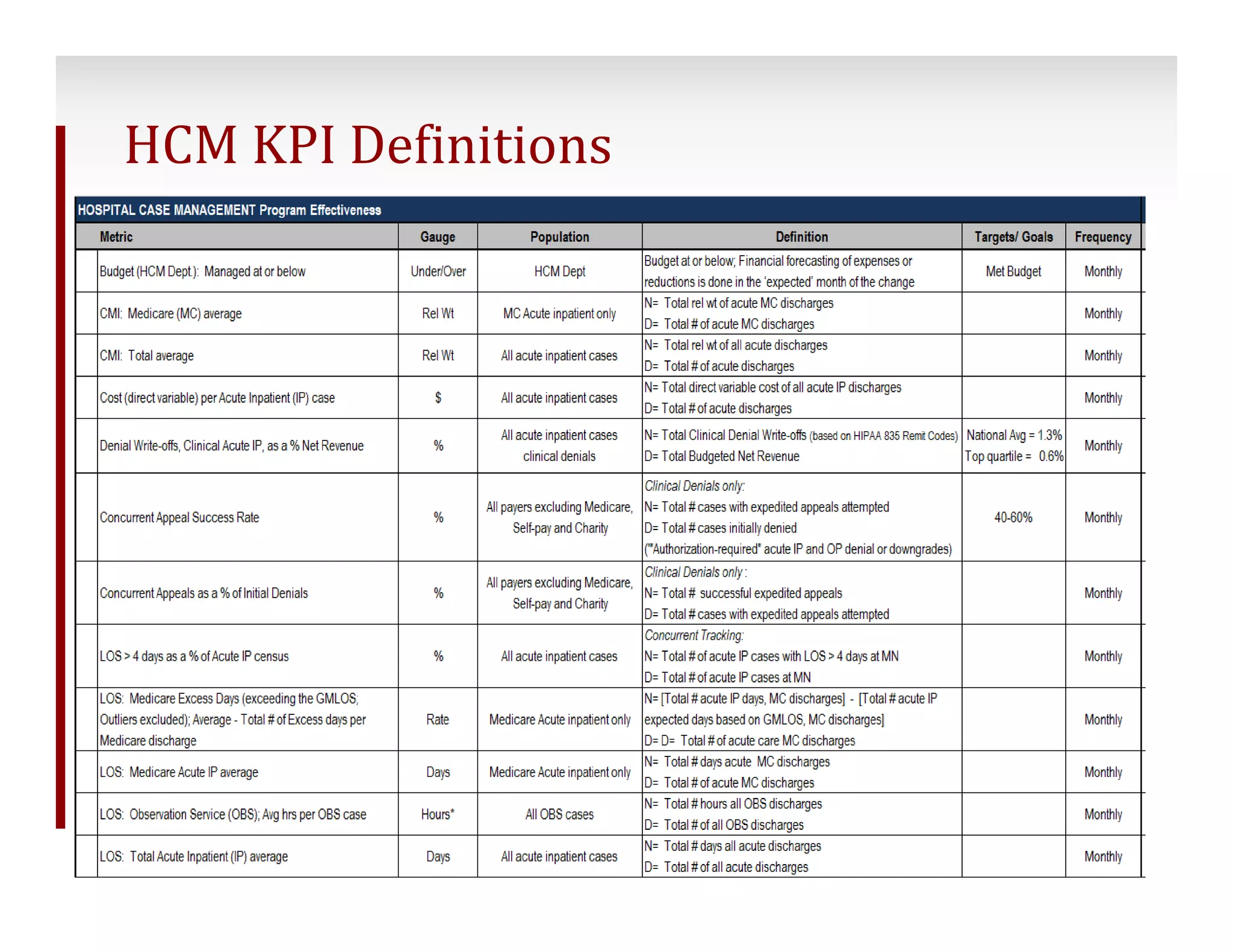
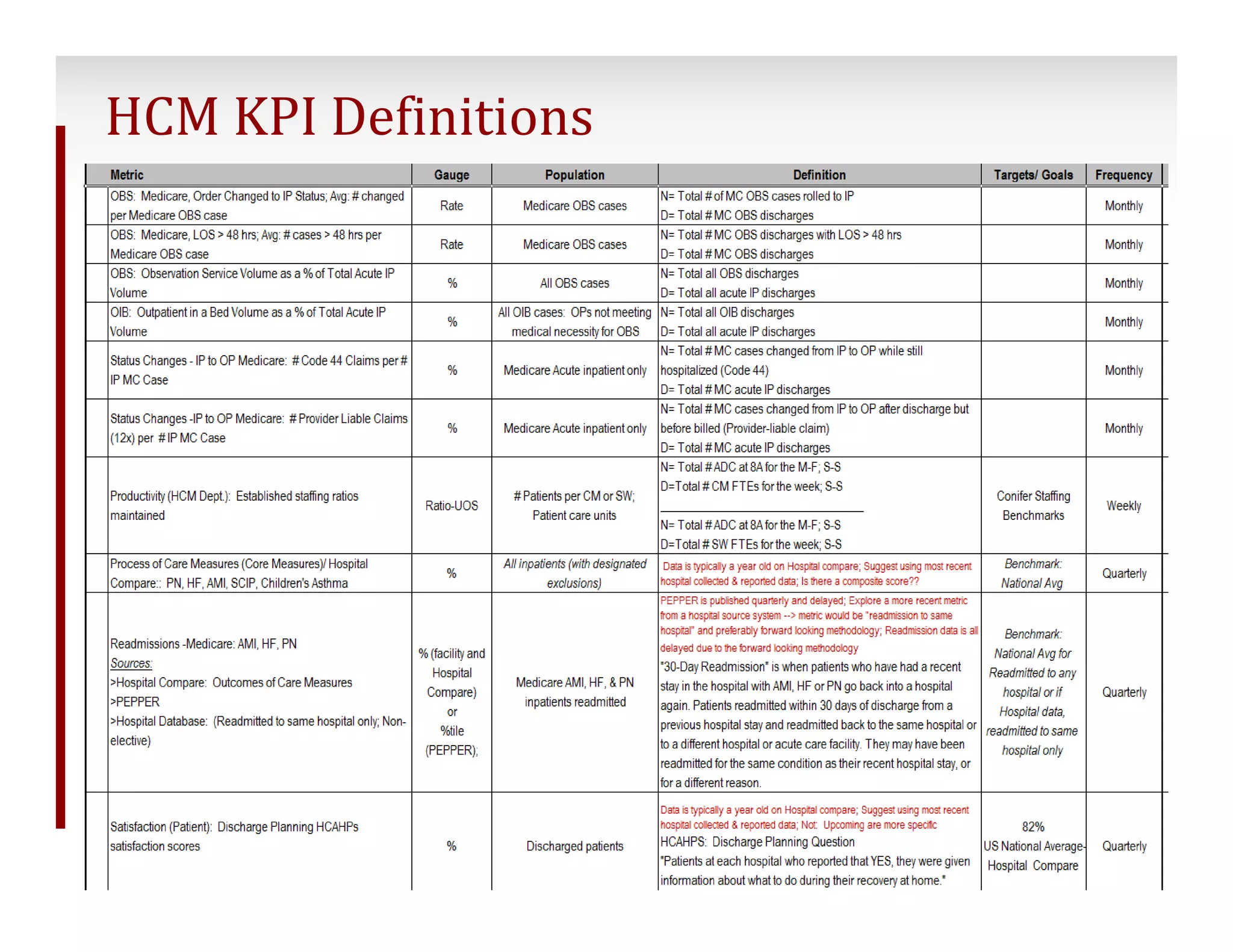
The document discusses strategies for hospitals to create data-driven case management programs. It outlines a framework for hospitals to assess data needs, design analytics reporting, and use data to improve outcomes. The framework includes 4 steps: 1) assessing information needs, 2) designing future reporting structures, 3) sustaining data management and auditing, and 4) developing analytics and reporting capabilities. Key goals are providing the right data to stakeholders, enhancing decision-making, and using metrics to influence performance.