This document discusses chronic inflammation and wound healing. It provides details on:
1. The general features of chronic inflammation including infiltration of inflammatory cells and tissue destruction through macrophage activation.
2. The systemic effects of chronic inflammation such as anemia, fever, and amyloidosis.
3. The types of chronic inflammation including non-specific and granulomatous inflammation, and describes granulomas and their composition.
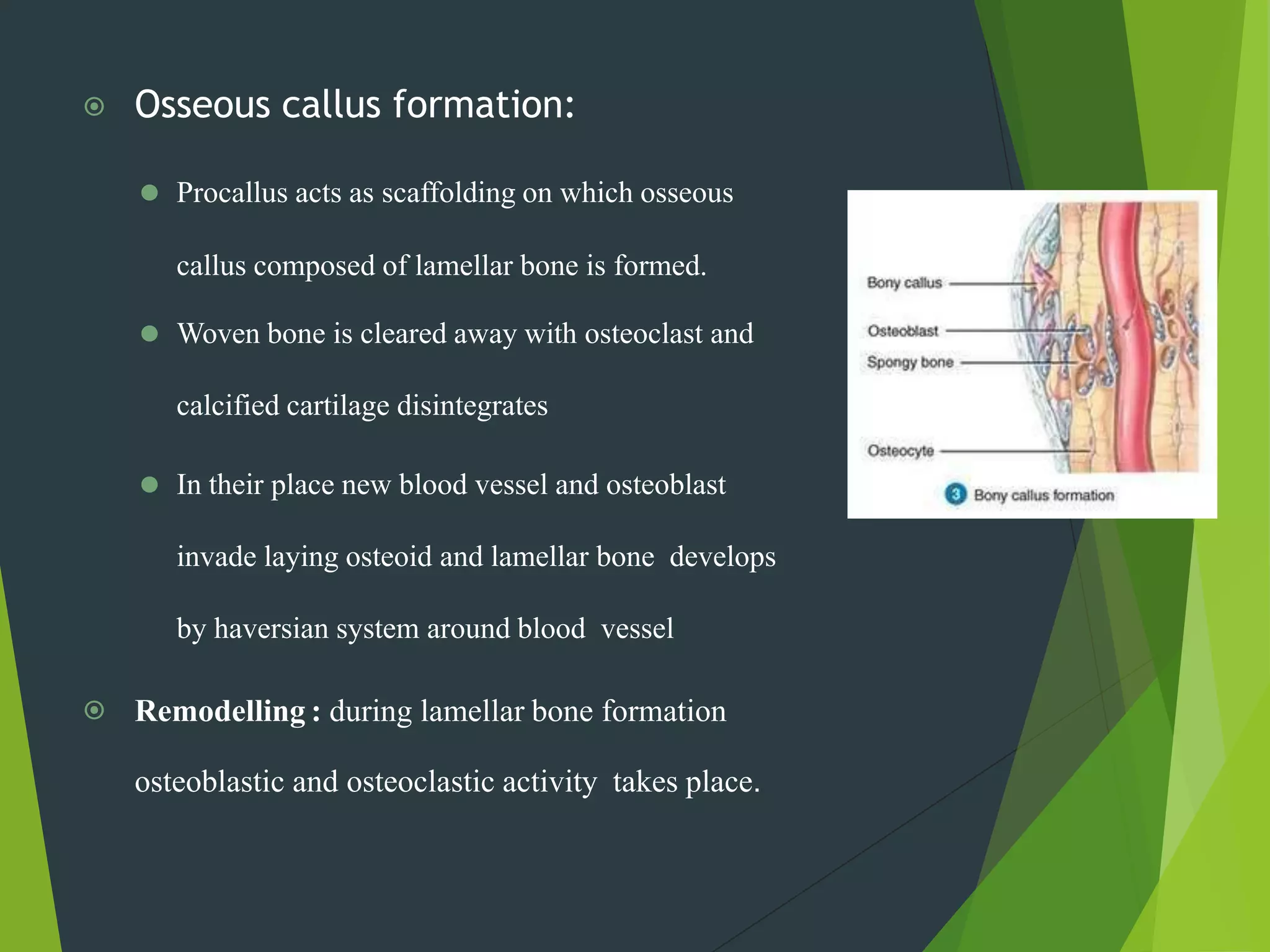
4. The process of wound healing including regeneration, repair through granulation tissue formation and wound contraction. It also discusses healing of special tissues like fractures.